Ontario's Electronic Health Record (EHR
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Financial Reporting and Is Ultimately Responsible for Reviewing and Approving the Financial Statements
Treasury Board Secretariat ANNUAL REPORT OF ONTARIO Financial Statements of Government Organizations VOLUME 2B | 2015-2016 7$%/( 2)&217(176 9ROXPH% 3DJH *HQHUDO 5HVSRQVLEOH0LQLVWU\IRU*RYHUQPHQW$JHQFLHV LL $*XLGHWRWKHAnnual Report .. LY ),1$1&,$/ 67$7(0(176 6HFWLRQ ņ*RYHUQPHQW 2UJDQL]DWLRQV± &RQW¶G 1LDJDUD3DUNV&RPPLVVLRQ 0DUFK 1RUWKHUQ2QWDULR+HULWDJH)XQG&RUSRUDWLRQ 0DUFK 2QWDULR$JHQF\IRU+HDOWK 3URWHFWLRQDQG 3URPRWLRQ 3XEOLF+HDOWK2QWDULR 0DUFK 2QWDULR&DSLWDO*URZWK&RUSRUDWLRQ 0DUFK 2QWDULR&OHDQ :DWHU$JHQF\ 'HFHPEHU 2QWDULR(GXFDWLRQDO&RPPXQLFDWLRQV$XWKRULW\ 79 2QWDULR 0DUFK 2QWDULR(OHFWULFLW\)LQDQFLDO&RUSRUDWLRQ 0DUFK 2QWDULR(QHUJ\%RDUG 0DUFK 2QWDULR)LQDQFLQJ$XWKRULW\ 0DUFK 2QWDULR)UHQFK/DQJXDJH(GXFDWLRQDO&RPPXQLFDWLRQV$XWKRULW\ 0DUFK 2QWDULR,PPLJUDQW,QYHVWRU&RUSRUDWLRQ 0DUFK 2QWDULR,QIUDVWUXFWXUH DQG/DQGV&RUSRUDWLRQ ,QIUDVWUXFWXUH 2QWDULR 0DUFK 2QWDULR0RUWJDJH DQG+RXVLQJ&RUSRUDWLRQ 0DUFK 2QWDULR1RUWKODQG7UDQVSRUWDWLRQ&RPPLVVLRQ 0DUFK 2QWDULR3ODFH&RUSRUDWLRQ 'HFHPEHU 2QWDULR5DFLQJ&RPPLVVLRQ 0DUFK 2QWDULR6HFXULWLHV&RPPLVVLRQ 0DUFK 2QWDULR7RXULVP0DUNHWLQJ3DUWQHUVKLS&RUSRUDWLRQ 0DUFK 2QWDULR7ULOOLXP)RXQGDWLRQ 0DUFK 2UQJH 0DUFK 2WWDZD&RQYHQWLRQ&HQWUH &RUSRUDWLRQ 0DUFK 3URYLQFH RI2QWDULR&RXQFLOIRUWKH$UWV 2QWDULR$UWV&RXQFLO 0DUFK 7KH 5R\DO2QWDULR0XVHXP 0DUFK 7RURQWR 2UJDQL]LQJ&RPPLWWHHIRUWKH 3DQ $PHULFDQ DQG3DUDSDQ$PHULFDQ*DPHV 7RURQWR 0DUFK 7RURQWR :DWHUIURQW5HYLWDOL]DWLRQ&RUSRUDWLRQ :DWHUIURQW7RURQWR 0DUFK L ANNUAL REPORT 5(63216,%/(0,1,675<)25*29(510(17%86,1(66(17(535,6(6 25*$1,=$7,216758676 0,6&(//$1(286),1$1&,$/67$7(0(176 -
Health Informatics Principles
Health Informatics Principles Foundational Curriculum: Cluster 4: Informatics Module 7: The Informatics Process and Principles of Health Informatics Unit 2: Health Informatics Principles FC-C4M7U2 Curriculum Developers: Angelique Blake, Rachelle Blake, Pauliina Hulkkonen, Sonja Huotari, Milla Jauhiainen, Johanna Tolonen, and Alpo Vӓrri This work is produced by the EU*US eHealth Work Project. This project has received funding from the European Union’s Horizon 2020 research and 21/60 innovation programme under Grant Agreement No. 727552 1 EUUSEHEALTHWORK Unit Objectives • Describe the evolution of informatics • Explain the benefits and challenges of informatics • Differentiate between information technology and informatics • Identify the three dimensions of health informatics • State the main principles of health informatics in each dimension This work is produced by the EU*US eHealth Work Project. This project has received funding from the European Union’s Horizon 2020 research and FC-C4M7U2 innovation programme under Grant Agreement No. 727552 2 EUUSEHEALTHWORK The Evolution of Health Informatics (1940s-1950s) • In 1940, the first modern computer was built called the ENIAC. It was 24.5 metric tonnes (27 tons) in volume and took up 63 m2 (680 sq. ft.) of space • In 1950 health informatics began to take off with the rise of computers and microchips. The earliest use was in dental projects during late 50s in the US. • Worldwide use of computer technology in healthcare began in the early 1950s with the rise of mainframe computers This work is produced by the EU*US eHealth Work Project. This project has received funding from the European Union’s Horizon 2020 research and FC-C4M7U2 innovation programme under Grant Agreement No. -

Freedom Liberty
2013 ACCESS AND PRIVACY Office of the Information and Privacy Commissioner Ontario, Canada FREEDOM & LIBERTY 2013 STATISTICS In free and open societies, governments must be accessible and transparent to their citizens. TABLE OF CONTENTS Requests by the Public ...................................... 1 Provincial Compliance ..................................... 3 Municipal Compliance ................................... 12 Appeals .............................................................. 26 Privacy Complaints .......................................... 38 Personal Health Information Protection Act (PHIPA) .................................. 41 As I look back on the past years of the IPC, I feel that Ontarians can be assured that this office has grown into a first-class agency, known around the world for demonstrating innovation and leadership, in the fields of both access and privacy. STATISTICS 4 1 REQUESTS BY THE PUBLIC UNDER FIPPA/MFIPPA There were 55,760 freedom of information (FOI) requests filed across Ontario in 2013, nearly a 6% increase over 2012 where 52,831 were filed TOTAL FOI REQUESTS FILED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,995 17,334 34,329 Provincial 7,029 14,402 21,431 Total 24,024 31,736 55,760 TOTAL FOI REQUESTS COMPLETED BY JURISDICTION AND RECORDS TYPE Personal Information General Records Total Municipal 16,726 17,304 34,030 Provincial 6,825 13,996 20,821 Total 23,551 31,300 54,851 TOTAL FOI REQUESTS COMPLETED BY SOURCE AND JURISDICTION Municipal Provincial Total -
Redesigning Care Through Digital Health Implementation
Redesigning Care through Digital Health Implementation Lessons Learned from Ontario Hospitals Acknowledgements The Ontario Hospital Association (OHA) would like to thank all the member hospitals and provincial partners who contributed to this resource. Individual contributing authors are noted at the end of each story. The OHA also acknowledges the ongoing and valuable work of all health care professionals who embrace change as hospitals innovate to improve care delivery and patient experiences. Disclaimer This publication is a collection of hospital submissions The Ontario Hospital Association (OHA) assumes no showcasing digital health implementation initiatives responsibility or liability for any harm, damage or other across the province. It has been created for general losses, direct or indirect, resulting from any reliance on information purposes only and implementation the use or the misuse of any information contained in suggestions should be adapted to the circumstances of this resource. Facts, figures and resources mentioned each hospital. Hospitals should seek their own legal and/ throughout the document have not been validated by or professional advice and opinion when developing the OHA. For details on sources of information, readers their organization’s approach and plans for digital health are encouraged to contact the hospital directly using the implementation. contact information cited in each submission. I Introduction Digital technologies have, and will continue to, These factors point to what may be the key ingredient -

Rapid Review Mental Health Interventions 1 Rapid
Rapid review mental health interventions 1 Rapid review and meta-meta-analysis of self-guided interventions to address anxiety, depression and stress during COVID-19 social distancing Ronald Fischer ¹ ² Tiago Bortolini ² Johannes Alfons Karl ¹ Marcelo Zilberberg 3 Kealagh Robinson ¹ André Rabelo 4 Lucas Gemal ² Daniel Wegerhoff ¹ Nguyễn Thị Bảo Trâm ¹ Briar Irving ¹ Megan Chrystal 1 Paulo Mattos ² ⁵ Affiliations 1 Victoria University of Wellington, Wellington, New Zealand 2 Instituto D’Or de Pesquisa & Ensino, Rio de Janeiro, Brazil 3 TAL Education Group, Beijing, China 4 Universidade de Brasília, Brasília, Brazil 5 Institute of Psychiatry, Federal University of Rio de Janeiro Author contributions RF conceptualized the study; RF, TB, JK, MZ, KR, AR, LG conducted the literature search & data extraction, RF, JK, TB conducted the analyses & created the visualizations, DW coordinated the activity material collation, DW, TN, BI, MC collated & summarized the activity material; PM provided feedback & advice; RF wrote the first draft; all authors approved the final version. Abstract We conducted a rapid review and quantitative summary of meta-analyses that have examined interventions which can be used by individuals during quarantine and social distancing to manage anxiety, depression, stress and subjective well-being. A literature search yielded 34 meta-analyses (total number of studies k = Rapid review mental health interventions 2 1,390, n = 145,744) that were summarized. Overall, self-guided interventions showed small to medium effects in comparison to control groups. In particular, self-guided therapeutic approaches (including cognitive-behavioral, mindfulness, and acceptance-based interventions), selected positive psychology interventions, and multi-component and activity-based interventions (music, physical exercise) showed promising evidence for effectiveness. -

ITAC Health PHIPA Modernization Feedback to ONTARIO MOHLTC FEBRUARY 21, 2020 Summary 2
ITAC Health PHIPA Modernization Feedback TO ONTARIO MOHLTC FEBRUARY 21, 2020 Summary 2 At the conclusion of November 20, 2019 meeting hosted by the MOHLTC privacy policy team that included representatives from ITAC Health Board and members, an action opportunity was requested and permission received to share the Ministry’s PHIPA Modernization document with select privacy subject matter experts within the ITAC Health membership. ITAC Health members, including SME members, have provided input that has been collected and summarized in this document. Our goal is to provide timely and in-depth feedback beyond the November meeting’s initial reflections on the PHIPA Modernization policies. We appreciate the opportunity to contribute to the Ministry our summary that includes five sections in companion to this executive summary: thematic topics related to PHIPA Modernization; beyond PHIPA, privacy (and security) contextual discussion; and general comments, recommendations and questions on PHIPA Modernization; direct references to slide content in Ministry’s PHIPHA Modernization deck; bibliography of external documents relevant to PHIPA Modernization effort 1. PHIPA Privacy Themes 3 Roles and responsibilities under the new PHIPA Penalties Under the New PHIPA Consent – aligned with GDPR Patient access to information De-identification and secondary use Right to portability Right to be forgotten Breach notification Research Ethic Boards harmonization Governance operating model Levers for change to enable data sharing Roles and responsibilities under the 4 new PHIPA Patient - a natural person whose personal data is processed by a controller or processor Health information custodian (HIC) - a person who determines the purposes for which and the manner in which any personal data are, or are to be, processed. -
Copy of Data Inventory
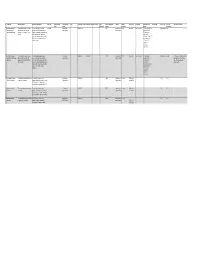
Copy of Data Inventory # Public Title Short Description Long Description (Body) Other Title Data Custodian Data Custodian Tags Date Range ‐ Start Date Range ‐ End Date Created Date Contains Geographic Publisher Update Access Level Exemption Rationale not to Dataset URL License Type File Types Additional Comments Email Branch published Markers Frequency Release (extensions) 1 Consent and Capacity This dataset contains case‐related The case management system CaseLoad Consent and 2014‐03‐15 TRUE Consent and Daily Restricted Confidentiality The case management Other Licence DBF Board (CCB) Case data and information for CCB provides case‐related data such as Capacity Board Capacity Board system contains Management System applications from March 15 2014 contact information of the parties that private contact onward. come before the CCB, information information, about the hearing scheduling process, reference to personal file status, hearing information and health information case disposition. and sensitive, confidential party/case information. 2 Consent and Capacity This dataset contains case‐related The scheduling database provides Consent and 2006‐04‐01 2014‐03‐14 TRUE Consent and Other Restricted Confidentiality The scheduling Other Licence ACCDB This dataset is no longer updated. Board (CCB) Scheduling data and information for CCB case‐related data such as contact Capacity Board Capacity Board database contains Data not used for day‐to‐day Database applications from April 1 2006 to information of the parties that come private contact business. Occasional use for March 14 2014. before the CCB, information about the information, reference only. hearing scheduling process, file status, reference to personal hearing information and case health information disposition. and sensitive, confidential party/case information. -
Insights from Patient Care Utilization in Colorado SEPTEMBER 2020
THE VALUE OF TELEMEDICINE DURING THE COVID-19 PANDEMIC RESPONSE Insights From Patient Care Utilization in Colorado SEPTEMBER 2020 Informing Policy. Advancing Health. The Value of Telemedicine During the COVID-19 Pandemic Response Insights From Patient Care Utilization in Colorado 3 Introduction CHI Staffers 4 The Value of Telemedicine During the COVID-19 Pandemic Response Contributing to This Report 5 Telemedicine Adoption and Use in Colorado 6 Methods: What You Need to Know • Kristi Arellano 7 Which Coloradans Are Using Telemedicine? • Jasmine Bains 7 Demographics: Telemedicine Adoption by Age • Nina Bastian 10 Demographics: Telemedicine Adoption by Race, Ethnicity, • Jeff Bontrager and Gender • Ashlie Brown 11 How Has Telemedicine Affected the Volume of Care Delivered • Spencer Budd by Different Providers During the Pandemic? • Brian Clark 12 Federally Qualified Health Centers • Joe Hanel 13 Community Mental Health Centers • Paul Presken 14 Other Provider Types • Sara Schmitt 14 Telemedicine Care Delivery by Health Condition and Procedure • Lindsey Whittington 17 Telemedicine Adoption by Insurance Type • Jackie Zubrzycki 18 Telemedicine Adoption by Modality (Telephone and Video) 21 Opportunities to Increase the Value of Telemedicine 22 What We Don’t Know Yet: Next Steps for Research 22 Conclusion 23 Methods Appendix 23 The Colorado Health Observation Regional Data Service (CHORDS) 23 Analysis Details 24 Baseline and Analysis Periods 25 Endnotes This research was conducted in collaboration with the Colorado Office of eHealth Innovation (OeHI) and the Colorado eHealth Commission, in support of the Colorado Health Information Technology (IT) Roadmap. OeHI is responsible for defining, maintaining, and evolving Colorado’s Health IT strategy concerning care coordination, data access, health care integration, payment reform, and care delivery. -

Identifying Health Consumers' Ehealth Literacy to Decrease Disparities In
CONTINUING EDUCATION ANCC 2.0 CONTACT HOURS Identifying Health Consumers’ eHealth Literacy to Decrease Disparities in Accessing eHealth Information Hyejin Park, PhD, RN, Eileen Cormier, PhD, RN, Glenna Gordon, Jung Hoon Baeg, MS resources. Consumer engagement in health-related decision The increasing amount of health information available on making has also increased in health service delivery.4 Be- the Internet highlights the importance of eHealth literacy ’ skills for health consumers. Low eHealth literacy results in cause online health information can affect health consumers disparities in health consumers’ ability to access and use health decisions and health outcomes, it is important for “ eHealth information. The purpose of this study was to as- them to possess eHealth literacy, defined as the ability to sess the perceived eHealth literacy of a general health con- seek, find, understand, appraise online health information, 5 sumer population so that healthcare professionals can and apply the knowledge to make a health decision.” effectively address skills gaps in health consumers’ ability The Internet provides a portal for everyone to access to access and use high-quality online health informa- available health knowledge, but disparities exist in con- tion. Participants were recruited from three public library sumers’ ability to parse the health information they read. branches in a Northeast Florida community. The eHealth Lit- The low level of eHealth literacy of some consumers makes eracy Scale was used. The majority of participants -

Exhibit 2 Crown-Controlled Corporations
Exhibit 2 Crown-Controlled Corporations Corporations whose accounts are audited by an auditor other than the Auditor General, with full access by the Auditor General to audit reports, working papers and other related documents as required Alcohol and Gaming Commission of Ontario North West Local Health Integration Network Agricultural Research Institute of Ontario Ontario Capital Growth Corporation Central East Local Health Integration Network Ontario College of Trades Central Local Health Integration Network Ontario French-language Educational Central West Local Health Integration Network Communications Authority (TFO) Champlain Local Health Intgration Network Ontario Health Quality Council Education Quality and Accountability Office Ontario Infrastructure and Lands Corporation eHealth Ontario (Infrastructure Ontario) Erie St. Clair Local Health Integration Network Ontario Lottery and Gaming Corporation Forest Renewal Trust Ontario Pension Board (Dec 31)* General Real Estate Portfolio Ontario Power Generation Inc. (Dec 31)* Hamilton Niagara Haldimand Brant Local Health Ontario Tourism Marketing Partnership Corporation Integration Network Ontario Trillium Foundation HealthForceOntario Marketing and Recruitment Ottawa Convention Centre Corporation Agency Owen Sound Transportation Company Limited Health Shared Services Ontario (HSSOntario) Ontario Agency for Health Protection and Higher Education Quality Council of Ontario Promotion (Public Health Ontario) Human Rights Legal Support Centre Royal Ontario Museum Hydro One Inc. (Dec 31)* Science -

Electronic Health Records in India
CSD Working Paper Series: Towards a New Indian Model of Information and Communications Technology-Led Growth and Development Electronic Health Records in India ICT India Working Paper #25 Manisha Wadhwa March 2020 CSD Working Paper Series: Towards a New Indian Model of Information and Communications Technology-Led Growth and Development Table of Contents Abbreviations ................................................................................................................................................ 4 Abstract ......................................................................................................................................................... 5 Introduction .................................................................................................................................................. 6 Benefits of EHR ............................................................................................................................................. 8 Initiatives by the Government of India ......................................................................................................... 8 EHR Standards ........................................................................................................................................... 8 Goals of EHR Standards ......................................................................................................................... 9 Need for EHR Standards ....................................................................................................................... -

Telepharmacy: the Pharmacy of the 21St Century
SMGr up Telepharmacy: The Pharmacy of the 21st Century Marlise Araújo dos Santos1,4*, Patrícia Bellicanta Lazzarotto1,4, Helena Willhelm de Oliveira2,4, Júlio César M de Lima3,4 and Thais Russomano4 1 2 Joan Vernikos Aerospace Pharmacy Laboratory, Brazil 3 eHealth Laboratory, Brazil 4 Aerospace Engineering Lab, Brazil *CorrespondingMicroG- PUCRS, Brazil author: Marlise Araújo dos Santos, Joan Vernikos Aerospace Pharmacy Laboratory, MicroG- PUCRS, Brazil, Tel: +55 51 998287743 and +55 51 33536369; Email:Published [email protected] Date: June 27, 2017 ABSTRACT Telehealth is a new area of health assistance, research, and education, in which information and telecommunication technologies (ICT) are used to give support services to communities where there is a lack of healthcare or access to particular specialties of medical assistance. One area of activity of telehealth is telepharmacy, which makes pharmaceutical assistance possible to remote and disadvantaged areas.This Chapter presents the establishment of the The Brazilian Telepharmacy experience is highlighted, which includes the laws and regulations first telepharmacy services in U.S. hospitals, its spread to local pharmacies and other countries. involving the rational use of medication and medicinal plants, and how the Brazilian Health Policy to medical doctors and dentists, nutritionists, pharmacists and physiotherapists can prescribe and System promotes and motivates this area. According to Brazilian laws, for example, in addition medicinal plants and phytotherapies to their patients. This Chapter also discusses the eHealth Telemedicine | www.smgebooks.com 1 Copyright dos Santos MA.This book chapter is open access distributed under the Creative Commons Attribution 4.0 International License, which allows users to download, copy and build upon published articles even for com- mercial purposes, as long as the author and publisher are properly credited.