ABMU Agenda Supplement for Council, 04/10/2018 15:00
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neath Port Talbot County Borough Council Cabinet 16
NEATH PORT TALBOT COUNTY BOROUGH COUNCIL CABINET 16 January 2019 REPORT OF THE HEAD OF LEGAL SERVICES – MR C GRIFFITHS Matter for Decision Wards Affected: All Adoption of the JNC Framework in setting Coroner Pay and review of the financial contributions made to the Joint Coroner Service between Neath Port Talbot County Borough Council and City and County of Swansea Purpose of the Report 1. To seek approval from Members to increase the financial contributions made to the Joint Coroner Service between Neath Port Talbot County Borough Council and the City and County of Swansea as a result of the adoption of the JNC Framework for Coroners pay. Background 2. The Coroners and Justice Act 2009 (Alteration of Coroner areas) Order 2013 formally amalgamated The City and County of Swansea (“Swansea”) with Neath Port Talbot County Borough Council (“NPT”) for the purposes of a single Coroner area. The cost of the service is split using a formula between the two authorities based on place of death. City and County of Swansea is the “relevant authority” in law and is required to appoint and agree the remuneration of the Senior Coroner. Presently NPT contributes the sum of £248,030 in the financial year 2017/2018 and it was originally proposed the same amount would have been made in 2018/2019. 3. The budget for the amalgamated Coroners Services see NPT contribute the sum of 34.5% of the total budget costs. The percentage is based on the number of deaths registered in the areas of Swansea and NPT and is reviewed on an annual basis. -

Large Print Version (Welsh Or English)
This booklet has been produced by Abertawe Bro Morgannwg University Health Board (ABMU) We would be happy to send you more copies in Welsh or English or in the follow- ing formats: • Braille (Welsh or English) • Talking Book (Welsh or English) • British Sign Language • Easy Read (Welsh or English) • Large print version (Welsh or English) There is a short film about our ideas and much more information on our website www.changingforthebetter.org.uk and YouTube™ as well (ABMULHB channel). You can download more copies of this booklet and copies of other associated documents from the site. For further copies or other formats to be sent to you, please ring our helpline (01792) 704019, email us at [email protected] or write to Changing for the Better team, ABMU, One Talbot Gateway, Baglan Energy Park, Baglan, Port Talbot SA12 7BR Illustration & design G John Rees ABMU Production ABMU Medical Illustration Dept. © ABMU Health Board 2012 3 CONTENTS Who Are We And What Do We Do? ................................................................................ 7 What is This Booklet About And Who Should Read It? .................................... 9 Our Vision For Your Future Healthcare ............................................................................ 10 What Are The Challenges Facing Us? ............................................................................... 14 What We’ve Been Doing So Far ........................................................................................ 22 Working Together With Other Health Boards .............................................................. -

1 Abertawe Bro Morgannwg University Health Board – Annual Report 2018/19
1 Abertawe Bro Morgannwg University Health Board – Annual Report 2018/19 Links included within this Annual Report Annual Quality Statement (AQS) link: Annual Quality Statement Annual Governance Statement/ Accountability Report (AGS) link: Accountability Report including Annual Governance Statement Financial Accounts and Statements Link: Audited Accounts 2018-19 Welsh language version of Annual Report link: Swansea Bay University Health Board (note available after 23.3.19) Web site address link: Swansea Bay University Health Board Email address: [email protected] 2 Abertawe Bro Morgannwg University Health Board – Annual Report 2018/19 Annual Report 2018/19 Contents Foreword Pages 4 - 6 About Abertawe Bro Morgannwg University Health Board Pages 7 - 16 Overview Pages 17 - 19 Primary and Community Services Pages 20 - 26 Mental Health and Learning Disabilities Services Pages 26 - 27 Achievements in 2018/19 Pages 28 - 45 Our People Pages 46 - 52 Performance Analysis Pages 53 - 67 Sustainability Report Pages 68 - 76 Long Term Expenditure Page 77 Finance Report Pages 78 - 89 3 Abertawe Bro Morgannwg University Health Board – Annual Report 2018/19 Chair and Chief Executive Foreword The Board This has been a year of new beginnings with We are delighted to present this, our final Annual changes at executive and non-executive level but, Report as Abertawe Bro Morgannwg University with all but one vacancy now filled, we have a stable Health Board. You will see from the pages that follow and talented Board to guide the organisation through we are incredibly proud of the progress that has been the next year and beyond. There have been many made during 2018/19, but we are also realistic about staff engagement events during the past year which the challenges that remain. -

Independent Review of Fire Precautions at Gorseinon Hospital Brynawel Road Swansea, SA4 4UU
Independent Review of Fire Precautions at Gorseinon Hospital Brynawel Road Swansea, SA4 4UU Stage 1 Report: Prior to Agreement of Action Plan February 2020 Mae'r Gwasanaethau Ystadau Arbenigol yn is-adran o fewn Partneriaeth Cydwasanaethau GIG Cymru Specialist Estates Services is a division of the NHS Wales Shared Services Partnership NWSSP – SPECIALIST ESTATES SERVICES INDEPENDENT REVIEW OF FIRE PRECAUTIONS AT GORSEINON HOSPITAL Brynawel Road, Swansea, SA4 4UU JOB NO: SB/FI/013 - IFR REPORT DATE: February 2020 ORIGINATOR: S Hanger (Signed) Fire Safety Advisor AUTHORISED: S Douglas (Signed) Head of Estate Development CONTENT 1.0 Introduction 1 2.0 Executive Summary 2 3.0 Building Description 4 4.0 Overview of FRA Documentation 5 5.0 Site-Specific Fire Safety Manual 7 6.0 Managerial Controls 9 7.0 Detection and Alarm 15 8.0 Fire Precautions and Means of Escape 19 9.0 Evacuation and Response Procedures 22 10.0 Guidance on Prioritising the Recommendations 26 Appendix A Site Plan Appendix B Prioritised Risk Rating Appendix C Cause & Effect Template 1.0 INTRODUCTION During February 2020, on behalf of the Welsh Government, NWSSP1 – Specialist Estates Services (NWSSP-SES) commenced an independent review of the fire precautions at Gorseinon Hospital, in accordance with the monitoring procedures outlined in FSN12/102. This report sets out the overall findings of that review, which have been established following a combination of a desktop review, site surveys and discussions with the fire management team, ward staff and estates personnel. Whilst the review has focussed on the managerial fire controls and emergency procedures, in addition to examining the main passive and active fire precautions, it is not intended to be a risk assessment. -

2015 UK Parkinson's Audit Reference Report
2015 UK Parkinson’s Audit Reference Report Contents Reference Report 3 Appendix A 87 Definition of phases of Parkinson’s Appendix B 89 Participating services Appendix C 104 Elderly Care and Neurology standards and guidance Appendix D 137 Occupational Therapy standards and guidance Appendix E 167 Physiotherapy standards and guidance Appendix F 188 Speech and Language therapy standards and guidance Appendix G 218 Patient Reported Experience Measure (PREM) questionnaire Appendix H 223 PREM - Qualitative report on free-text comments Appendix I 243 Acknowledgements Foreword The 2015 Parkinson’s Audit provides the largest dataset yet obtained about the quality of care provided to people with Parkinson’s across the UK. The unprecedented level of participation in the 2015 audit demonstrates the dedication and commitment of UK doctors, nurses, occupational therapists, physiotherapists and speech and language therapists to improving services for people with Parkinson’s. As in 2012, this summary report highlights that healthcare professionals are working to evidence-based standards and it confirms many areas of good practice. For the first time the views of people with Parkinson’s have been gathered as part of the audit process and their responses back up evidence of good practice. For example, 73% of respondents felt that the number of times that they were reviewed by their Consultant met their needs. Furthermore, an overwhelming number of comments made about the quality of service received were positive. But this report shows that there are still important areas for improvement. For example, only 50% of patients reported getting their medication consistently on time whilst in hospital. -

ABMU LHB Year End Accounts
ABERTAWE BRO MORGANNWG UNIVERSITY LOCAL HEALTH BOARD ANNUAL ACCOUNTS 2009-10 Abertawe Bro Morgannwg University Local Health Board FOREWORD These accounts have been prepared by the Local Health Board under schedule 9 section 178 Para 3(1) of the National Health Service (Wales) Act 2006 (c.42) in the form in which the Welsh Ministers have, with the approval of the Treasury, directed. Statutory background The Local Health Board was established on 1 October 2009 following the merger of Abertawe Bro Morgannwg Iniversity NHS Trust and Swansea, Bridgend and Neath Port Talbot Local Health Boards All the bodies which were in existence have prepared a set of statutory accounts for their final six month period from 1 April 2009 to 30 September 2009. The LHB is required to prepare a set of accounts for the accounting year 2009-10 in accordance with the HM Treasury's Financial Reporting Manual Section 4.2.18 on a merger accounting basis. This requires the account to be prepared as if the new LHB had existed in its post 1 October 2009 configuration for the full 12 month period and for prior period comparators to be reported with these accounts. Performance Management and Financial Results Local Health Boards in Wales must comply fully with the Treasury's Financial Reporting Manual to the extent that it is applicable to them. As a result the Primary Statement of in-year income and expenditure is the Operating Cost Statement, which shows the net operating cost incurred by the LHB which is funded by the Assembly. This funding is allocated on receipt directly to the General Fund in the Balance Sheet. -
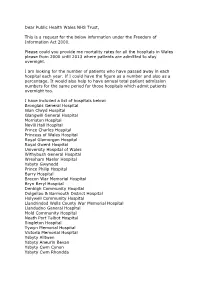
Dear Public Health Wales NHS Trust, This Is a Request for the Below
Dear Public Health Wales NHS Trust, This is a request for the below information under the Freedom of Information Act 2000. Please could you provide me mortality rates for all the hospitals in Wales please from 2000 until 2013 where patients are admitted to stay overnight. I am looking for the number of patients who have passed away in each hospital each year. If I could have the figure as a number and also as a percentage. It would also help to have annual total patient admission numbers for the same period for those hospitals which admit patients overnight too. I have included a list of hospitals below: Bronglais General Hospital Glan Clwyd Hospital Glangwili General Hospital Morriston Hospital Nevill Hall Hospital Prince Charles Hospital Princess of Wales Hospital Royal Glamorgan Hospital Royal Gwent Hospital University Hospital of Wales Withybush General Hospital Wrexham Maelor Hospital Ysbyty Gwynedd Prince Philip Hospital Barry Hospital Brecon War Memorial Hospital Bryn Beryl Hospital Denbigh Community Hospital Dolgellau & Barmouth District Hospital Holywell Community Hospital Llandrindod Wells County War Memorial Hospital Llandudno General Hospital Mold Community Hospital Neath Port Talbot Hospital Singleton Hospital Tywyn Memorial Hospital Victoria Memorial Hospital Ysbyty Alltwen Ysbyty Aneurin Bevan Ysbyty Cwm Cynon Ysbyty Cwm Rhondda Ysbyty Penrhos Stanley Ysbyty Ystrad Fawr Ystradgynlais Community Hospital Pontypridd & District Cottage Hospital (Y Bwthyn) St. Woolos Hospital CHC Local Committee Carmarthenshire Local Committee -

Llynfi Ward, Maesteg Community Hospital and West Ward, Gorseinon Hospital
Hospital Inspection (Unannounced) Abertawe Bro Morgannwg University Health Board: Llynfi Ward, Maesteg Community Hospital and West Ward, Gorseinon Hospital Inspection date: 27 and 28 September 2016 Publication date: 29 December 2016 This publication and other HIW information can be provided in alternative formats or languages on request. There will be a short delay as alternative languages and formats are produced when requested to meet individual needs. Please contact us for assistance. Copies of all reports, when published, will be available on our website or by contacting us: In writing: Communications Manager Healthcare Inspectorate Wales Welsh Government Rhydycar Business Park Merthyr Tydfil CF48 1UZ Or via Phone: 0300 062 8163 Email: [email protected] Fax: 0300 062 8387 Website: www.hiw.org.uk Digital ISBN 978-1-4734-7952-4 © Crown copyright 2016 Contents 1. Introduction ........................................................................................................ 2 2. Methodology....................................................................................................... 2 3. Context ............................................................................................................... 5 4. Summary ............................................................................................................ 6 5. Findings ............................................................................................................. 9 Quality of the Patient Experience ..................................................................... -

Updated: July 2021 Organisation Team Name and Hospitals Covered
Updated: July 2021 Organisation Team Name and Hospitals Covered Status Swansea Department of Liaison Psychiatry Swansea Bay University Health Morriston Hospital, Swansea; Singleton Hospital, Swansea; Accredited Board Neath Port Talbot Hospital; Baglan and Gorseinon Hospital, Valid until 03/12/21 Swansea Avon & Wiltshire Mental Health Great Western Hospital Mental Health Liaison Service Members Partnership NHS Trust Great Western Hospital, Swindon Barnet, Enfield and Haringey Barnet Hospital Mental Health Liaison Service Accredited Mental Health NHS Trust Barnet Hospital Valid until 08/04/22 Berkshire Healthcare NHS Royal Berkshire Hospital Psychological Medicine Service Accredited Foundation Trust Royal Berkshire Hospital Valid until 15/12/22 Berkshire Healthcare NHS East Berkshire Psychological Medicine Accredited Foundation Trust Wexham Park Hospital Valid until 15/12/22 Birmingham and Solihull Mental Birmingham City Hospital Liaison Psychiatry Team Accredited Health NHS Foundation Trust Birmingham City Hospital Valid until 15/03/23 Birmingham and Solihull Mental Good Hope Hospital Liaison Psychiatry Team Accredited Health NHS Foundation Trust Good Hope Hospital Valid until 17/09/21 Birmingham and Solihull Mental Heartlands Liaison Psychiatry Team Not Accredited Health NHS Foundation Trust Heartlands Hospital Queen Elizabeth Hospital, Birmingham, Liaison Psychiatry Birmingham and Solihull Mental Team Not Accredited Health NHS Foundation Trust Queen Elizabeth Hospital Birmingham Updated: July 2021 Cambridge and Peterborough Addenbrooke's -

Swansea Department of Liaison Psychiatry
Updated April 2020 Organisation Team Name and Hospitals Covered Status Swansea Department of Liaison Psychiatry Swansea Bay University Morriston Hospital, Swansea; Singleton Hospital, Accredited Health Board Swansea; Neath Port Talbot Hospital; Baglan and Gorseinon Hospital, Swansea Great Western Hospital Mental Health Liaison Avon & Wiltshire Mental Health Service Accredited Partnership NHS Trust Great Western Hospital, Swindon Barnet, Enfield and Haringey North Middlesex Mental Health Liaison Service Members Mental Health NHS Trust North Middlesex University Hospital Barnet, Enfield and Haringey Barnet Hospital Mental Health Liaison Service Accredited Mental Health NHS Trust Barnet Hospital Royal Berkshire Hospital Psychological Medicine Berkshire Healthcare NHS Service Members Foundation Trust Royal Berkshire Hospital Berkshire Healthcare NHS East Berkshire Psychological Medicine Accredited Foundation Trust Wexham Park Hospital Birmingham and Solihull Birmingham City Hospital Liaison Psychiatry Mental Health NHS Foundation Team Accredited Trust Birmingham City Hospital Birmingham and Solihull Good Hope Hospital Liaison Psychiatry Team Mental Health NHS Foundation Accredited Good Hope Hospital Trust Birmingham and Solihull Solihull Hospital Liaison Psychiatry Team Mental Health NHS Foundation Not Accredited Solihull Hospital Trust Updated April 2020 Birmingham and Solihull Heartlands Liaison Psychiatry Team Mental Health NHS Foundation Not Accredited Heartlands Hospital Trust Birmingham and Solihull Queen Elizabeth Hospital, Birmingham, -

Updated September 2020 Organisation Team Name And
Updated September 2020 Organisation Team Name and Hospitals Covered Status Swansea Department of Liaison Psychiatry Swansea Bay University Health Morriston Hospital, Swansea; Singleton Hospital, Swansea; Accredited Board Neath Port Talbot Hospital; Baglan and Gorseinon Hospital, Valid until 03/12/21 Swansea Avon & Wiltshire Mental Health Great Western Hospital Mental Health Liaison Service Accredited Partnership NHS Trust Great Western Hospital, Swindon Valid until 21/09/20 Barnet, Enfield and Haringey North Middlesex Mental Health Liaison Service Members Mental Health NHS Trust North Middlesex University Hospital Barnet, Enfield and Haringey Barnet Hospital Mental Health Liaison Service Accredited Mental Health NHS Trust Barnet Hospital Valid until 08/04/22 Berkshire Healthcare NHS Royal Berkshire Hospital Psychological Medicine Service Accredited Foundation Trust Royal Berkshire Hospital Valid until 15/12/22 Berkshire Healthcare NHS East Berkshire Psychological Medicine Accredited Foundation Trust Wexham Park Hospital Valid until 15/12/222 Birmingham and Solihull Mental Birmingham City Hospital Liaison Psychiatry Team Members Health NHS Foundation Trust Birmingham City Hospital Birmingham and Solihull Mental Good Hope Hospital Liaison Psychiatry Team Accredited Health NHS Foundation Trust Good Hope Hospital Valid until 17/09/21 Birmingham and Solihull Mental Solihull Hospital Liaison Psychiatry Team Not Accredited Health NHS Foundation Trust Solihull Hospital Updated September 2020 Birmingham and Solihull Mental Heartlands Liaison Psychiatry -

50 Years of the NHS in Wales.Pdf
CONTENTS Preface ........ .......... .. ............... .......... ... ... ... ..... " ... ................... ..... .. 5 Acknowledgements ........... 6 Chapter 1 Introduction .................. .. ................. ...... .................... 7 Chapter 2 Pre 1948: The legacy of the Past ........................ ... .. ..... 9-35 THE HISTORICAL PERSPECTIVE Voluntary Hospitals ..... .. ................ ....... .. 10 Municipal Hospitals .. 11 11 .,' Mr Delme Griffiths and Welsh Health Esrares, 1998 Poor Law Institutions ................... Isolation Hospitals: the spectre of epidemics ................... ... ...... 13 From Lunatic Asylums to Mental Hospitals .......... ........... ..... .. 14 THE GENESIS OF HOSPITALS IN WALES Firsr Published 1998 by Welsh Health Esrares A Tradition of Care ............... ................. ................. ........ ... .... 16 Voluntary Hospitals Take the Lead .... ........................... ... ... ... 16 All Rights Reserved. No parr of this publicarion may be reproduced, srored in a Municipal Hospitals Follow On ....... .. .... ... ........ .... .. ........... .... 19 retrieval sysrem, or transmirred, in any fonn or by any means, electronic, General Acute Hospitals .. .......... ........ ............. .... .... .. ... ....... 19 mechanical, phorocopying, recording or otherwise without the prior pennission of Infectious Diseases Hospitals .............. .................. ..... ......... 24 Mental Health Hospitals . .... ..... .................... .... ....... ... 27 the copyright owner. The Role of