Development and Validation of a Clinical Risk Score to Predict SARS-Cov-2 Infection in Emergency Department Patients: the CCEDRRN COVID-19 Infection Score (CCIS)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rop 2019-2020
RECORD OF PROCEEDINGS May 28, 2019 – October 18, 2020 The United Church of Canada Shining Waters Regional Council 2019/2020 – i Table of Contents PASTORAL RELATIONS COMMISSION, May 28, 2019 .................................................................................. 1 COMMUNITIES OF FAITH COMMISSION, June 18, 2019 ............................................................................... 4 PASTORAL RELATIONS COMMISSION, June 18, 2019 ................................................................................ 13 EXECUTIVE, June 20, 2019 ......................................................................................................................... 25 EXECUTIVE, July 24, 2019 ............................................................................................................................ 28 COMMUNITIES OF FAITH COMMISSION, August 22, 2019 ......................................................................... 31 PASTORAL RELATIONS COMMISSION, August 27, 2019 ............................................................................ 33 EXECUTIVE, August 28, 2019 ...................................................................................................................... 40 COMMUNITIES OF FAITH COMMISSION, September 18, 2019 ................................................................. 42 PASTORAL RELATIONS COMMISSION, September 24, 2019 ...................................................................... 49 SOCIAL AND ECOLOGICAL JUSTICE COMMISSION, October 9, 2019 ......................................................... -

Annual Report2019-20
UNITY HEALTH TORONTO Annual Report 2019-20 ST. JOSEPH’S HEALTH CENTRE ST. MICHAEL’S HOSPITAL PROVIDENCE HEALTHCARE Message from our When Unity Health Toronto launched its first St. Michael’s Hospital, that enhanced system capacity strategic plan last spring, we unveiled a new vision when our city needed it the most. With the requirement President and CEO of what we aspire to deliver for everyone we serve: The of visitor restriction policies and ramping down of best care experiences. Created together. All of our clinical services, we implemented virtual solutions to and Board Chair dreaming and planning resulted in identifying strategic enable people to connect with their loved ones or to areas of focus that are interrelated and move us steadily access care from home. towards our shared vision. None of our accomplishments would have been Though we experienced unprecedented change in possible without us all working together and we are the final months of this year as we responded to the incredibly proud that our people have continued to live COVID-19 pandemic, we wanted to take this opportunity our mission and values during this unprecedented time to reflect on the great progress our teams made in in health care, locally and around the world. achieving our Year 1 strategic objectives before we We are so grateful for the many contributions of our turned our efforts to this new virus. Throughout this Unity Health community through the past year and report you will see stories that show how we have during this pandemic. As we go forward and begin our been building the foundation to create the best care recovery, we will continue to be guided by our vision experiences together. -

Master of Public Policy Class of 2020
Candidate Profiles MCaasntedr oidf Pautbelic PPorloicyfiles MClasste orf o2f0 P2u0blic Policy Class of 2019 Candidate List Student Profiles for the Master of Public Policy Class of 2020 Page 3 Lamia Aganagic Page 45 Nilanee Koneswaran Page 4 Saif-U-Din Alnuweiri Page 46 Rikin Kotak Page 5 Erin Anderson-Birmingham Page 47 Natalie Krzywiecki Page 6 Aryeh Ansel Page 48 Nemesha Kukan Page 7 Victoria Antinucci Page 49 Arpit Kumar Page 8 Shir Barzilay Page 50 Matthew Kupferschmidt Page 9 Jennifer Bocti Page 51 Adam Laughton Page 10 Aidan Carroll Page 52 Lin Ying Lin Page 11 Clarence Chan Page 53 Katherine Lordon Page 12 Jennifer Chew Page 54 Saurav Maini Page 13 Joshua Cho Page 55 Daniella Marciano Page 14 Catherine Clasadonte Page 56 Chloe Marcil Page 15 Chelsea Clifford Page 57 Megan Mattes Page 16 Carly Cook Page 58 Anna Millar Page 17 Olivia Courneya Page 59 Benjamin Miller Page 18 Alexandra De Rosa Page 60 Madison Newton Page 19 Caitlyn Dwyer Page 61 Samantha Nguyen Page 20 Evguenia Ermakova Page 62 Vienna O'Shea Page 21 Arsalan Esmaeili Page 63 Madhav Panday Page 22 Dean Evangeliou Page 64 Ryan Phillips Page 23 Caroline Ewen Page 65 Matthew Quance Page 24 Andre Fast Page 66 Shalini Ramgoolam Page 25 Jolene Funk Page 67 Cherise Regier Page 26 Maya Gajic Page 68 Rachel Robinson Page 27 Natalie Gdyczynski Page 69 Victoria Santos Page 28 Robert Giannetta Page 70 Donya Taghizadeh Page 29 Aneet Gill Page 71 Genevieve Tallmeister Page 30 Luka Glozic Page 72 Sandy Tat Page 31 Alexander Gold-Apel Page 73 Melisa Tica Page 32 Timothy Gopaul Page -

2020-21 STUDENT-ATHLETE HANDBOOK Your Mental Health Is Important!
VARSITY BLUES 2020-21 STUDENT-ATHLETE HANDBOOK Your mental health is important! In any given year, 1 in 5 Canadians experience a mental health illness* Mental Health Resources For YOU EMBEDDED COUNSELLOR U OF T MY SSP GOOD 2 TALK Book your confidential appointment Talk to Someone Right Now with 24/7 After hours? Always available 24 with Health & Wellness: Emergency Counseling Services: hours a day 416-978-8030 (Option 5) - Identify yourself My SSP: 1-844-451-9700 as a varsity athlete. Outside North America: 001-416-380- 6578 *According to CAMH Centre for Addiction and Mental Health ii | Student-Athlete Handbook 2020–21 Table of Contents Varsity Blues Student-Athlete Rights 4 Section 1 A Tradition of Excellence 5 Section 2 Intercollegiate and High Performance Sport Model 7 Section 3 Varsity Blues Expectations of Behaviour 9 Section 4 Eligibility 17 Section 5 Student-Athlete Services 19 Section 6 Athletic Scholarships and Financial Aid Awards 24 Section 7 Intercollegiate Program - Appeal Procedures 26 Section 8 Health Care 28 Section 9 Leadership and Governance 30 Section 10 Frequently Asked Questions 31 Safety Information for Students, Staff and Faculty 32 Helpful University Resources 33 Important Numbers Executive Director of Athletics Assistant Manager, Student-Athlete Services Mental Health Resources For YOU (Athletic Director) Steve Manchur Beth Ali 416-946-0807 416-978-7379 [email protected] [email protected] Manager, Marketing and Events Manager, Intercollegiate Sport Mary Beth Challoner Melissa Krist 416-946-5131 416-946-3712 [email protected] [email protected] Coordinator, Athletic Communications Assistant Manager, Intercollegiate Jill Clark Blue & White and Club Sports 416-978-4263 Kevin Sousa [email protected] 416-978-5431 [email protected] Student-Athlete Handbook 2020–21 | 1 About the University of Toronto The University of Toronto was founded as King’s College in 1827 and has evolved into a large and complex institution. -

Position: Developmental Pediatrician (0.8FTE), St. Michael's Hospital, Unity Health Toronto, Toronto on the Successful Candidat
Position: Developmental Pediatrician (0.8FTE), St. Michael's Hospital, Unity Health Toronto, Toronto ON The successful candidate would be expected to provide outpatient diagnostic and treatment services as part of the Developmental Pediatric Team associated with Unity Health Toronto, focusing on inner city populations and outreach services. The Developmental Pediatrics clinics at St. Michael’s Hospital provide care at various clinical sites in the downtown Toronto area for the diagnosis and treatment of neurodevelopmental disorders. These sites include Unity Health Toronto affiliated clinics, as well as onsite clinical care through community partners, such as community health centres and inner-city schools. The Department of Pediatrics provides services from infancy through adolescence, for individuals who are referred with complex neurodevelopmental disorders, including autism spectrum disorder, medical and genetic conditions, intellectual disabilities, and learning, attentional, and behavioral disorders. The Department has a large, well-developed clinical research infrastructure in partnership with the Li Ka Shing Knowledge Institute and University of Toronto. The successful candidate will be required to actively participate in clinical, public health and/or basic research, in keeping with the missions and values of Unity Health Toronto. The position involves active participation in the medical education of Developmental Pediatrics fellows, pediatric/family medicine residents and University of Toronto medical students. The Department of Pediatrics at St. Michael’s Hospital is dedicated to promoting research, teaching, and service innovations designed to improve the lives of children, adolescents, and families. St. Michael’s Hospital is a part of Unity Health Toronto, which is a Catholic health care organization providing compassionate physical, emotional and spiritual care to all in need. -
Welcome Guide
GRADUATE STUDENTS & POSTDOCTORAL FELLOWS WELCOME GUIDE 2019 - 2020 TABLE OF CONTENTS CHAPTER 1: WELCOME CHAPTER 2: GET TO KNOW THE RTC, TRAINEE ASSOCIATIONS AND THE RESEARCH INSTITUTE 1.0 What is the Research Training Centre? .................................................................................................................11 1.1 What does the RTC do? .......................................................................................................................................... 11 1.2 RTC Team ................................................................................................................................................................ 12 1.2.1 RTC Co-directors ............................................................................................................................................. 12 1.2.2 RTC Coordinator .............................................................................................................................................. 13 1.2.3 RTC Program Administrator ............................................................................................................................ 14 1.3 Our website ............................................................................................................................................................ 14 2.0 SRSA.....................................................................................................................................................................14 3.0 PDF Association ...................................................................................................................................................16 -
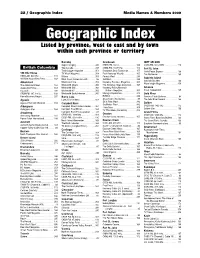
Geographic Index Media Names & Numbers 2009 Geographic Index Listed by Province, West to East and by Town Within Each Province Or Territory
22 / Geographic Index Media Names & Numbers 2009 Geographic Index Listed by province, west to east and by town within each province or territory Burnaby Cranbrook fORT nELSON Super Camping . 345 CHDR-FM, 102.9 . 109 CKRX-FM, 102.3 MHz. 113 British Columbia Tow Canada. 349 CHBZ-FM, 104.7mHz. 112 Fort St. John Truck Logger magazine . 351 Cranbrook Daily Townsman. 155 North Peace Express . 168 100 Mile House TV Week Magazine . 354 East Kootenay Weekly . 165 The Northerner . 169 CKBX-AM, 840 kHz . 111 Waters . 358 Forests West. 289 Gabriola Island 100 Mile House Free Press . 169 West Coast Cablevision Ltd.. 86 GolfWest . 293 Gabriola Sounder . 166 WestCoast Line . 359 Kootenay Business Magazine . 305 Abbotsford WaveLength Magazine . 359 The Abbotsford News. 164 Westworld Alberta . 360 The Kootenay News Advertiser. 167 Abbotsford Times . 164 Westworld (BC) . 360 Kootenay Rocky Mountain Gibsons Cascade . 235 Westworld BC . 360 Visitor’s Magazine . 305 Coast Independent . 165 CFSR-FM, 107.1 mHz . 108 Westworld Saskatchewan. 360 Mining & Exploration . 313 Gold River Home Business Report . 297 Burns Lake RVWest . 338 Conuma Cable Systems . 84 Agassiz Lakes District News. 167 Shaw Cable (Cranbrook) . 85 The Gold River Record . 166 Agassiz/Harrison Observer . 164 Ski & Ride West . 342 Golden Campbell River SnoRiders West . 342 Aldergrove Campbell River Courier-Islander . 164 CKGR-AM, 1400 kHz . 112 Transitions . 350 Golden Star . 166 Aldergrove Star. 164 Campbell River Mirror . 164 TV This Week (Cranbrook) . 352 Armstrong Campbell River TV Association . 83 Grand Forks CFWB-AM, 1490 kHz . 109 Creston CKGF-AM, 1340 kHz. 112 Armstrong Advertiser . 164 Creston Valley Advance. -

Cohort Profile: St. Michael's Hospital Tuberculosis Database (SMH-TB)
medRxiv preprint doi: https://doi.org/10.1101/2020.09.11.20192419; this version posted September 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY 4.0 International license . PLOS ONE Submission Landsman et al. 1 Cohort profile: St. Michael’s Hospital Tuberculosis Database (SMH-TB), a retrospective 2 cohort of electronic health record data and variables extracted using natural language 3 processing 4 David Landsman1, Ahmed Abdelbasit2, Christine Wang2, Michael Guerzhoy3, 4, 5, Ujash Joshi4, 5 Shaun Mathew6, Chloe Pou-Prom7, David Dai7, Victoria Pequegnat8, Joshua Murray7, Kamalprit 6 Chokar9, Michaelia Banning7, Muhammad Mamdani5, 7, 10, 11, 12, Sharmistha Mishra¶, 1, 2, 11, Jane 7 Batt*,¶, 13, 14 8 1. MAP Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, St. Michael’s 9 Hospital, Unity Health Toronto, Toronto, Ontario, Canada 10 2. Department of Medicine, University of Toronto, Toronto, Ontario, Canada 11 3. Princeton University, Princeton, New Jersey, United States 12 4. University of Toronto, Toronto, Ontario, Canada 13 5. Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Unity Health Toronto, Toronto, 14 Ontario, Canada 15 6. Department of Computer Science, Ryerson University, Toronto, Ontario, Canada 16 7. Unity Health Toronto, Toronto, Ontario, Canada 17 8. Decision Support Services, St. Michael’s Hospital, Unity Health Toronto, Toronto, 18 Ontario, Canada 19 9. Division of Respirology, Department of Medicine, St. Michael’s Hospital, Unity Health 20 Toronto, Toronto, Ontario, Canada 21 10. -

January 1, 2019 to May 26, 2019
RECORD OF PROCEEDINGS January 1, 2019 – May 26, 2019 The United Church of Canada Shining Waters Regional Council 2019 - i Table of Contents EXECUTIVE, January 14, 2019 ...................................................................................................................... 1 COMMUNITIES OF FAITH COMMISSION, January 29, 2019.......................................................................... 7 PASTORAL RELATIONS COMMISSION, January 29, 2019 ........................................................................... 11 EXECUTIVE, February 6, 2019 .................................................................................................................... 19 PASTORAL RELATIONS COMMISSION, February 26, 2019 ......................................................................... 30 COMMUNITIES OF FAITH COMMISSION, February 28, 2019 ..................................................................... 36 EXECUTIVE, March 5, 2019 ........................................................................................................................ 42 PASTORAL RELATIONS COMMISSION, March 26, 2019 ............................................................................. 51 COMMUNITIES OF FAITH COMMISSION, March 28, 2019 ......................................................................... 56 EXECUTIVE, April 10, 2019 ......................................................................................................................... 62 EXECUTIVE, April 23, 2019 ........................................................................................................................ -

Leading the World When the World Needs Us Most
Leading the world when the world needs us most INFORMATION CIRCULAR 2021 We are leading the world TELUS is a dynamic, world-leading communications technology company with $16 billion in annual revenue and 16 million customer connections spanning wireless, data, IP, voice, television, entertainment, video and security. We leverage our global-leading technology and compassion to enable remarkable human outcomes. Our long-standing commitment to putting our customers first fuels every aspect of our business, making us a distinct leader in customer service excellence and loyalty. TELUS Health is Canada’s leader in digital health technology, TELUS Agriculture provides innovative digital solutions throughout the agriculture value chain and TELUS International is a leading digital customer experience innovator that delivers next-generation AI and content management solutions for global brands. Driven by our passionate social purpose to connect all citizens for good, our deeply meaningful and enduring philosophy to give where we live has inspired TELUS, our team members and retirees to contribute more than $820 million and 1.6 million days of service since 2000. This unprecedented generosity and unparalleled volunteerism have made TELUS the most giving company in the world. All financial information is reported in Canadian dollars unless otherwise specified. Copyright © 2021 TELUS Corporation. All rights reserved. Certain products and services named in this information circular are trademarks. The symbols TM and ® indicate those owned by TELUS Corporation or its subsidiaries. All other trademarks are the property of their respective owners. Welcome to our shareholder meeting The TELUS annual general meeting of shareholders will be held on May 7, 2021. -

February 25, 1999 Volume 39 ISSUE 25 "Simply the Best"
walk® (iflpl aix howtobeevil the Cord 3 23 mm u Thursday, February 25, 1999 Volume 39 ISSUE 25 "Simply the best" RECORD K-W THE COURTESY: BETH MULLEN As a result of effective passing by Heather Hossie at the end of the first was selected a first team all-star by a place over the course of the OUA finals Kim CIAU Shillington and Ashley Colter, period. This goal was matched a minute committee of OUA coaches. Teammates (and not earning a playoff spot), Through a flurry of helmets, gloves and Heather Allan sniped the next goal into and a half later by dangerous York com- Jen Krog and Kim Shillington were the Toronto \forsity Blues will play in the sticks about the awarded second as the result of strewn the ice surface on Guelph net at the begining of the petitor, Sari Krooks. team all-star honours. CIAU tournament a bye second contribu- to the hosts of the event. Sunday, February 14 at the University of period. Both teams played scoreless Along with these essentia! given after Backman The that exist in the Guelph's Gryphon Centre, you would Soon that play, came through the next two periods. tions to the team's high-flying offense challenges have been able future include to make your way to the through once again with an unassisted Confidently entering into overtime on a during the championships, aggressive Hawks near getting past Women's WLU lead added Kim celebrating 1999 Hockey OUA goal to round off the at 3-0. power-play, the WLU women were Hawk Cheryl Pounder, greatly to first-year McGill goalie, St.Pierre - WLU who to Champions The Wilfrid Laurier Golden Hardly decreasing the Hawks solid determined to score first. -

St. Michael's Hospital Integrated to Form a New Health Network Known As Unity Health Toronto
St. Michael’s Inspired Care. Inspiring Science. Trauma Director St. Michael’s Hospital University of Toronto Applications are invited for the position of Director of Trauma at St. Michael’s Hospital, part of Unity Health Toronto. Located in downtown Toronto, St. Michael’s Hospital is a designated provincial Level 1 Trauma Centre and provides care for patients in the Toronto and surrounding region.Trauma care is a key element of the hospital’s Strategic Plan. St. Michael’s Hospital is integrated with the Li Ka Shing Knowledge Institute, an institute dedicated to the advancement of research and education. On August 1, 2017, Providence Healthcare, St. Joseph's Health Centre and St. Michael's Hospital integrated to form a new health network known as Unity Health Toronto. United, the three organizations serve patients, residents and clients across the full spectrum of care while investing in world-class research and education. Unity Health Toronto works to advance the health of everyone in their urban communities and beyond. The health network provides services spanning primary care, secondary community care, tertiary and quaternary care services to post- acute through rehabilitation, palliative care and long-term care. St. Michael's Hospital is a fully affiliated University of Toronto teaching and research-intensive hospital, and is a hub for care, ranging from primary and secondary care to highly complex tertiary and quaternary care for patients from across the province. St. Michael's is downtown Toronto's adult trauma centre, as well as a major referral centre for severely injured patients from across the GTA and our provincial catchment area.