Redesigning Care Through Digital Health Implementation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Financial Reporting and Is Ultimately Responsible for Reviewing and Approving the Financial Statements
Treasury Board Secretariat ANNUAL REPORT OF ONTARIO Financial Statements of Government Organizations VOLUME 2B | 2015-2016 7$%/( 2)&217(176 9ROXPH% 3DJH *HQHUDO 5HVSRQVLEOH0LQLVWU\IRU*RYHUQPHQW$JHQFLHV LL $*XLGHWRWKHAnnual Report .. LY ),1$1&,$/ 67$7(0(176 6HFWLRQ ņ*RYHUQPHQW 2UJDQL]DWLRQV± &RQW¶G 1LDJDUD3DUNV&RPPLVVLRQ 0DUFK 1RUWKHUQ2QWDULR+HULWDJH)XQG&RUSRUDWLRQ 0DUFK 2QWDULR$JHQF\IRU+HDOWK 3URWHFWLRQDQG 3URPRWLRQ 3XEOLF+HDOWK2QWDULR 0DUFK 2QWDULR&DSLWDO*URZWK&RUSRUDWLRQ 0DUFK 2QWDULR&OHDQ :DWHU$JHQF\ 'HFHPEHU 2QWDULR(GXFDWLRQDO&RPPXQLFDWLRQV$XWKRULW\ 79 2QWDULR 0DUFK 2QWDULR(OHFWULFLW\)LQDQFLDO&RUSRUDWLRQ 0DUFK 2QWDULR(QHUJ\%RDUG 0DUFK 2QWDULR)LQDQFLQJ$XWKRULW\ 0DUFK 2QWDULR)UHQFK/DQJXDJH(GXFDWLRQDO&RPPXQLFDWLRQV$XWKRULW\ 0DUFK 2QWDULR,PPLJUDQW,QYHVWRU&RUSRUDWLRQ 0DUFK 2QWDULR,QIUDVWUXFWXUH DQG/DQGV&RUSRUDWLRQ ,QIUDVWUXFWXUH 2QWDULR 0DUFK 2QWDULR0RUWJDJH DQG+RXVLQJ&RUSRUDWLRQ 0DUFK 2QWDULR1RUWKODQG7UDQVSRUWDWLRQ&RPPLVVLRQ 0DUFK 2QWDULR3ODFH&RUSRUDWLRQ 'HFHPEHU 2QWDULR5DFLQJ&RPPLVVLRQ 0DUFK 2QWDULR6HFXULWLHV&RPPLVVLRQ 0DUFK 2QWDULR7RXULVP0DUNHWLQJ3DUWQHUVKLS&RUSRUDWLRQ 0DUFK 2QWDULR7ULOOLXP)RXQGDWLRQ 0DUFK 2UQJH 0DUFK 2WWDZD&RQYHQWLRQ&HQWUH &RUSRUDWLRQ 0DUFK 3URYLQFH RI2QWDULR&RXQFLOIRUWKH$UWV 2QWDULR$UWV&RXQFLO 0DUFK 7KH 5R\DO2QWDULR0XVHXP 0DUFK 7RURQWR 2UJDQL]LQJ&RPPLWWHHIRUWKH 3DQ $PHULFDQ DQG3DUDSDQ$PHULFDQ*DPHV 7RURQWR 0DUFK 7RURQWR :DWHUIURQW5HYLWDOL]DWLRQ&RUSRUDWLRQ :DWHUIURQW7RURQWR 0DUFK L ANNUAL REPORT 5(63216,%/(0,1,675<)25*29(510(17%86,1(66(17(535,6(6 25*$1,=$7,216758676 0,6&(//$1(286),1$1&,$/67$7(0(176 -

Freedom Liberty
2013 ACCESS AND PRIVACY Office of the Information and Privacy Commissioner Ontario, Canada FREEDOM & LIBERTY 2013 STATISTICS In free and open societies, governments must be accessible and transparent to their citizens. TABLE OF CONTENTS Requests by the Public ...................................... 1 Provincial Compliance ..................................... 3 Municipal Compliance ................................... 12 Appeals .............................................................. 26 Privacy Complaints .......................................... 38 Personal Health Information Protection Act (PHIPA) .................................. 41 As I look back on the past years of the IPC, I feel that Ontarians can be assured that this office has grown into a first-class agency, known around the world for demonstrating innovation and leadership, in the fields of both access and privacy. STATISTICS 4 1 REQUESTS BY THE PUBLIC UNDER FIPPA/MFIPPA There were 55,760 freedom of information (FOI) requests filed across Ontario in 2013, nearly a 6% increase over 2012 where 52,831 were filed TOTAL FOI REQUESTS FILED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,995 17,334 34,329 Provincial 7,029 14,402 21,431 Total 24,024 31,736 55,760 TOTAL FOI REQUESTS COMPLETED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,726 17,304 34,030 Provincial 6,825 13,996 20,821 Total 23,551 31,300 54,851 TOTAL FOI REQUESTS COMPLETED BY SOURCE AND JURISDICTION Municipal Provincial Total -

An Urgent Statement from Hospitals in the City of Toronto and the Regions of Durham, Halton, Peel and York GTA Hospitals Support Further Lockdown Measures
An Urgent Statement from Hospitals in the City of Toronto and the Regions of Durham, Halton, Peel and York GTA Hospitals Support Further Lockdown Measures December 20, 2020 - Today, on behalf of our patients, health care workers and staff, we are supporting the Ontario Hospital Association’s call for stronger lockdown measures from the Government of Ontario. Across the Greater Toronto Area, COVID-19 infections are continuing to rise, as are hospitalizations and intensive care cases. These trends show no sign of slowing – in fact, a surge in cases following the holiday season is expected to make the situation even worse. Our staff are caring for increasing numbers of COVID-19 patients in hospitals and assisting in other settings such as long-term care homes. They are also keeping up with the care needs of patients without COVID-19 and trying to make progress in the significant backlog of scheduled surgeries and procedures cancelled during the first wave. For many months now, these frontline health care workers have been devoting enormous energy and skill to caring for their patients, at the very epicenter of the pandemic. They are stressed and overstretched. This level of strain is simply not sustainable for much longer. We are seeing increasing numbers of staff becoming ill and not able to work – both with COVID-19 and other illnesses. While we are coping and planning for redeployment, we are seeing more illness and stress and hearing about the toll this is taking on people’s families. We recognize that lockdown measures are challenging for many members of our communities, but we cannot afford to put patients and health care workers at further risk. -

ITAC Health PHIPA Modernization Feedback to ONTARIO MOHLTC FEBRUARY 21, 2020 Summary 2
ITAC Health PHIPA Modernization Feedback TO ONTARIO MOHLTC FEBRUARY 21, 2020 Summary 2 At the conclusion of November 20, 2019 meeting hosted by the MOHLTC privacy policy team that included representatives from ITAC Health Board and members, an action opportunity was requested and permission received to share the Ministry’s PHIPA Modernization document with select privacy subject matter experts within the ITAC Health membership. ITAC Health members, including SME members, have provided input that has been collected and summarized in this document. Our goal is to provide timely and in-depth feedback beyond the November meeting’s initial reflections on the PHIPA Modernization policies. We appreciate the opportunity to contribute to the Ministry our summary that includes five sections in companion to this executive summary: thematic topics related to PHIPA Modernization; beyond PHIPA, privacy (and security) contextual discussion; and general comments, recommendations and questions on PHIPA Modernization; direct references to slide content in Ministry’s PHIPHA Modernization deck; bibliography of external documents relevant to PHIPA Modernization effort 1. PHIPA Privacy Themes 3 Roles and responsibilities under the new PHIPA Penalties Under the New PHIPA Consent – aligned with GDPR Patient access to information De-identification and secondary use Right to portability Right to be forgotten Breach notification Research Ethic Boards harmonization Governance operating model Levers for change to enable data sharing Roles and responsibilities under the 4 new PHIPA Patient - a natural person whose personal data is processed by a controller or processor Health information custodian (HIC) - a person who determines the purposes for which and the manner in which any personal data are, or are to be, processed. -
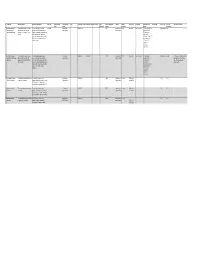
Copy of Data Inventory
Copy of Data Inventory # Public Title Short Description Long Description (Body) Other Title Data Custodian Data Custodian Tags Date Range ‐ Start Date Range ‐ End Date Created Date Contains Geographic Publisher Update Access Level Exemption Rationale not to Dataset URL License Type File Types Additional Comments Email Branch published Markers Frequency Release (extensions) 1 Consent and Capacity This dataset contains case‐related The case management system CaseLoad Consent and 2014‐03‐15 TRUE Consent and Daily Restricted Confidentiality The case management Other Licence DBF Board (CCB) Case data and information for CCB provides case‐related data such as Capacity Board Capacity Board system contains Management System applications from March 15 2014 contact information of the parties that private contact onward. come before the CCB, information information, about the hearing scheduling process, reference to personal file status, hearing information and health information case disposition. and sensitive, confidential party/case information. 2 Consent and Capacity This dataset contains case‐related The scheduling database provides Consent and 2006‐04‐01 2014‐03‐14 TRUE Consent and Other Restricted Confidentiality The scheduling Other Licence ACCDB This dataset is no longer updated. Board (CCB) Scheduling data and information for CCB case‐related data such as contact Capacity Board Capacity Board database contains Data not used for day‐to‐day Database applications from April 1 2006 to information of the parties that come private contact business. Occasional use for March 14 2014. before the CCB, information about the information, reference only. hearing scheduling process, file status, reference to personal hearing information and case health information disposition. and sensitive, confidential party/case information. -

Ontario's Electronic Health Record (EHR
Ontario’s Electronic Health Record (EHR) Conceptual Information Model (CIM) Digital Health Enabled VERSION 2.0 Version History Version Number Date Summary of Change Changed By 1.0 November 2014 Initial version part of Ontario’s Ehealth Blueprint eHealth Ontario, Architecture & Standards Division 2.0 June 26, 2019 Updated to align with HL7 Electronic Health Record eHealth Ontario, Architecture & System Functional Model (EHR-S FM) [Draft Standards Division Release 2.1] CIM 2.0 Page 1 Table of Contents Introduction ...................................................................................................................................................................... 3 Overview ............................................................................................................................................................................ 4 Information Architecture .................................................................................................................................................................................................... 6 EHR Information Principles ............................................................................................................................................................................................... 6 Modelling References .......................................................................................................................................................................................................... 7 Conceptual Information -

Exhibit 2 Crown-Controlled Corporations
Exhibit 2 Crown-Controlled Corporations Corporations whose accounts are audited by an auditor other than the Auditor General, with full access by the Auditor General to audit reports, working papers and other related documents as required Alcohol and Gaming Commission of Ontario North West Local Health Integration Network Agricultural Research Institute of Ontario Ontario Capital Growth Corporation Central East Local Health Integration Network Ontario College of Trades Central Local Health Integration Network Ontario French-language Educational Central West Local Health Integration Network Communications Authority (TFO) Champlain Local Health Intgration Network Ontario Health Quality Council Education Quality and Accountability Office Ontario Infrastructure and Lands Corporation eHealth Ontario (Infrastructure Ontario) Erie St. Clair Local Health Integration Network Ontario Lottery and Gaming Corporation Forest Renewal Trust Ontario Pension Board (Dec 31)* General Real Estate Portfolio Ontario Power Generation Inc. (Dec 31)* Hamilton Niagara Haldimand Brant Local Health Ontario Tourism Marketing Partnership Corporation Integration Network Ontario Trillium Foundation HealthForceOntario Marketing and Recruitment Ottawa Convention Centre Corporation Agency Owen Sound Transportation Company Limited Health Shared Services Ontario (HSSOntario) Ontario Agency for Health Protection and Higher Education Quality Council of Ontario Promotion (Public Health Ontario) Human Rights Legal Support Centre Royal Ontario Museum Hydro One Inc. (Dec 31)* Science -

MEDICAL RESOURCES During COVID-19
MEDICAL RESOURCES During COVID-19 If You Think You Have COVID-19: If you are having symptoms of COVID-19 and need to get screened, it is important to follow the guidelines of Toronto Public Health and the Government of Ontario. DO NOT show up unannounced at a clinic or hospital. Instead follow these guidelines: Review this Self-Assessment Tool www.ontario.ca/page/2019-novel-coronavirus-covid-19-self-assessment If you answered yes to any of those questions on the Self-Assessment Tool, then seek assistance over the phone with Telehealth Ontario: Telehealth Ontario 24/7 | 1-866-797-0000 | Speak with a registered nurse regarding your symptoms If it is confirmed you need to be tested, visit one of these dedicated COVID-19 assessment centres: William Osler Health System – Peel Memorial 2-8pm daily | 20 Lynch Street, Brampton | 905-494-2120 Trillium Health Partners 9:30am-9:30pm daily | call 905-799-7700 first Mississauga Hospital: 15 Bronte College Court, Mississauga, ON Credit Valley Hospital: 2200 Erin Mills Parkway, Mississauga, ON North York General Hospital 11am-11pm daily | 4001 Leslie Street, North York, ON | 416-756-6000 Michael Garron Hospital 8am-8pm | 825 Coxwell Avenue | 416-469-6858 BY APPOINTMENT ONLY. CALL TO BOOK. Women’s College Hospital 9am-8pm daily | 76 Grenville Street | 416-323-6400 Humber River Hospital 12pm-8pm Monday-Friday | 2111 Finch Avenue West | 416-242-1000 St. Joseph’s Health Centre 9am-9pm daily | Sunnyside Building 1st floor; 30 The Queensway St. Michael’s Hospital 9am-7pm daily | Li Ka Shing Knowledge Institute; -

Hospital Lhins Contact List
Hospital LHINs Contact List Patient Hospital LHIN Hospital LHIN LHIN Hospital Inquiry or Main Direct # or Address Map Fax # Number Extension Hotel-Dieu Grace Healthcare 519-257-5111 1453 Prince Rd Map it! (HDGH)(Windsor) Windsor, ON N9C 3Z4 Leamington District Memorial 519-326-2373 194 Talbot St W Map it! Hospital Leamington, ON N8H 1N9 Windsor Regional Hospital- 519-254-5577 1995 Lens Ave Map it! Metropolitan Campus Windsor, ON N8W 1L9 Windsor Regional Hospital- 519-253-5253 2220 Kildare Rd Map it! Erie St Clair LHIN Windsor Regional Cancer Windsor, ON N8W 2X3 1-888-447-4468 Centre Windsor Regional Hospital- 519-973-4411 1030 Ouellette Ave Map it Ouellette Campus Windsor, ON N9A 1E1 Chatham-Kent Health 519-352-6400 80 Grand Ave W Map it! Alliance-Chatham Campus Chatham, ON N7M 5L9 Chatham-Kent Health 519-352-6400 325 Margaret Ave Map it! Alliance Sydenham Campus Wallaceburg ON, N8A 2A7 Bluewater Health 419-464-4400 89 Norman St Map it! Sarnia, ON N7T 6S3 Charlotte Eleanor Englehart 519-882-4325 450 Blanche St Map it! Hospital of Bluewater Health Petrolia, ON N0N 1R0 1 Jan 2012 (Update Oct 12, 2016) Hospital LHIN(s) Contact List - Ontario Page 1 of 15 Patient Hospital LHIN Hospital LHIN LHIN Hospital Inquiry or Main Direct # or Address Map Fax # Number Extension Middlesex Hospital Alliance- 519-693-4441 519-474-5662 519-472-4045 1824 Concession Dr Map it! Four Counties Health Services Newbury, ON N0L 1Z0 Middlesex Hospital Alliance- 519-245-5295 519-474-5662 519-472-4045 395 Carrie St Map it! Strathroy Middlesex General Strathroy, ON N7G 3J4 Hospital London Health Sciences Centre 519-685-8500 519-474-5662 519-472-4045 800 Commissioners Rd E Map it! - Victoria Hospital London, ON N6A 5W9 London Health Sciences 519-685-8500 519-474-5662 519-472-4045 339 Windermere Rd Map it! Centre-University Hospital London, ON N6A 5A5 St Joseph's Health Care 519-646-6100 519-474-5662 519-472-4045 268 Grosvenor St Map it! London- St. -

Information Security and Privacy Policy IM-002 May 2018
Information Security and Privacy Policy IM-002 May 2018 1. Purpose: Patient Ombudsman will be collecting Sensitive Information that includes personal information (PI) and personal health information (PHI) in order to carry out its business functions described in the Excellent Care for All Act, 2010, S.O. 2010, c. 14 (ECFAA). This document sets out Patient Ombudsman’s policies regarding the management of information security and privacy protection. Information security refers to methodologies that protect information from unauthorized access, use, disclosure, disruption or destruction regardless of how the information is formatted or whether it is being processed or stored. Included in this document is the protection of privacy, managing security-related risks and limiting potential breach of privacy. The security of information and the protection of privacy is critical to the success of Patient Ombudsman to provide effective customer service and maintain public trust. Patient Ombudsman shall act as a responsible conservator of information assets entrusted to its care and shall promote a culture of information security and privacy. Loss of confidentiality, integrity, or availability of information and possible breach could adversely affect the achievement of Patient Ombudsman’s mandate and ability to store Sensitive Information. 2. Scope: This policy applies to all Employees of Patient Ombudsman. 3. Definitions: Business Owner: means any program director or equivalent having authority and accountability under legislation or policy for particular business activities and related business records. Employee: means a person employed by, or on contract with the Ontario Health Quality Council to work exclusively for Patient Ombudsman, and a person employed by or on contract to the Ontario Health Quality Council, operating as Health Quality Ontario, and assigned to provide Information Technology support to Patient Ombudsman. -

Fracture Clinic Access at Toronto Hospitals Not All Hospitals Offer Fracture Clinic Telephone Call Or Referral Required - No Walk-Ins Accepted
Fracture Clinic Access at Toronto Hospitals Not all hospitals offer fracture clinic Telephone call or referral required - no walk-ins accepted Note: Fracture clinics are not for initial evaluation and stabilization of acute fractures. This must be done at primary care or emergency department level as appropriate Humber River Hospital 416-242-1000 Monday to Friday 7:30 am – 4:30 pm 1235 Wilson Ave x 23000 2.5 hrs for each AM, PM clinic Toronto, M3M 0B2 Call to speak to ortho-on-call, will accept if space avail Michael Garron Hospital 416-469-6384 Monday, Tuesday, Friday 8 – 4 pm 825 Coxwell Avenue Fx: 416-469-6424 Wednesday, Thurs 8:30 – 4 pm Toronto, M4C 3E7 Referral triaged according to urgency North York General Hospital 416-756-6970 Use referral form, only for minor fracture, 1st flr, West Lobby Fx: 416-756-6502 splinting/casting 4001 Leslie St., 1st flr Located near the Information Desk Toronto, M2K 1E1 Scarborough Health Network 416-495-2557 Referrals/consultation not accepted from Birchmount Hospital community physicians/NPs. 2 ways to access clinic: 3030 Birchmount Rd., 1) Through ER d/t injury Scarborough, M1W 3W3 2) Apt scheduled by Ortho Scarborough Health Network 416-431-8212 Monday to Thursday 7:00-3:00 pm General Hospital Refer to individual Ortho to obtain appointment 3050 Lawrence Ave. E., Scarborough, M1P 2V5 Scarborough Health Network 416-281-7269 Monday to Friday 7:30-3:30 pm Centenary Hospital Fx: 416-281-7204 2867 Ellesmere Road, M1E 4B9 Mount Sinai Hospital 416-596-4200 Clinic hours vary. -

Supporting Those Impacted by COVID-19
Supporting those impacted by COVID-19 Many of you have reached out to us either looking for suggestions or offering ideas on how our TFS community can support those impacted by COVID-19. We are indeed a strong community and we know that it is essential, as citizens, that we act for the common good, most especially in situations such as this one. Please see below a list of organizations that you might want to support, specifically considering the shortage of personal protective equipment and other items. Of the many worthy institutions making an impact, we have put together a list of those with which we have partnered over the years as part of our citizenship program or where our alumni and parents are engaged. We will post this list online at tfs.ca and sr.tfs.ca/coronavirus. To quote President John F. Kennedy, from his inaugural speech, “Ask not what your country can do for you - ask what you can do for your country.” Or province or city. And, of course, for the world at large. Thank you! Baycrest Hospital CAMH Canadian Cancer Society Daily Bread Food Bank Holland Bloorview Kids Rehabilitation Hospital Humber River Hospital Lakeridge Health Mackenzie Health Markham Stouffville Hospital Michael Garron Hospital Foundation Oakville Hospital Foundation North York General Hospital Foundation Second Harvest Scarborough Hospital Network Foundation Sick Kids Foundation Sinai Health System Southlake Regional Health Centre Sunnybrook Health Sciences Centre Toronto General & Western Hospitals Toronto Rehab Trillium Health Partners Foundation Unity Health (St. Michael's, St. Joseph's and Providence Health Care) War Child William Osler Health System Women's College Hospital Foundation .