148343-ACI-Full-Book
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
01 Principal's Report 20 P&C
CAMMERAYGAL HIGH SCHOOL | PH: (02) 9954 7100 ISSUE #70 1 APRIL 2021 Cammeraygal High School Empowered to Achieve 01 PRINCIPAL’S REPORT 20 P&C MESSAGE FROM THE PRINCIPAL The delivery of our grand piano this week has CALENDAR been a wonderful way to end a very successful TERM 2 | WK 1 | 19 – 23 APRIL Term 1 here at Cammeraygal. Our first opportunity to showcase the grand piano for all students will be Monday Staff Development Day at our Anzac Day ceremony which will be our first Tuesday All students return for Term 2 on site whole school assembly since the start of Friday ANZAC Day Ceremony COVID, restrictions permitting, in Wk 1 of Tm 2. TERM 2 | WK 2 | 26 - 30 APRIL Student Safety in the Community Tuesday Cross Country We have been advised that there have been Wed - Fri Combined HS Swimming several cases in our region lately of students being approached by strangers while walking to and from UPCOMING EVENTS: school and in some cases of those strangers trying Careers Expo Incursion (Yrs 10/11 & 12) | 7 May to persuade students to get into vehicles. With the Y12 Parent Teacher | 11 May holidays upon us please continue to regularly Y11 Geography Excursion | 12 May speak with your children about the importance of Y8 Medieval Incursion | 13 May being aware of their surroundings (and not immersed in their phones!) while out and about Zone Athletics | 14 May and of seeking help from local businesses and Zone Cross Country | 20 May residents if they feel threatened. Y11 Parent Teacher | 27 May Cammeraygal Represented at the Regional Cross Country | 4 June Australian National Rowing Championships Queen’s Birthday Public Holiday | 14 June Lili H (Y12 )again demonstrated her outstanding Y7 Parent Teacher | 21 June rowing prowess at the Australian National Rowing Y10 Work Experience | 21 – 25 June Championships in Tasmanian this past weekend, Y8 & Y9 Parent Teacher | 24 June competing in the finals of the Schoolgirl Single Last Day Term 2 | 25 June th Scull for Cammeraygal and placing 5 overall. -
19 Language Revitalisation: Community and School Programs Working Together
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Sydney eScholarship 19 Language revitalisation: community and school programs working together Diane McNaboe1 and Susan Poetsch2 Abstract Since it was published in 2003 the New South Wales Aboriginal Languages K– 10 Syllabus has led to a substantial increase in the number of school programs operating in the state. It has supported the quality of those programs, and the status and recognition given to Aboriginal languages and cultures in the curriculum. School programs also complement community initiatives to revitalise, strengthen and share Aboriginal languages in New South Wales. As linguistic and cultural knowledge increases among adult community members, school programs provide a channel for them to continue to develop their own skills and knowledge and to pass on this heritage. This paper takes Wiradjuri as an example of language revitalisation, and describes achievements in adult language learning and the process of developing a school program with strong input from community. A brief history of Wiradjuri language revitalisation Wiradjuri is one of the central inland New South Wales (NSW) languages (Wafer & Lissarrague 2008, pp. 215–25). In recent decades various language teams have investigated and analysed archival sources for Wiradjuri and collected information from both written and oral sources (Büchli 2006, pp. 58–60). These teams include Grant and Rudder (2001a, b, c, d; 2005), Hosking and McNicol (1993), McNicol and Hosking (1994) and Donaldson (1984), as well as Christopher Kirkbright, George Fisher and Cheryl Riley, who have been working with Wiradjuri people in and near Sydney. -
Some Emerging Issues in Relation to Claims to Land Under the Aboriginal Land Rights Act 1983 (Nsw)
2011 Emerging Issues: Claims to Land under the Aboriginal Land Rights Act 1983 (NSW) 811 SOME EMERGING ISSUES IN RELATION TO CLAIMS TO LAND UNDER THE ABORIGINAL LAND RIGHTS ACT 1983 (NSW) JASON BEHRENDT ∗ I INTRODUCTION In 1983, the New South Wales Parliament passed the Aboriginal Land Rights Act 1983 (NSW) (‘ ALRA ’). The necessity to provide Aboriginal people with economic independence as well as providing compensation for past injustice was at the forefront of the policy underlying the enactment of the ALRA . In his second reading speech, the Minister for Aboriginal Affairs, Frank Walker noted that the Keane Report 1 prepared by the Parliamentary Select Committee that preceded the ALRA had noted that Aboriginal people experienced ‘severe economic deprivations’ and that the Committee believed that ‘land rights could also, in our times, lay the basis for improving Aboriginal self-sufficiency and economic wellbeing’. 2 He stated that ‘[i]n this sense land rights has a dual purpose – cultural and economic. Some lands, with traditional significance to Aborigines, will retain a cultural and a spiritual significance. Other lands will be developed as commercial ventures designed to improve living standards’. 3 The legislative policy expressed in the ALRA to return land to the Aboriginal people as ‘a form of economic compensation’ was noted by Sheller J in Minister Administering the Crown Lands Act v New South Wales Aboriginal Land Council .4 For the last 25 years, the ALRA has operated with mixed success. Although Frank Walker anticipated a quick process for the resolution of claims, the process of determining claims and transferring the land has taken much longer. -
MATHEWS J16 Sound Recordings Collected by Janet Mathews, 1972
Finding aid MATHEWS_J16 Sound recordings collected by Janet Mathews, 1972 Prepared November, 2006 by MH Last updated 12 December 2016 ACCESS Availability of copies Listening copies are available. Contact AIATSIS to arrange an appointment to listen to the recordings or to order copies. Restrictions on listening This collection is open for listening. Restrictions on use This collection is open for copying to the people recorded on the tapes, their relatives, Aboriginal communities in and around the places where the tapes were recorded, speakers of the languages recorded on the tapes, and Aboriginal cultural centres in and around the places where the tapes were recorded. All other clients may only copy this collection with the permission of Susan Upton. Permission must be sought from Susan Upton and the relevant Indigenous individual, family or community. Any publication or quotation must be consistent with the Copyright Act (1968). SCOPE AND CONTENT NOTE Date: 1972 Extent: 18 sound tape reels (ca. 1 hr. each) : analogue, 3 ¾ ips, mono + field tape report sheets Production history These recordings were collected by Janet Mathews between the 10th and 16th of April 1972 in Coonamble, Lightning Ridge, Weilmoringle and Brewarrina. They document various languages spoken in western New South Wales, including Wailwan, Yuwaalaraay, Guwamu and Muruwari, as spoken by Bill Davis, Fred Reece, Robin Campbell and Daisy Brown. The recordings also feature an oral history interview in English with Jimmie Barker. RELATED MATERIAL John Giacon has prepared partial transcripts of field tapes 104 - 112, copies of which are held by the AIATSIS Audiovisual Archive. For a complete listing of related material held by AIATSIS, consult the Institute's Mura® online catalogue at http://mura.aiatsis.gov.au. -
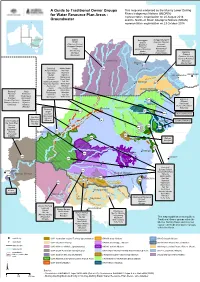
A Guide to Traditional Owner Groups For
A Guide to Traditional Owner Groups Th is m ap w as e nd orse d by th e Murray Low e r Darling Rive rs Ind ige nous Nations (MLDRIN) for Water Resource Plan Areas - re pre se ntative organisation on 20 August 2018 Groundwater and th e North e rn Basin Aboriginal Nations (NBAN) re pre se ntative organisation on 23 Octobe r 2018 Bidjara Barunggam Gunggari/Kungarri Budjiti Bidjara Guwamu (Kooma) Guwamu (Kooma) Bigambul Jarowair Gunggari/Kungarri Euahlayi Kambuwal Kunja Gomeroi/Kamilaroi Mandandanji Mandandanji Murrawarri Giabel Bigambul Mardigan Githabul Wakka Wakka Murrawarri Githabul Guwamu (Kooma) M Gomeroi/Kamilaroi a r a Kambuwal !(Charleville n o Ro!(ma Mandandanji a GW21 R i «¬ v Barkandji Mutthi Mutthi GW22 e ne R r i i «¬ am ver Barapa Barapa Nari Nari d on Bigambul Ngarabal C BRISBANE Budjiti Ngemba k r e Toowoomba )" e !( Euahlayi Ngiyampaa e v r er i ie Riv C oon Githabul Nyeri Nyeri R M e o r Gomeroi/Kamilaroi Tati Tati n o e i St George r !( v b GW19 i Guwamu (Kooma) Wadi Wadi a e P R «¬ Kambuwal Wailwan N o Wemba Wemba g Kunja e r r e !( Kwiambul Weki Weki r iv Goondiwindi a R Barkandji Kunja e GW18 Maljangapa Wiradjuri W n r on ¬ Bigambul e « Kwiambul l Maraura Yita Yita v a r i B ve Budjiti Maljangapa R i Murrawarri Yorta Yorta a R Euahlayi o n M Murrawarri g a a l rr GW15 c Bigambul Gomeroi/Kamilaroi Ngarabal u a int C N «¬!( yre Githabul R Guwamu (Kooma) Ngemba iv er Kambuwal Kambuwal Wailwan N MoreeG am w Gomeroi/Kamilaroi Wiradjuri o yd Barwon River i R ir R Kwiambul !(Bourke iv iv Barkandji e er GW13 C r GW14 Budjiti -

Indigenous Geographies of Home at Orient Point, NSW
University of Wollongong Research Online Faculty of Social Sciences - Honours Theses University of Wollongong Thesis Collections 2017 Indigenous Geographies of Home at Orient Point, NSW Hilton Penfold University of Wollongong Follow this and additional works at: https://ro.uow.edu.au/thss University of Wollongong Copyright Warning You may print or download ONE copy of this document for the purpose of your own research or study. The University does not authorise you to copy, communicate or otherwise make available electronically to any other person any copyright material contained on this site. You are reminded of the following: This work is copyright. Apart from any use permitted under the Copyright Act 1968, no part of this work may be reproduced by any process, nor may any other exclusive right be exercised, without the permission of the author. Copyright owners are entitled to take legal action against persons who infringe their copyright. A reproduction of material that is protected by copyright may be a copyright infringement. A court may impose penalties and award damages in relation to offences and infringements relating to copyright material. Higher penalties may apply, and higher damages may be awarded, for offences and infringements involving the conversion of material into digital or electronic form. Unless otherwise indicated, the views expressed in this thesis are those of the author and do not necessarily represent the views of the University of Wollongong. Recommended Citation Penfold, Hilton, Indigenous Geographies of Home at Orient Point, NSW, GEOG401: Human Geography (Honours), SGSC, University of Wollongong, 2017. https://ro.uow.edu.au/thss/14 Research Online is the open access institutional repository for the University of Wollongong. -

Aboriginal Languages
Aboriginal Languages Advice on Programming and Assessment for Stages 4 and 5 Acknowledgements The map on p 8 is © Department of Lands, Panorama Ave, Bathurst, NSW, www.lands.nsw.gov.au © 2003 Copyright Board of Studies NSW for and on behalf of the Crown in right of the State of New South Wales. This document contains Material prepared by the Board of Studies NSW for and on behalf of the State of New South Wales. The Material is protected by Crown copyright. All rights reserved. No part of the Material may be reproduced in Australia or in any other country by any process, electronic or otherwise, in any material form or transmitted to any other person or stored electronically in any form without the prior written permission of the Board of Studies NSW, except as permitted by the Copyright Act 1968. School students in NSW and teachers in schools in NSW may copy reasonable portions of the Material for the purposes of bona fide research or study. When you access the Material you agree: • to use the Material for information purposes only • to reproduce a single copy for personal bona fide study use only and not to reproduce any major extract or the entire Material without the prior permission of the Board of Studies NSW • to acknowledge that the Material is provided by the Board of Studies NSW • not to make any charge for providing the Material or any part of the Material to another person or in any way make commercial use of the Material without the prior written consent of the Board of Studies NSW and payment of the appropriate copyright fee • to include this copyright notice in any copy made • not to modify the Material or any part of the material without the express prior written permission of the Board of Studies NSW. -

A Thesis Submitted by Dale Wayne Kerwin for the Award of Doctor of Philosophy 2020
SOUTHWARD MOVEMENT OF WATER – THE WATER WAYS A thesis submitted by Dale Wayne Kerwin For the award of Doctor of Philosophy 2020 Abstract This thesis explores the acculturation of the Australian landscape by the First Nations people of Australia who named it, mapped it and used tangible and intangible material property in designing their laws and lore to manage the environment. This is taught through song, dance, stories, and paintings. Through the tangible and intangible knowledge there is acknowledgement of the First Nations people’s knowledge of the water flows and rivers from Carpentaria to Goolwa in South Australia as a cultural continuum and passed onto younger generations by Elders. This knowledge is remembered as storyways, songlines and trade routes along the waterways; these are mapped as a narrative through illustrations on scarred trees, the body, engravings on rocks, or earth geographical markers such as hills and physical features, and other natural features of flora and fauna in the First Nations cultural memory. The thesis also engages in a dialogical discourse about the paradigm of 'ecological arrogance' in Australian law for water and environmental management policies, whereby Aqua Nullius, Environmental Nullius and Economic Nullius is written into Australian laws. It further outlines how the anthropocentric value of nature as a resource and the accompanying humanistic technology provide what modern humans believe is the tool for managing ecosystems. In response, today there is a coming together of the First Nations people and the new Australians in a shared histories perspective, to highlight and ensure the protection of natural values to land and waterways which this thesis also explores. -

Fishing Malgun
Aboriginal Heritage Office Yarnuping Education Series Ku-ring-gai, Lane Cove, North Sydney, Northern Beaches, Strathfield and Willoughby Councils © Copyright Aboriginal Heritage Office www.aboriginalheritage.org Yarnuping 9 - Women and Salt Water Country – Fishing Karen Smith & Phil Hunt Sydney Aboriginal women are too often forgotten in the stories of Bennelong and other Sydney men of the late 1700s, early 1800s. I wanted to bring them to the fore in this Yarnuping about Saltwater Women. You will note that the commentators are largely men, which adds further imbalance to the story, so we must take things with a grain of salt. Malgun The Aboriginal custom of female finger- tip removal – 'malgun', “the finger is taken off by means of ligature (generally a sinew of a kangaroo) tied so tight as to stop the circulation of the blood, which induces mortification and the part drops off. I remember to have seen Colbee’s child, when about a month old, on whom this operation had just been performed by her mother.” Watkin Tench 1788 page 248 For example, Captain Arthur Phillip, of the First Fleet, interpreted finger tip removal as follows: “It was now first observed by the Governor that the women in general had lost two joints from the little finger of the left hand. As these appeared to be all married women, he at first conjectured this privation to be part of the marriage ceremony; but going afterwards into a hut where were several women and children, he saw a girl of five or six years of age whose left hand was thus mutilated; and at the same time an old woman, and another who appeared to have had children, on both of whom all the fingers were perfect. -

TAFE NSW Innovate Reconciliation Action Plan 2020 -2022
Innovate Reconciliation Action Plan 2020–2022 November 2020 – November 2022 tafensw.edu.au Acknowledgement of Country TAFE NSW acknowledges Aboriginal Peoples as the Traditional Custodians of the lands on which our campuses are located and where we conduct our business. We pay our respects to past, present, and emerging Elders, and we are committed to honouring Australian Aboriginal and Torres Strait Islander Peoples’ unique Cultural and spiritual relationships to the land, waters, and seas, as well as their rich contribution to society. We recognise that Aboriginal Cultures and Communities form the foundation of Cultural diversity within New South Wales. Hundreds of Cultures, Languages, and Kinship structures have long been embedded in the lands of Aboriginal Countries throughout the state. We acknowledge and celebrate these diverse Traditions, Customs, and Cultures that have existed for more than 60,000 years. TAFE NSW is committed to support Closing the Gap targets for Aboriginal and Torres Strait Islander Peoples, by identifying opportunities to increase their learning potential and by helping them to achieve their goals and flourish. TAFE NSW will continue to value Aboriginal and Torres Strait Islander Cultures and promote their rights and interests. In doing so, we acknowledge the wrongs of the past, respect the Cultural diversity of Aboriginal and Torres Strait Islander Peoples, and commit to embedding equality and equity throughout all areas of TAFE NSW by integrating inclusive and innovative opportunities that will result in stronger relationships built on respect and trust. Disclaimer: For the purposes of this document, use of the term ‘Aboriginal’ is inclusive of Torres Strait Islander Peoples and has been written and formated in accordance with the TAFE NSW Aboriginal and Torres Strait Islander Protocols for Appropriate Language and Referencing Guide. -

BOOKBINDING .;'Ft1'
• BALOS BOOKBINDING .;'fT1'. I '::1 1 I't ABORIGINAL SONGS FROM THE BUNDJALUNG AND GIDABAL AREAS OF SOUTH-EASTERN AUSTRALIA by MARGARET JANE GUMMOW A thesis submitted in fulfihnent ofthe requirements for the degree of Doctor of Philosophy Department ofMusic University of Sydney July 1992 (0661 - v£6T) MOWWnO UllOI U:lpH JO .uOW:lW :lip Ol p:ll1l:>W:l<J ACKNOWLEDGEMENTS Firstly, I wish to express my most sincere thanks to all Bundjalung and Gidabal people who have assisted this project Many have patiently listened to recordings ofold songs from the Austra1ian Institute ofAboriginal and Torres Strait Islander Studies, sung their own songs, translated, told stories from their past, referred me to other people, and so on. Their enthusiasm and sense ofurgency in the project has been a continual source of inspiration. There are many other people who have contributed to this thesis. My supervisor, Dr. Allan Marett, has been instrumental in the compilation of this work. I wish to thank him for his guidance and contributions. I am also indebted to Dr. Linda Barwick who acted as co-supervisor during part of the latter stage of my candidature. I wish to thank her for her advice on organising the material and assistance with some song texts. Dr. Ray Keogh meticulously proofread the entire penultimate draft. I wish to thank him for his suggestions and support. Research was funded by a Commonwealth Postgraduate Research Award. Field research was funded by the Austra1ian Institute of Aboriginal and Torres Strait Islander Studies. Several staff members at AlATSIS have been extremely helpful. -

Radiocarbon Dating of Archaeological Material at Present-Day Cammeray Indicates That Aboriginal People Were Living in the North
Radiocarbon dating of archaeological material at significant enough for Carradah to ‘exchange’ names of the city. Indigenous people were employed as and adopt the title Mr Ball for himself. He may well gardeners and grooms on the larger estates of North present-day Cammeray indicates that Aboriginal have assisted European exploration of north shore Sydney. people were living in the North Sydney area at areas. Balls Head was named in the Englishman’s The physical evidence of the first inhabitants of the least 5,800 years ago. By this time the last ice age honour. The Aboriginal name for the area was North Shore can be found in fire-charred caves, apparently not recorded. had ended and water levels had risen to create stencilled hands painted on stone, engravings of Sydney Harbour and its river valleys. The Barangaroo was also identified as a Cammeraygal animals and weapons on rocks, and middens of landforms and waterways familiar to these people woman in these early accounts. She was a wife of the whitened seashells from thousands of meals. Wongal man Bennelong and a strong willed figure would have differed little from those that Balls Head has some of the most significant who did not approve of her husband’s consorting with remaining Aboriginal sites in North Sydney. The European colonists first encountered in 1788. the interloping Europeans. Australian Museum investigated a rock shelter at Then, the North Shore of Sydney was inhabited by By the early 1800s Aboriginal social structures had Balls Head in 1964 and 1971 where the skeleton of the Cammeraygal (Gameraigal) clan or band.