Dissecting a Role for Polyamines in Rift Valley Fever Virus Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Zika Virus Envelope Mutation Preceding the 2015 Epidemic Enhances Virulence and Fitness for Transmission
A Zika virus envelope mutation preceding the 2015 epidemic enhances virulence and fitness for transmission Chao Shana,b,1,2, Hongjie Xiaa,1, Sherry L. Hallerc,d,e, Sasha R. Azarc,d,e, Yang Liua, Jianying Liuc,d, Antonio E. Muruatoc, Rubing Chenc,d,e,f, Shannan L. Rossic,d,f, Maki Wakamiyaa, Nikos Vasilakisd,f,g,h,i, Rongjuan Peib, Camila R. Fontes-Garfiasa, Sanjay Kumar Singhj, Xuping Xiea, Scott C. Weaverc,d,e,k,l,2, and Pei-Yong Shia,d,e,k,l,2 aDepartment of Biochemistry and Molecular Biology, University of Texas Medical Branch, Galveston, TX 77555; bState Key Laboratory of Virology, Wuhan Institute of Virology, Chinese Academy of Sciences, 430071 Wuhan, China; cDepartment of Microbiology and Immunology, University of Texas Medical Branch, Galveston, TX 77555; dInstitute for Human Infections and Immunity, University of Texas Medical Branch, Galveston, TX 77555; eInstitute for Translational Science, University of Texas Medical Branch, Galveston, TX 77555; fDepartment of Pathology, University of Texas Medical Branch, Galveston, TX 77555; gWorld Reference Center of Emerging Viruses and Arboviruses, University of Texas Medical Branch, Galveston, TX 77555; hCenter for Biodefence and Emerging Infectious Diseases, University of Texas Medical Branch, Galveston, TX 77555; iCenter for Tropical Diseases, University of Texas Medical Branch, Galveston, TX 77555; jDepartment of Neurosurgery-Research, The University of Texas MD Anderson Cancer Center, Houston, TX 77030; kSealy Institute for Vaccine Sciences, University of Texas Medical Branch, Galveston, TX 77555; and lSealy Center for Structural Biology and Molecular Biophysics, University of Texas Medical Branch, Galveston, TX 77555 Edited by Peter Palese, Icahn School of Medicine at Mount Sinai, New York, NY, and approved July 2, 2020 (received for review March 26, 2020) Arboviruses maintain high mutation rates due to lack of proof- recently been shown to orchestrate flavivirus assembly through reading ability of their viral polymerases, in some cases facilitating recruiting structural proteins and viral RNA (8, 9). -

Following Acute Encephalitis, Semliki Forest Virus Is Undetectable in the Brain by Infectivity Assays but Functional Virus RNA C
viruses Article Following Acute Encephalitis, Semliki Forest Virus is Undetectable in the Brain by Infectivity Assays but Functional Virus RNA Capable of Generating Infectious Virus Persists for Life Rennos Fragkoudis 1,2, Catherine M. Dixon-Ballany 1, Adrian K. Zagrajek 1, Lukasz Kedzierski 3 and John K. Fazakerley 1,3,* ID 1 The Roslin Institute and Royal (Dick) School of Veterinary Studies, College of Medicine & Veterinary Medicine, University of Edinburgh, Edinburgh, Midlothian EH25 9RG, UK; [email protected] (R.F.); [email protected] (C.M.D.-B.); [email protected] (A.K.Z.) 2 The School of Veterinary Medicine and Science, the University of Nottingham, Sutton Bonington Campus, Leicestershire LE12 5RD, UK 3 Department of Microbiology and Immunology, Faculty of Medicine, Dentistry and Health Sciences at The Peter Doherty Institute for Infection and Immunity and the Melbourne Veterinary School, Faculty of Veterinary and Agricultural Sciences, the University of Melbourne, 792 Elizabeth Street, Melbourne 3000, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-3-9731-2281 Received: 25 April 2018; Accepted: 17 May 2018; Published: 18 May 2018 Abstract: Alphaviruses are mosquito-transmitted RNA viruses which generally cause acute disease including mild febrile illness, rash, arthralgia, myalgia and more severely, encephalitis. In the mouse, peripheral infection with Semliki Forest virus (SFV) results in encephalitis. With non-virulent strains, infectious virus is detectable in the brain, by standard infectivity assays, for around ten days. As we have shown previously, in severe combined immunodeficient (SCID) mice, infectious virus is detectable for months in the brain. -

Replication of Semliki Forest Virus: Polyadenylate in Plus- Strand RNA and Polyuridylate in Minus-Strand RNA
JOURNAL OF VIROLOGY, Nov. 1976, p. 446-464 Vol. 20, No. 2 Copyright X) 1976 American Society for Microbiology Printed in U.S.A. Replication of Semliki Forest Virus: Polyadenylate in Plus- Strand RNA and Polyuridylate in Minus-Strand RNA DOROTHEA L. SAWICKI* AND PETER J. GOMATOS Division of Virology, The Sloan-Kettering Institute, New York, New York 10021 Received for publication 4 June 1976 The 42S RNA from Semliki Forest virus contains a polyadenylate [poly(A)] sequence that is 80 to 90 residues long and is the 3'-terminus of the virion RNA. A poly(A) sequence of the same length was found in the plus strand of the replicative forms (RFs) and replicative intermediates (RIs) isolated 2 h after infection. In addition, both RFs and RIs contained a polyuridylate [poly(U)] sequence. No poly(U) was found in virion RNA, and thus the poly(U) sequence is in minus-strand RNA. The poly(U) from RFs was on the average 60 residues long, whereas that isolated from the RIs was 80 residues long. Poly(U) sequences isolated from RFs and RIs by digestion with RNase Ti contained 5'-phosphoryl- ated pUp and ppUp residues, indicating that the poly(U) sequence was the 5'- terminus of the minus-strand RNA. The poly(U) sequence in RFs or RIs was free to bind to poly(A)-Sepharose only after denaturation of the RNAs, indicating that the poly(U) was hydrogen bonded to the poly(A) at the 3'-terminus of the plus-strand RNA in these molecules. When treated with 0.02 g.g of RNase A per ml, both RFs and RIs yielded the same distribution of the three cores, RFI, RFII, and RFIII. -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Notification Requirements
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2021 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of within the next reporting cycle. a case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 Approved by CSTE: June 2019 within 24 hours of a case meeting the notification criteria, followed by Interim Update Approved by CSTE: April 5, 2020 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2020 electronic transmission. Updated: May 28, 2020 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Page 1 of 5 Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis -

2018 DSHS Arbovirus Activity
Health and Human Texas Department of State Services Health Services Arbovirus Activity in Texas 2018 Surveillance Report August 2019 Texas Department of State Health Services Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California (CAL) serogroup viruses, chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2018, reported human arboviral disease cases were attributed to WNV (82%), DENV (11%), CHIKV (4%), ZIKV (2%), and CAL (1%) (Table 1). In addition, there were two cases reported as arbovirus disease cases which could not be diagnostically or epidemiologically differentiated between DENV and ZIKV. Animal infections or disease caused by WNV and SLEV were also reported during 2018. Local transmission of DENV, SLEV, and WNV was documented during 2018 (Figure 1). No reports of EEEV or WEEV were received during 2018. Table 1. Year-End Arbovirus Activity Summary, Texas, 2018 Positive Human* Arbovirus Mosquito Avian Equine TOTAL TOTAL Fever Neuroinvasive Severe Deaths PVD‡ Pools (Human) CAL 1 1 1 CHIK 7 7 7 DEN 20 20 20 SLE 2 0 2 WN 1,021 6 19 38 108 146 11 24 1,192 Zika** 4 4 TOTAL 1,023 6 19 65 109 0 178 11 24 1,226 CAL - California serogroup includes California encephalitis, Jamestown Canyon, Keystone, La Crosse, Snowshoe hare and Trivittatus viruses CHIK - Chikungunya DEN - Dengue SLE - Saint Louis encephalitis WN - West Nile ‡PVD - Presumptive viremic blood donors are people who had no symptoms at the time of donating blood through a blood collection agency, but whose blood tested positive when screened for the presence of West Nile virus or Zika virus. -
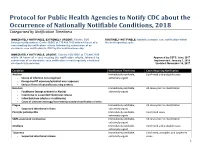
Protocol for Public Health Agencies to Notify CDC About the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification within Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of a the next reporting cycle. case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 within 24 hours of a case meeting the notification criteria, followed by Approved by CSTE: June 2017 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2018 electronic transmission. Updated: November 16, 2017 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis Immediately notifiable, Confirmed cases extremely -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -

Identification of Novel Antiviral Compounds Targeting Entry Of
viruses Article Identification of Novel Antiviral Compounds Targeting Entry of Hantaviruses Jennifer Mayor 1,2, Giulia Torriani 1,2, Olivier Engler 2 and Sylvia Rothenberger 1,2,* 1 Institute of Microbiology, University Hospital Center and University of Lausanne, Rue du Bugnon 48, CH-1011 Lausanne, Switzerland; [email protected] (J.M.); [email protected] (G.T.) 2 Spiez Laboratory, Swiss Federal Institute for NBC-Protection, CH-3700 Spiez, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +41-21-314-51-03 Abstract: Hemorrhagic fever viruses, among them orthohantaviruses, arenaviruses and filoviruses, are responsible for some of the most severe human diseases and represent a serious challenge for public health. The current limited therapeutic options and available vaccines make the development of novel efficacious antiviral agents an urgent need. Inhibiting viral attachment and entry is a promising strategy for the development of new treatments and to prevent all subsequent steps in virus infection. Here, we developed a fluorescence-based screening assay for the identification of new antivirals against hemorrhagic fever virus entry. We screened a phytochemical library containing 320 natural compounds using a validated VSV pseudotype platform bearing the glycoprotein of the virus of interest and encoding enhanced green fluorescent protein (EGFP). EGFP expression allows the quantitative detection of infection and the identification of compounds affecting viral entry. We identified several hits against four pseudoviruses for the orthohantaviruses Hantaan (HTNV) and Citation: Mayor, J.; Torriani, G.; Andes (ANDV), the filovirus Ebola (EBOV) and the arenavirus Lassa (LASV). Two selected inhibitors, Engler, O.; Rothenberger, S. -

Chikungunya Vaccine Candidates Elicit Protective Immunity in C57BL/6 Mice
Novel attenuated chikungunya vaccine candidates elicit protective immunity in C57BL/6 mice Author Hallengard, David, Kakoulidou, Maria, Lulla, Aleksei, Kummerer, Beate M., Johansson, Daniel X., Mutso, Margit, Lulla, Valeria, Fazakerley, John K., Roques, Pierre, Le Grand, Roger, Merits, Andres, Liljestrom, Peter Published 2014 Journal Title Journal of Virology Version Version of Record (VoR) DOI https://doi.org/10.1128/JVI.03453-13 Copyright Statement © 2013 American Society for Microbiology. The attached file is reproduced here in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/343708 Griffith Research Online https://research-repository.griffith.edu.au Novel Attenuated Chikungunya Vaccine Candidates Elicit Protective Immunity in C57BL/6 mice David Hallengärd,a Maria Kakoulidou,a Aleksei Lulla,b Beate M. Kümmerer,c Daniel X. Johansson,a Margit Mutso,b Valeria Lulla,b John K. Fazakerley,d Pierre Roques,e,f Roger Le Grand,e,f Andres Merits,b Peter Liljeströma Department of Microbiology, Tumor and Cell Biology, Karolinska Institutet, Stockholm, Swedena; Institute of Technology, University of Tartu, Tartu, Estoniab; Institute of Virology, University of Bonn Medical Centre, Bonn, Germanyc; The Pirbright Institute, Pirbright, United Kingdomd; Division of Immuno-Virology, iMETI, CEA, Paris, Francee; UMR-E1, University Paris-Sud XI, Orsay, Francef ABSTRACT Chikungunya virus (CHIKV) is a reemerging mosquito-borne alphavirus that has caused severe epidemics in Africa and Asia and occasionally in Europe. As of today, there is no licensed vaccine available to prevent CHIKV infection. Here we describe the development and evaluation of novel CHIKV vaccine candidates that were attenuated by deleting a large part of the gene encod- ing nsP3 or the entire gene encoding 6K and were administered as viral particles or infectious genomes launched by DNA. -

DSHS Arbovirus Activity 061817
Arbovirus Activity in Texas 2017 Surveillance Report June 2018 Texas Department of State Health Services Infectious Disease Control Unit Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California serogroup viruses (CAL), chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2017, reported human arboviral disease cases were attributed to WNV (54%), ZIKV (22%), DENV (17%), and CHIKV (6%) (Table 1). Animal infections or disease caused by CAL, EEEV, SLEV, and WNV were also reported during 2017. Table 1. Year-End Arbovirus Activity Summary, Texas, 2017 California Serogroup Viruses California serogroup viruses (CAL) are bunyaviruses and include California encephalitis virus (CEV), Jamestown Canyon virus, Keystone virus, La Crosse virus (LACV), snowshoe hare virus, and Trivittatus virus. These viruses are maintained in a cycle between mosquito vectors and vertebrate hosts in forest habitats. In the United States (U.S.), approximately 80-100 reported cases of human neuroinvasive disease are caused by LACV each year (CDC), mostly in mid-Atlantic and southeastern states. From 2002-2016, Texas reported a total of 5 cases of human CAL disease (range: 0-3 cases/year): 1 case of CEV neuroinvasive disease and 4 cases of LACV neuroinvasive disease. In 2017, one CEV-positive mosquito pool was identified in Orange County (Figure 1); no human cases of CAL disease were reported. -

Early Events in Chikungunya Virus Infection—From Virus Cell Binding to Membrane Fusion
Viruses 2015, 7, 3647-3674; doi:10.3390/v7072792 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review Early Events in Chikungunya Virus Infection—From Virus Cell Binding to Membrane Fusion Mareike K. S. van Duijl-Richter, Tabitha E. Hoornweg, Izabela A. Rodenhuis-Zybert and Jolanda M. Smit * Department of Medical Microbiology, University of Groningen and University Medical Center Groningen, 9700 RB Groningen, The Netherlands; E-Mails: [email protected] (M.K.S.D.-R.); [email protected] (T.E.H.); [email protected] (I.A.R.-Z.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +31-50-3632738. Academic Editors: Yorgo Modis and Stephen Graham Received: 4 May 2015 / Accepted: 29 June 2015 / Published: 7 July 2015 Abstract: Chikungunya virus (CHIKV) is a rapidly emerging mosquito-borne alphavirus causing millions of infections in the tropical and subtropical regions of the world. CHIKV infection often leads to an acute self-limited febrile illness with debilitating myalgia and arthralgia. A potential long-term complication of CHIKV infection is severe joint pain, which can last for months to years. There are no vaccines or specific therapeutics available to prevent or treat infection. This review describes the critical steps in CHIKV cell entry. We summarize the latest studies on the virus-cell tropism, virus-receptor binding, internalization, membrane fusion and review the molecules and compounds that have been described to interfere with virus cell entry. The aim of the review is to give the reader a state-of-the-art overview on CHIKV cell entry and to provide an outlook on potential new avenues in CHIKV research.