The Impact of Anaesthesia Protocols on BOLD Fmri Validity in Laboratory Rodents –A Systematic Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lubeluzole/Mecamylamine Hydrochloride 1331 Precautions Ing Treated
Lubeluzole/Mecamylamine Hydrochloride 1331 Precautions ing treated. Mannitol infusion has also been used to de Manzanas; Pol.: Purisole SM; Port.: Purisole; Xarope de Macas Reinetas; Rus.: Rheogluman (Реоглюман); Spain: Salcemetic†; Salmagne; Switz.: Mannitol is contra-indicated in patients with pulmo- prevent acute renal failure during cardiovascular and Cital†. nary congestion or pulmonary oedema, intracranial other types of surgery, or after trauma. bleeding (except during craniotomy), heart failure (in To reduce raised intracranial or intra-ocular pres- patients with diminished cardiac reserve, expansion of sure mannitol may be given by intravenous infusion as Mebutamate (BAN, USAN, rINN) the extracellular fluid may lead to fulminating heart a 15 to 25% solution in a dose of 0.25 to 2 g/kg over 30 Mébutamate; Mebutamato; Mebutamatum; W-583. 2-sec-Butyl- failure), and in patients with renal failure unless a test to 60 minutes. Rebound increases in intracranial or 2-methyltrimethylene dicarbamate. dose has produced a diuretic response (if urine flow is intra-ocular pressure may occur but are less frequent Мебутамат inadequate, expansion of the extracellular fluid may than with urea. C10H20N2O4 = 232.3. lead to acute water intoxication). During transurethral prostatic resection a 2.5 to 5% CAS — 64-55-1. Mannitol should not be given with whole blood. ATC — N05BC04. solution of mannitol has been used for irrigating the ATC Vet — QN05BC04. All patients given mannitol should be carefully ob- bladder. served for signs of fluid and electrolyte imbalance and Ciguatera poisoning. Ciguatera poisoning occurs throughout O O renal function should be monitored. the Caribbean and Indopacific as a result of the consumption of certain fish contaminated with ciguatoxin; it is increasingly seen Pharmacokinetics in Europe, in travellers returning from these areas, or as a result H2NO O NH2 Only small amounts of mannitol are absorbed from the of eating imported fish. -

Ep 0665009 A1
Eu^^esP— || | MMMMI 1 1 1 1 1 1|||| 1 1 1||| || J European Patent Office _ _ _ _ _ © Publication number: 0 665 009 A1 Office europeen desj brevets © EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC © Application number: 93922625.4 © Int. CI.6: A61 K 9/00 @ Date of filing: 13.10.93 © International application number: PCT/JP93/01469 © International publication number: WO 94/08561 (28.04.94 94/10) ® Priority: 14.10.92 JP 303085/92 Koga-gun, Shiga 520-32 (JP) @ Date of publication of application: Inventor: IZUMI, Shougo 02.08.95 Bulletin 95/31 3-94, Nlshltsutsujlgaoka Mlyamadal 1-chome Kameoka-shl, © Designated Contracting States: Kyoto 621 (JP) AT BE CH DE DK ES FR GB GR IE IT LI LU MC Inventor: OKA, Masaakl NL PT SE 18-8-207, Hoshlgaoka 1-chome Hlrakata-shl, © Applicant: NIPPON SHINYAKU COMPANY, Osaka 573 (JP) LIMITED 14, Klssholn Nlshlnosho Monguchlcho Mlnaml-ku © Representative: Vogeser, Werner, Dipl.-lng. et Kyoto-shl al Kyoto 601 (JP) Patent- und Rechtsanwalte Hansmann, Vogeser, Dr. Boecker, © Inventor: NAKAMICHI, Koulchl Alber, Dr. Strych, Lledl 13-16, Kltayamadal 1-chome, Albert-Rosshaupter-Strasse 65 Koselcho D-81369 Munchen (DE) © CRYSTALLINE CONDITION DISLOCATING METHOD. © An object of this invention is to provide a meth- od of the crystalline condition of dislocating cry- \A/ < stalline medicine simply, speedily and homoge- 4 ^ 0 at neously, and, moreover, in large quantities at once. A X. X O O x.X o °o This invention is directed to a method using an x x.x O outlet side melting zonex cooling zone. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -
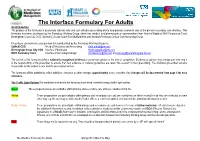
The Interface Formulary for Adults
The Interface Formulary For Adults An introduction The purpose of the formulary is to promote rational, safe and cost-effective prescribing and to help promote seamless care at the primary-secondary care interface. This formulary has been developed by the Formulary Working Group, which has medical and pharmaceutical representation from Heart of England NHS Foundation Trust, Birmingham Cross City CCG, Solihull CCG and South East Staffordshire and Seisdon Peninsula Clinical Commissioning Group. Prescribers can nominate a preparation for consideration by the Formulary Working Group via Solihull CCG Head of Medicines and Prescribing [email protected] Birmingham Cross City CCG Interface Pharmacist [email protected] HEFT Formulary Team Interface Prescribing Manager [email protected] or [email protected] The content of the formulary reflects nationally recognised evidence or consensus opinion at the time of compilation. Evidence or opinion may change over time and it is the responsibility of the prescriber to ensure that new evidence or national guidelines are taken into account in their prescribing. The individual prescriber remains responsible for the patient’s care and the prescription written. The formulary will be updated to reflect additions, removals or other changes approximately every 3 months. Any changes will be documented from page 3 for easy reference. The Traffic Light System The medicines included in the formulary have been classified using a traffic light system. Green These preparations are prescribable within primary and secondary care and are considered first line Yellow These preparations are prescribable within primary and secondary care and are considered as either second line or they are restricted in some other way e.g. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

WO 2014/115152 Al 31 July 20 14 (31.07.2014) W P O P CT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/115152 Al 31 July 20 14 (31.07.2014) W P O P CT (51) International Patent Classification: (72) Inventor; and A61K 51/04 (2006.01) (71) Applicant (for PG only): BEN-HAIM, Shlomo [IL/CH]; c/o Lemuria Alliance SA, 17 Rue des Pierres-du-Niton, (21) International Application Number: CH- 1207 Geneva (CH). PCT/IL20 14/050090 (74) Agents: G.E. EHRLICH (1995) LTD. et al: 11 Mena- (22) International Filing Date: chem Begin Road, 5268104 Ramat Gan (IL). 24 January 2014 (24.01 .2014) (81) Designated States (unless otherwise indicated, for every English (25) Filing Language: kind of national protection available): AE, AG, AL, AM, (26) Publication Language: English AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (30) Priority Data: DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, 61/756,1 12 24 January 2013 (24.01. 2013) US HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 61/776,599 11 March 2013 ( 11.03 2013) US KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 61/803,61 1 20 March 2013 (20.03 2013) us MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 61/83 1,664 6 June 2013 (06.06 2013) us OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, 61/875,069 ! September 2013 (08.09. -

Drug/Substance Trade Name(S)
A B C D E F G H I J K 1 Drug/Substance Trade Name(s) Drug Class Existing Penalty Class Special Notation T1:Doping/Endangerment Level T2: Mismanagement Level Comments Methylenedioxypyrovalerone is a stimulant of the cathinone class which acts as a 3,4-methylenedioxypyprovaleroneMDPV, “bath salts” norepinephrine-dopamine reuptake inhibitor. It was first developed in the 1960s by a team at 1 A Yes A A 2 Boehringer Ingelheim. No 3 Alfentanil Alfenta Narcotic used to control pain and keep patients asleep during surgery. 1 A Yes A No A Aminoxafen, Aminorex is a weight loss stimulant drug. It was withdrawn from the market after it was found Aminorex Aminoxaphen, Apiquel, to cause pulmonary hypertension. 1 A Yes A A 4 McN-742, Menocil No Amphetamine is a potent central nervous system stimulant that is used in the treatment of Amphetamine Speed, Upper 1 A Yes A A 5 attention deficit hyperactivity disorder, narcolepsy, and obesity. No Anileridine is a synthetic analgesic drug and is a member of the piperidine class of analgesic Anileridine Leritine 1 A Yes A A 6 agents developed by Merck & Co. in the 1950s. No Dopamine promoter used to treat loss of muscle movement control caused by Parkinson's Apomorphine Apokyn, Ixense 1 A Yes A A 7 disease. No Recreational drug with euphoriant and stimulant properties. The effects produced by BZP are comparable to those produced by amphetamine. It is often claimed that BZP was originally Benzylpiperazine BZP 1 A Yes A A synthesized as a potential antihelminthic (anti-parasitic) agent for use in farm animals. -

Council of Europe Committee of Ministers (Partial
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (82) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 2 June 1982 at the 348th meeting of the Ministers' Deputies and superseding Resolution AP (77) 1) AND APPENDIX containing the list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 31 October 1982 RESOLUTION AP (82) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION 1 (Adopted by the Committee of Ministers on 2 June 1982 at the 348th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands, the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969 and 5 May 1964, respectively, Considering that, under the terms of its Statute, the aim of the Council of Europe is to achieve a greater unity between its Members for the purpose of safeguarding and realising the ideals and principles which are their common heritage and facilitating their economic and social progress; Having regard to the -

Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes
Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2004) -- Supplement 1 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABACAVIR 136470-78-5 ACEXAMIC ACID 57-08-9 ABAFUNGIN 129639-79-8 ACICLOVIR 59277-89-3 ABAMECTIN 65195-55-3 ACIFRAN 72420-38-3 ABANOQUIL 90402-40-7 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABIRATERONE 154229-19-3 ACIVICIN 42228-92-2 ABITESARTAN 137882-98-5 ACLANTATE 39633-62-0 ABLUKAST 96566-25-5 ACLARUBICIN 57576-44-0 ABUNIDAZOLE 91017-58-2 ACLATONIUM NAPADISILATE 55077-30-0 ACADESINE 2627-69-2 ACODAZOLE 79152-85-5 ACAMPROSATE 77337-76-9 ACONIAZIDE 13410-86-1 ACAPRAZINE 55485-20-6 ACOXATRINE 748-44-7 ACARBOSE 56180-94-0 ACREOZAST 123548-56-1 ACEBROCHOL 514-50-1 ACRIDOREX 47487-22-9 ACEBURIC ACID 26976-72-7 -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -

HALOSIN Indications Therapeutic Class Pharmacology Dosage
the lungs. The remaining 20% is lower concentration is usually HALOSIN metabolized in the liver by oxidative and most suitable for elderly under hypoxic conditions, reductive patients. Indications pathways. The main metabolites are Halothane is a volatile anaesthetic which trifluoroacetic acid, bromide and Interaction is suitable for the induction and chloride salts (via the oxidative Increased risk of ventricular maintenance of anaesthesia for all types pathway) and fluoride salts (via the dysrhythmias with epinephrine. of surgery and in patients of all ages. reductive pathway). The concentrations Increased risk of malignant of metabolites peak 24 hours post- hyperthermia with suxamethonium. Therapeutic Class operatively and are eliminated by renal Prolonged recovery from anaesth with General (Inhalation) anesthetics excretion during the following week. concurrent use of ketamine for induction. May potentiate response to Pharmacology Dosage & Administration non-depolarising muscle relaxants, When inhaled, Halothane is absorbed A number of anaesthetic vaporisers hypotensive agents (e.g. hexamethonium through the alveoli into the bloodstream. specially designed for use with bromide, trimetaphan camsilate). In the bloodstream, Halothane circulates Halothane are available. Open, semi- through the body to the principal site of open, semi-closed and closed circuit Contraindications action, the brain. Here Halothane causes systems have all been used with good Halothane can induce liver damage; a progressive depression of the central results. however, the incidence of severe liver nervous system, beginning with the damage (jaundice, which may lead to higher centers (cerebral cortex) and For induction of anaesthesia: hepatic failure as a consequence of spreading to the vital centers in the massive hepatic cell necrosis) is medulla. -

Essential Medicines in the United States Andrew Ellner
Essential Medicines in the United States Andrew Ellner, Luisa Dillner, Beth Nash, Fiona Godlee BMJ Publishing Group April 25, 2003 Contents Contents 2 Executive summary 3 Introduction 8 Methods 9 Defining essential drugs 11 Developing an essential medicines list 14 Implementing an essential medicines list 20 Accounting for the interests of important stakeholders 26 Access to essential medicines for seniors in other developed countries 30 Access to essential medicines for seniors in the United States 33 Comparative analysis of drug lists 36 Recommendations 37 Acknowledgements 38 References 39 Appendix A: Comparative matrix of cardiovascular drugs 58 Appendix B: Methodology used for drug list comparison 66 Essential Medicines in the United States 2 Executive summary Introduction This report has been produced at the request of UnitedHealth Foundation. UHF has been interested for some time in the concept of an essential medicines list that could improve access to health care for the uninsured population. This report focuses on the potential for developing an essential medicines list for seniors in the United States. Methods • An in-depth policy review was carried out on essential medicines and related concepts, such as drug formularies. • We consulted with experts in the fields of pharmacoeconomics, pharmacology, evidence-based medicine, health care policy, geriatrics and biostatistics. • To see if there is an international consensus on a basic drug benefits package, we did a comparative analysis of drug lists from English-speaking developed