Congenital Central Hypoventilation Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Core Transcriptional Regulatory Circuitries in Cancer
Oncogene (2020) 39:6633–6646 https://doi.org/10.1038/s41388-020-01459-w REVIEW ARTICLE Core transcriptional regulatory circuitries in cancer 1 1,2,3 1 2 1,4,5 Ye Chen ● Liang Xu ● Ruby Yu-Tong Lin ● Markus Müschen ● H. Phillip Koeffler Received: 14 June 2020 / Revised: 30 August 2020 / Accepted: 4 September 2020 / Published online: 17 September 2020 © The Author(s) 2020. This article is published with open access Abstract Transcription factors (TFs) coordinate the on-and-off states of gene expression typically in a combinatorial fashion. Studies from embryonic stem cells and other cell types have revealed that a clique of self-regulated core TFs control cell identity and cell state. These core TFs form interconnected feed-forward transcriptional loops to establish and reinforce the cell-type- specific gene-expression program; the ensemble of core TFs and their regulatory loops constitutes core transcriptional regulatory circuitry (CRC). Here, we summarize recent progress in computational reconstitution and biologic exploration of CRCs across various human malignancies, and consolidate the strategy and methodology for CRC discovery. We also discuss the genetic basis and therapeutic vulnerability of CRC, and highlight new frontiers and future efforts for the study of CRC in cancer. Knowledge of CRC in cancer is fundamental to understanding cancer-specific transcriptional addiction, and should provide important insight to both pathobiology and therapeutics. 1234567890();,: 1234567890();,: Introduction genes. Till now, one critical goal in biology remains to understand the composition and hierarchy of transcriptional Transcriptional regulation is one of the fundamental mole- regulatory network in each specified cell type/lineage. -

Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

SOX11 Interactome Analysis: Implication in Transcriptional Control and Neurogenesis
SOX11 interactome analysis: Implication in transcriptional control and neurogenesis Dissertation der Mathematisch-Naturwissenschaftlichen Fakultät der Eberhard Karls Universität Tübingen zur Erlangung des Grades eines Doktors der Naturwissenschaften (Dr. rer. nat.) vorgelegt von Birgit Heim, geb.Kick aus Augsburg Tübingen 2014 Gedruckt mit Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Eberhard Karls Universität Tübingen. Tag der mündlichen Qualifikation: 12.02.2015 Dekan: Prof. Dr. Wolfgang Rosenstiel 1. Berichterstatter: Prof. Dr. Olaf Rieß 2. Berichterstatter: Prof. Dr. Marius Ueffing Für meine Familie TABLE OF CONTENTS Table of contents Summary ................................................................................................................ 5 Zusammenfassung ............................................................................................... 7 1. Introduction ...................................................................................... 9 1.1. Adult neurogenesis .................................................................................... 9 1.1.1. Adult neural stem cells and neuronal precursor cells ............................ 9 1.1.2. Neurogenic niches .............................................................................. 11 1.1.3. Regulation of adult neurogenesis ........................................................ 12 1.1.3.1. Extrinsic mechanisms .................................................................. 12 1.1.3.2. Intrinsic mechanisms .................................................................. -

Phox2b and Motoneuronal Differentiation
Development 127, 1349-1358 (2000) 1349 Printed in Great Britain © The Company of Biologists Limited 2000 DEV1515 Control of hindbrain motor neuron differentiation by the homeobox gene Phox2b Alexandre Pattyn, Marie-Rose Hirsch, Christo Goridis and Jean-François Brunet* Laboratoire de Génétique et Physiologie du Développement, Developmental Biology Institute of Marseille, CNRS/INSERM/Univ Méditerranée/AP de Marseille, Luminy Case 907, 13288 Marseille Cedex 9, France *Author for correspondence (e-mail: [email protected]) Accepted 11 January; published on WWW 7 March 2000 SUMMARY Motor neurons are a widely studied model of vertebrate both the generic and subtype-specific programs of neurogenesis. They can be subdivided in somatic, branchial motoneuronal differentiation are disrupted at an early and visceral motor neurons. Recent studies on the stage. Most motor neuron precursors die inside the dorsoventral patterning of the rhombencephalon have neuroepithelium while those that emigrate to the mantle implicated the homeobox genes Pax6 and Nkx2.2 in the layer fail to switch on early postmitotic markers and to early divergence of the transcriptional programme of downregulate neuroepithelial markers. Thus, the loss of hindbrain somatic and visceral motor neuronal function of Phox2b in hindbrain motor neurons exemplifies differentiation. We provide genetic evidence that the a novel control point in the generation of CNS neurons. paired-like homeodomain protein Phox2b is required for the formation of all branchial and visceral, but not somatic, Key words: Neurogenesis, Motor neuron, Homeobox gene, motor neurons in the hindbrain. In mice lacking Phox2b, Rhombencephalon, Phox2b, Mouse INTRODUCTION of sm neurons has been studied most extensively and some of the transcriptional cascades controlling their differentiation are The specification of neuronal subtype identity in the beginning to be understood. -

The Evolving Genetic Landscape of Hirschprung Disease: an Update and Review
Review Article Clinics in Surgery Published: 11 Oct, 2017 The Evolving Genetic Landscape of Hirschprung Disease: An Update and Review Amit Kumar Yadav* and Gaurav Chopra Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India Abstract Hirschsprung Disease (HD) is a developmental disorder characterized by the complete absence of ganglion cells in the distal gastrointestinal tract. It is the most common cause of functional intestinal obstruction in neonates and children. The aganglionosis is believed to be either due to failure of neural crest cells to migrate, proliferate, differentiate or survive during gut development in the embryonic stage. The incidence of HD is estimated at 1/5000 live births and shows a male predominance. It is usually sporadic, although it can be familial and may be inherited as autosomal dominant or autosomal recessive. In 70% of cases, HD occurs as an isolated trait and in the other 30% it is associated with other congenital malformation syndromes. HD has a complex multifactorial etiology, and genetic factors play a key role in its pathogenesis. Several gene loci appear to be involved. Many of these have been identified by conducting Genome Wide Association (GWAS) studies and recently by Next Generation Sequencing (NGS). These genes encode for receptors, ligands (especially those participating in the RET, EDNRB and Semaphorin signaling pathways), transcriptional factors (PHOX2B & SOX10). These genes are involved in the neural crest cell development and migration that give rise to ganglion cells. Overall, the RET proto-oncogene is considered the major disease causing gene in HD. A greater understanding of the genetic landscape of this disease might pave way for genetic counseling, prenatal and preimplantation diagnosis in the management of HD. -

HAND2 Synergistically Enhances Transcription of Dopamine-ß
Available online at www.sciencedirect.com R Developmental Biology 262 (2003) 183–193 www.elsevier.com/locate/ydbio HAND2 synergistically enhances transcription of dopamine-- hydroxylase in the presence of Phox2a Haiming Xu,a Anthony B. Firulli,b Xiaotong Zhang,a and Marthe J. Howarda,* a Department of Anatomy and Neurobiology, Medical College of Ohio, 3000 Arlington Ave., Toledo, OH 43614, USA b Wells Center for Pediatric Research, James Whitcomb Riley Hospital for Children, 702 Barnhill Drive, Room 2666, Indianapolis, IN 46202-5225, USA Received for publication 28 March 2003, revised 5 June 2003, accepted 5 June 2003 Abstract Noradrenergic neuronal identity and differentiation are controlled by cascades of transcription factors acting downstream of BMP4, including the basic helix–loop–helix DNA binding protein HAND2 and the homeodomain factor Phox2a. Dopamine--hydroxylase (DBH) is the penultimate enzyme required for synthesis of norepinephrine and is thus a noradrenergic cell type-specific marker. We have examined the interaction of HAND2 and Phox2a at the DBH promoter. Using transient transfection of P19 or NT-2 cells, HAND2 is shown to synergistically enhance Phox2a-driven transcriptional activity at the DBH promoter, an effect that is enhanced by cAMP. While mutation of the Phox2a homeodomain binding sites HD1, HD2, and HD3 results in the loss of HAND2/Phox2a transactivation of DBH, it is the interaction of HAND2/Phox2a at the CRE/AP1-HD1/2 domains in the DBH enhancer that are required for synergistic activation by HAND2. We find that HAND2 functions as a transcriptional activator without directly binding to E-box sequences in the DBH promoter, suggesting that HAND2-mediated DBH activity occurs by protein–protein interactions with other transcriptional regulators. -

Defining the Transcriptomic Landscape of the Developing Enteric Nervous System and Its Cellular Environment Sweta Roy-Carson Iowa State University, [email protected]
Genetics, Development and Cell Biology Genetics, Development and Cell Biology Publications 2017 Defining the transcriptomic landscape of the developing enteric nervous system and its cellular environment Sweta Roy-Carson Iowa State University, [email protected] Kevin Natukunda Iowa State University, [email protected] Hsien-chao Chou Iowa State University Narinder Pal Iowa State University Caitlin Farris Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/gdcb_las_pubs See next page for additional authors Part of the Cell and Developmental Biology Commons, and the Molecular Genetics Commons The ompc lete bibliographic information for this item can be found at https://lib.dr.iastate.edu/ gdcb_las_pubs/202. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Genetics, Development and Cell Biology at Iowa State University Digital Repository. It has been accepted for inclusion in Genetics, Development and Cell Biology Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Defining the transcriptomic landscape of the developing enteric nervous system and its cellular environment Abstract Background: Motility and the coordination of moving food through the gastrointestinal tract rely on a complex network of neurons known as the enteric nervous system (ENS). Despite its critical function, many of the molecular mechanisms that direct the development of the ENS and the elaboration of neural network connections remain unknown. The og al of this study was to transcriptionally identify molecular pathways and candidate genes that drive specification, differentiation and the neural circuitry of specific neural progenitors, the phox2b expressing ENS cell lineage, during normal enteric nervous system development. -

REVIEW ARTICLE Pediatric Disorders with Autonomic Dysfunction: What
0031-3998/05/5801-0001 PEDIATRIC RESEARCH Vol. 58, No. 1, 2005 Copyright © 2005 International Pediatric Research Foundation, Inc. Printed in U.S.A. REVIEW ARTICLE Pediatric Disorders with Autonomic Dysfunction: What Role for PHOX2B? CLAUDE GAULTIER, HA TRANG, STÉPHANE DAUGER, AND JORGE GALLEGO INSERM U676 [C.G., S.D., J.G.], Services de Physiologie [C.G., H.T.] et de Réanimation Médicale Pédiatrique [S.D.], Hôpital Robert Debré, 75019 Paris, France ABSTRACT Hirschsprung disease, neuroblastomas, and congenital central crest disorders, international databases of clinical symptoms and hypoventilation syndrome can occur in combination, and familial molecular test results should be established. Furthermore, the cases have been reported in all three conditions. This suggests development of genetic mouse models should help to improve variable expression of a single genetic abnormality as the com- our understanding of the molecular mechanisms underlying neu- mon cause to these neural crest disorders. Because the PHOX2B ral crest disorders. (Pediatr Res 58: 1–6, 2005) gene is pivotal in the development of most relays of the auto- nomic nervous system, including all autonomic neural crest derivatives, it was considered a candidate gene for the above Abbreviations conditions. Recent studies have shown that 1) PHOX2B is the ANS, autonomic nervous system main disease-causing gene for congenital central hypoventilation CCHS, congenital central hypoventilation syndrome syndrome, an autosomal dominant disorder with incomplete HASH-1, human achaete-scute homologous 1 gene penetrance; 2) PHOX2B is the first gene for which germline HSCR, Hirschsprung disease mutations have been demonstrated to predispose to neuroblas- LO-CHS, late-onset central hypoventilation syndrome toma; and 3) Hirschsprung disease was associated with an in- MASH-1, mammalian achaete-scute homologous 1 gene tronic single-nucleotide polymorphism of the PHOX2B gene in a PHOX2B, paired-like homeobox 2b gene case-control study. -

The NANOG Transcription Factor Induces Type 2 Deiodinase Expression and Regulates the Intracellular Activation of Thyroid Hormone in Keratinocyte Carcinomas
Cancers 2020, 12 S1 of S18 Supplementary Materials: The NANOG Transcription Factor Induces Type 2 Deiodinase Expression and Regulates the Intracellular Activation of Thyroid Hormone in Keratinocyte Carcinomas Annarita Nappi, Emery Di Cicco, Caterina Miro, Annunziata Gaetana Cicatiello, Serena Sagliocchi, Giuseppina Mancino, Raffaele Ambrosio, Cristina Luongo, Daniela Di Girolamo, Maria Angela De Stefano, Tommaso Porcelli, Mariano Stornaiuolo and Monica Dentice Figure S1. Strategy for the mutagenesis of Dio2 promoter. (A) Schematic representation of NANOG Binding Site within the Dio2 promoter region. (B) Schematic diagram for site‐directed mutagenesis of NANOG Binding Site on Dio2 promoter region by Recombinant PCR. (C) Representation of the mutated NANOG Binding Site on Dio2 promoter region. (D) Electropherogram of the NANOG Binding Site mutation within the Dio2 promoter. Cancers 2020, 12 S2 of S18 Figure S2. Strategy for the silencing of NANOG expression. (A) Cloning strategies for the generation of NANOG shRNA expression vectors. (B) Electropherograms of the NANOG shRNA sequences cloned into pcDNA3.1 vector. (C) Validation of effective NANOG down-modulation by two different NANOG shRNA vectors was assessed by Western Blot analysis of NANOG expression in BCC cells. (D) Quantification of NANOG protein levels versus Tubulin levels in the same experiment as in C is represented by histograms. Cancers 2020, 12 S3 of S18 Figure S3. The CD34+ cells are characterized by the expression of typical epithelial stemness genes. The mRNA levels of a panel of indicated stemness markers of epidermis were measured by Real Time PCR in the same experiment indicated in figure 3F and G. Cancers 2020, 12 S4 of S18 Figure S4. -
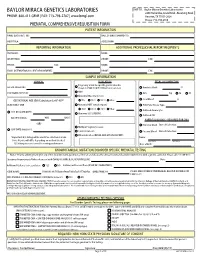
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Stem Cell 2015;6(2) 56
Stem Cell 2015;6(2) http://www.sciencepub.net/stem Stem Cell and Transcript Research Literatures Ma Hongbao 1, Margaret Young 2, Yang Yan 1 1 Brookdale Hospital, Brooklyn, New York 11212, USA; 2 Cambridge, MA 02138, USA [email protected] Abstract: The stem cell is the origin of an organism’s life that has the potential to develop into many different types of cells in life bodies. In many tissues stem cells serve as a sort of internal repair system, dividing essentially without limit to replenish other cells as long as the person or animal is still alive. When a stem cell divides, each new cell has the potential either to remain a stem cell or become another type of cell with a more specialized function, such as a red blood cell or a brain cell. This article introduces recent research reports as references in the stem cell and transcript related studies. [Ma H, Young M, Yang Y. Stem Cell and Transcript Research Literatures. Stem Cell. 2015;6(2):56-72] (ISSN 1545-4570). http://www.sciencepub.net/stem. 8 Key words: stem cell; transcript; life; research; literature 1. Introduction REST (322) target genes. The majority of these The stem cell is the origin of an organism’s life CoREST targets do not contain known RE1 motifs. that has the potential to develop into many different Notably, these CoREST target genes do play important types of cells in life bodies. In many tissues stem cells roles in pluripotency networks, in modulating NSC serve as a sort of internal repair system, dividing identity and fate decisions and in epigenetic processes essentially without limit to replenish other cells as previously associated with both REST and CoREST. -

Discovery of Biased Orientation of Human DNA Motif Sequences
bioRxiv preprint doi: https://doi.org/10.1101/290825; this version posted January 27, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Discovery of biased orientation of human DNA motif sequences 2 affecting enhancer-promoter interactions and transcription of genes 3 4 Naoki Osato1* 5 6 1Department of Bioinformatic Engineering, Graduate School of Information Science 7 and Technology, Osaka University, Osaka 565-0871, Japan 8 *Corresponding author 9 E-mail address: [email protected], [email protected] 10 1 bioRxiv preprint doi: https://doi.org/10.1101/290825; this version posted January 27, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 11 Abstract 12 Chromatin interactions have important roles for enhancer-promoter interactions 13 (EPI) and regulating the transcription of genes. CTCF and cohesin proteins are located 14 at the anchors of chromatin interactions, forming their loop structures. CTCF has 15 insulator function limiting the activity of enhancers into the loops. DNA binding 16 sequences of CTCF indicate their orientation bias at chromatin interaction anchors – 17 forward-reverse (FR) orientation is frequently observed. DNA binding sequences of 18 CTCF were found in open chromatin regions at about 40% - 80% of chromatin 19 interaction anchors in Hi-C and in situ Hi-C experimental data.