Summa Health System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treacher Collins Prize Essay the Significance of Nystagmus
Eye (1989) 3, 816--832 Treacher Collins Prize Essay The Significance of Nystagmus NICHOLAS EVANS Norwich Introduction combined. The range of forms it takes, and Ophthalmology found the term v!to"[<xy!too, the circumstances in which it occurs, must be like many others, in classical Greece, where it compared and contrasted in order to under described the head-nodding of the wined and stand the relationships between nystagmus of somnolent. It first acquired a neuro-ophthal different aetiologies. An approach which is mological sense in 1822, when it was used by synthetic as well as analytic identifies those Goodl to describe 'habitual squinting'. Since features which are common to different types then its meaning has been refined, and much and those that are distinctive, and helps has been learned about the circumstances in describe the relationship between eye move which the eye oscillates, the components of ment and vision in nystagmus. nystagmus, and its neurophysiological, Nystagmus is not properly a disorder of eye neuroanatomic and neuropathological corre movement, but one of steady fixation, in lates. It occurs physiologically and pathologi which the relationship between eye and field cally, alone or in conjunction with visual or is unstable. The essential significance of all central nervous system pathology. It takes a types of nystagmus is the disturbance in this variety of different forms, the eyes moving relationship between the sensory and motor about one or more axis, and may be conjugate ends of the visual-oculomotor axis. Optimal or dysjugate. It can be modified to a variable visual performance requires stability of the degree by external (visual, gravitational and image on the retina, and vision is inevitably rotational) and internal (level of awareness affected by nystagmus. -

Pediatric Ophthalmology/Strabismus 2017-2019
Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017–2019 Pediatric Ophthalmology/Strabismus *** Pediatric Ophthalmology/Strabismus 2 © AAO 2017-2019 Practicing Ophthalmologists Curriculum Disclaimer and Limitation of Liability As a service to its members and American Board of Ophthalmology (ABO) diplomates, the American Academy of Ophthalmology has developed the Practicing Ophthalmologists Curriculum (POC) as a tool for members to prepare for the Maintenance of Certification (MOC) -related examinations. The Academy provides this material for educational purposes only. The POC should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. The physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all the circumstances presented by that patient. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any information contained herein. References to certain drugs, instruments, and other products in the POC are made for illustrative purposes only and are not intended to constitute an endorsement of such. Such material may include information on applications that are not considered community standard, that reflect indications not included in approved FDA labeling, or that are approved for use only in restricted research settings. The FDA has stated that it is the responsibility of the physician to determine the FDA status of each drug or device he or she wishes to use, and to use them with appropriate patient consent in compliance with applicable law. -

Assessment and Management of Infantile Nystagmus Syndrome
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a o l m l a o n l r o Atilla, J Clin Exp Ophthalmol 2016, 7:2 g u y o J Ophthalmology 10.4172/2155-9570.1000550 ISSN: 2155-9570 DOI: Review Article Open Access Assessment and Management of Infantile Nystagmus Syndrome Huban Atilla* Department of Ophthalmology, Faculty of Medicine, Ankara University, Turkey *Corresponding author: Huban Atilla, Department of Ophthalmology, Faculty of Medicine, Ankara University, Turkey, Tel: +90 312 4462345; E-mail: [email protected] Received date: March 08, 2016; Accepted date: April 26, 2016; Published date: April 29, 2016 Copyright: © 2016 Atilla H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract This article is a review of infantile nystagmus syndrome, presenting with an overview of the physiological nystagmus and the etiology, symptoms, clinical evaluation and treatment options. Keywords: Nystagmus syndrome; Physiologic nystagmus phases; active following of the stimulus results in poor correspondence between eye position and stimulus position. At higher velocity targets Introduction (greater than 100 deg/sec) optokinetic nystagmus can no longer be evoked. Unlike simple foveal smooth pursuit, OKN appears to have Nystagmus is a rhythmic, involuntary oscillation of one or both both foveal and peripheral retinal components [3]. Slow phase of the eyes. There are various classifications of nystagmus according to the nystagmus is for following the target and the fast phase is for re- age of onset, etiology, waveform and other characteristics. -

6269 Variation of the Response to the Optokinetic Drum Among Various Strain
[Frontiers in Bioscience 13, 6269-6275, May 1, 2008] Variation of the response to the optokinetic drum among various strains of mice Oliver Puk1, Claudia Dalke1, Martin Hrabé de Angelis2, Jochen Graw1 1 GSF-National Research Center for Environment and Health, Institute of Developmental Genetics, D-85764 Neuherberg, Germany, 2GSF-National Research Center for Environment and Health, Institute of Experimental Genetics, D-85764 Neuherberg, Germany TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Materials and methods 3.1. Animals 3.2. Vision test protocol 3.3. Statistical analysis 3.4. Funduscopy 3.5. Electroretinography 3.6. Histology 4. Results 4.1. Head-tracking behavior 4.2. Electroretinography, funduscopy and histology of DBA/2 and BALB/c mice 4.3. Linkage analysis of BALB/c 5. Discussion 6. Acknowledgement 7. References 1. ABSTRACT 2. INTRODUCTION The mouse is currently an established The optokinetic drum has become an appropriate mammalian model for studying hereditary disorders, which tool to examine visual properties of mice. We performed have an effect on eye structure and function. In order to baseline measurements using mice of the inbred strains select and characterize mouse mutants suffering from C3H, C57BL/6, BALB/c, JF1, 129 and DBA/2 at the age of ocular defects, a variety of test systems are well 8-15 weeks. Each individual C57BL/6, 129 and JF1 mouse established, like slit lamp analysis for detecting lens was reliably identified as non-affected in vision by opacities, iris and corneal abnormalities (1-3), funduscopy determining head-tracking responses. C3H mice were used for abnormalities of the retinal fundus, reflecting retinal as negative control because of their inherited retinal degeneration, vascular problems and optic disc alterations degeneration; as expected, they did not respond to the (4), or electroretinography for functional disorders of the moving stripe pattern. -

Prolonged Pursuit by Optokinetic Drum Testing in Asymptomatic Female Carriers of Novel FRMD7 Splice Mutation C.1050 ؉5GϾA
OPHTHALMIC MOLECULAR GENETICS SECTION EDITOR: JANEY L. WIGGS, MD, PhD Prolonged Pursuit by Optokinetic Drum Testing in Asymptomatic Female Carriers of Novel FRMD7 Splice Mutation c.1050 ؉5GϾA Arif O. Khan, MD; Jameela Shinwari, MSc; Latifa Al-Sharif, BSc; Dania S. Khalil, BSc; Nada Al Tassan, PhD Objective: To determine the genotype underlying sus- was identified in the 2 affected brothers and in the 3 asymp- pected X-linked infantile nystagmus in a family and to tomatic women only. Allele sharing analysis further con- correlate genotype with clinical examination in poten- firmed that the aunt’s phenotype was not related to the tial female carriers. FRMD7 variant, which was absent in 246 ethnic controls. Her phenotype was also not related to mutation in known Methods: Ophthalmic examination (ophthalmic, or- CFEOM genes (KIF21A, PHOX2A, TUBB3). thoptic, optokinetic [OKN] drum, and electrophysi- ologic when possible) and candidate gene analysis. Conclusions: Prolonged pursuit responses during OKN drum testing in asymptomatic female carriers is consis- Results: Two affected brothers had infantile nystagmus tent with the concept of infantile nystagmus being an ab- with no evidence of associated visual or neurological normally increased pursuit oscillation. Further studies disease. The symptomatic maternal aunt had infantile are required to determine the reproducibility of this po- nystagmus in addition to congenital fibrosis of the ex- tential female carrier sign. Rather than being FRMD7 re- traocular muscles (CFEOM) (bilateral hypotropia, exo- lated, nystagmus in the maternal aunt represented a sec- tropia, ptosis, almost complete ophthalmoplegia, and ond disease in this family, likely related to CFEOM. poorly reactive pupils). A sister, the mother, and the ma- ternal grandmother—all 3 of whom were asymptomatic— Clinical Relevance: Clinicians can use the OKN drum had delayed corrective saccades (prolonged pursuit) dur- to assess obligate female carriers in a family suspected ing OKN drum testing. -

Ocular Emergencies – Chemical Burns (Alkali) – Temporal Arteritis Victoria M
Acute Conditions Emergency – Retinal Artery Occlusion Ocular Emergencies – Chemical burns (alkali) – Temporal Arteritis Victoria M. Romaniuk, MD – Orbital compartment syndrome Clinical Instructor of Emergency Medicine University of Maryland School of Medicine Very Urgent – Perforation – Rupture – Acute glaucoma Acute Conditions Non Traumatic Red Eye Possible Causes Urgent – Orbital cellulitis Conjunctivitis – Orbital injury Corneal – Corneal ulcer Inflammation/Infection – Corneal abrasion Iritis (Uveitis) – Hyphema Acute glaucoma – Intraocular foreign body – Retinal detachment – Macular edema Non Traumatic Red Eye Anatomy Conjunctivitis Discharge type Etiology Purulent Bacterial Serous or clear Viral Stringy, white Allergic Pre-auricular lymph node enlargement: Viral 1 Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Bacterial Conjunctivitis – Mucopurulent d/c – Staph, strep – Visual acuity good – Treatment: Antibiotic ointment or drops (Erythromycin, fluoroquinolone) Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Gonococcal Conjunctivitis Gonococcal – Copious discharge – Pre-auricular adenopathy – Neonates: Bilateral, 3-5 days post vaginal delivery – Treatment: IV Penicillin – Can cause perforation Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Viral Conjunctivitis Chlamydia (Inclusion) – Adenovirus – Lymphoid follicles – Frequently bilateral – Neonates: 5-14 days post vaginal delivery – Associated with URI – Adults: recurring symptoms, – Treatment: supportive ocular -

Ophthalmic Study Guide
67859 study guide cover:Layout 1 21/10/2009 11:18 Page 1 The Ophthalmic Study Guide Study Ophthalmic The In recent years, an increasing variety of professionals have been involved in the care of ophthalmic patients. This study guide, written by a team of specialist ophthalmic practitioners, enables nurses, healthcare assistants and other health professionals to The develop useful, basic ophthalmic knowledge quickly, whether they need it for their day-to-day work or as preparation for taking a higher qualification in ophthalmology. The Ophthalmic Study Guide has a number of helpful features, including red and amber flags to indicate urgent and less urgent symptoms, plentiful diagrams, lists of useful online resources, and simple questions at the end of many of the chapters, which Ophthalmic can be used for self-testing or as a basis for mentors’ questions to their students. There are also ‘To do’ boxes, which allow students to reflect on their own practice and develop good habits of self-assessment and self-directed learning. Study Guide Contents include G Basic anatomy and physiology of the eye G Basic pharmacology Other titles include G Treatment of cataracts G Treatment of glaucomas G Retinal problems G Macular degeneration G Ophthalmic equipment for Nurses and G Basic ophthalmic procedures Health Professionals Ophthalmology Books available from M&K Research Issues in Health Routine Blood Results The ECG Workbook and Social Care Explained 2/e ISBN: 978-1-905539-14-7 • 2008 ISBN: 978-1-905539-20-8 • 2009 ISBN: 978-1-905539-38-3 • 2007 -
9Ophthalmology Classification.Pdf
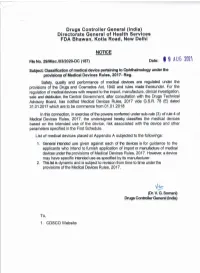
Appendix A File No. 29/Misc/03/2020-DC(187) Drugs Controller General (India) Directorate General of Health Services FDA Bhawan, Kotla Road, New Delhi. Notice Classification of Medical Devices Pertaining to Ophthalmology S. Risk Device Name Intended Use No. Class An ophthalmic device intended to measure the time required for retinal 1 Adaptometer B adaptation and the minimum light threshold. An ophthalmic device intended to 2 Amsler grid rapidly detect central and paracentral A irregularities in the visual field. A ophthalmic instrument used to test a patient for abnormal red/green colour 3 Anomaloscope A vision by differentiating the red/green colour vision defects. A collection of sterile devices, Aqueous/vitreous humour including a fluid or semifluid 4 D replacement medium kit substance, used in combination to replace the fluid of the eye. An ophthalmic instrument designed to measure the focusing power (dioptric Automated 5 power) and other optical A lensmeter(Dioptometer) characteristics of a spectacle lens, contact lens, or prism. An ophthalmic plane lens, intended to 6 Bagolini lens determine harmonious/anomalous A retinal correspondence. An ophthalmic device for binocular 7 Binocular vision test unit A vision testing. A hand-held, manual, ophthalmic surgical instrument intended to be 8 Blepharoplasty scissors used to cut eyelid tissue during plastic A surgery of the eyelids (blepharoplasty). A device intended to be permanently implanted in the posterior chamber of the eye for correction and fixation of a 9 Capsular bag anchor C subluxated capsular bag, typically in association with in-the-bag intraocular lens (IOL) implantation. Page 1 of 13 An ophthalmic lamp, used to test a 10 Colour discrimination tester person's ability to differentiate A between colours. -

Objective Evaluation of Patients with Vestibular Disorders
Global Journal of Otolaryngology ISSN 2474-7556 Research Article Glob J Otolaryngol - Volume 7 Issue 4 April 2017 Copyright © All rights are reserved by Lalsa Shilpa Perepa DOI: 10.19080/GJO.2017.07.555716 Objective Evaluation of Patients with Vestibular Disorders Lalsa Shilpa Perepa* Clinical Audiologist, Hearing First, Canada Submission: April 22, 2017; Published: May 05, 2017 *Corresponding author: Lalsa Shilpa Perepa, Clinical Audiologist, Hearing First, 1995 Weston Road Unit B, Toronto - M9N 1X2, Canada, Email: Introduction B. Speed of the eye movement equals that of the head Vestibular function tests are perceived as being less movement clinically useful than functional tests of the auditory system and, as a result, underestimate their full potential. Several factors C. Allows objects to remain in focus during head contribute to this perception. The anatomy and physiology of the movements peripheral and central vestibular system are at least as complex Compensatory Eye Movements as those of the auditory system, but audiologists in general possess less knowledge and interest in the vestibular system. combine to stabilize object on the same area of the retina=visual VOR, Optokinetic reflex, Smooth pursuit reflex, Neck reflexes peripheral vestibular problems from those of CNS origin, stability. The VOR is mediated by a three-neuron arc. For many years, audiologists considered it sufficient to separate treating peripheral lesions and referring non peripheral lesions For the horizontal VOR, these neurons include: A. the eighth cranial nerve (neuron 1), of the visual and somatosensory systems also is necessary to neurologists. This no longer is sufficient; today knowledge to complement that of the vestibular system if assessment of B. -

Doctor, Why Can't I See? Evaluation of the Patient Uncorrectable to 20/20
8/26/2019 Speakers Bureau for Aeri, Allergan, Bausch & Lomb, Glaukos, Ivantis, Optovue, Reichert Robert P. Wooldridge, O.D., F.A.A.O. Always be able to account for a patient’s VA Always be able to account for a patient’s VF Always be able to account for a patient’s C/O LOV ◦ vague complaint Anatomical Approach Refractive How to Evaluate Media opacity/distortion Refraction Macula problem ◦ Retinoscopy-lost skill look for scissors/distorted reflex Optic nerve/Neurologic Pinhole VA Amblyopia High order aberrations Hysteria/malingering 1 8/26/2019 Tear film Grade the View! Cornea VA vs View ◦ PEK, Central Cloudy Dystrophy of Francois (CCDF) Anterior Chamber 20/80 ◦ Careful evaluation for C/F hem, etc Lens ◦ Milky white NS vs yellow brown NS; vacuoles Vitreous 20/20 ◦ Hemorrhage ◦ Clarity: variable, cloudy ◦ Punctate Keratopathy Slit Lamp exam PEK, SPK Tear BUT ◦ Opacity: Oculus Topographer Scar Epithelial edema Stromal edema Central Cloudy Dystrophy of Francois (CCDF) Slit Lamp exam Keratoconus Corneal topography Pellucid Marginal Retinoscopy Degeneration (PMD) Pachymetry Post LASIK/PRK ◦ Ultrasonic Post PKP ◦ OCT CL induced 2 8/26/2019 Unusual cause of Nuclear sclerosis (NS) unclear media ◦ Milky white vs. Careful slit lamp brunescent yellow/brown NS exam ◦ Vacuoles ◦ Cells/flare Cortical cataract ◦ RBC’s ◦ Anterior (ACC) Turn the SL light ◦ Posterior (PCC) up high! Posterior Subcapsular (PSC) Easier to see with dilated pupil Myopic shift is a good hint of cataract progression! Slit Lamp exam -

21 CFR Ch. I (4–1–12 Edition) § 886.1200
§ 886.1200 21 CFR Ch. I (4–1–12 Edition) (b) Classification. Class I (general con- perforated mirror device intended to trols). The device is exempt from the inspect the interior of the eye) that premarket notification procedures in projects a bright light encompassing an subpart E of part 807 of this chapter, arc of about 30 degrees onto the fundus subject to the limitations in § 886.9. The of the eye. The center of the light bun- device is also exempt from the current dle is blocked by a black disk covering good manufacturing practice require- the fovea (the central depression of the ments of the quality system regulation macular retinae where only cones are in part 820 of this chapter, with the ex- present and blood vessels are lacking). ception of § 820.180, with respect to gen- The device is intended for use in the eral requirements concerning records, treatment of amblyopia (dimness of vi- and § 820.198, with respect to complaint sion without apparent disease of the files. eye). [52 FR 33355, Sept. 2, 1987, as amended at 53 (b) Classification. Class I for the bat- FR 35603, Sept. 14, 1988; 66 FR 38810, July 25, tery powered device. The battery pow- 2001] ered device is exempt from the pre- market notification procedures in sub- § 886.1200 Optokinetic drum. part E of part 807 of this chapter, sub- (a) Identification. An optokinetic ject to the limitations in § 886.9. Class drum is a drum-like device covered II for the AC-powered device. with alternating white and dark stripes or pictures that can be rotated on its [55 FR 48441, Nov. -

Understanding the Mechanisms of Motor Learning in the Vestibulo-Ocular Reflex
Understanding the Mechanisms of Motor Learning in the Vestibulo-ocular Reflex by Heather Kathryn Titley A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Department of Physiology University of Toronto © Copyright by Heather Titley 2011 Understanding the Mechanisms of Motor Learning in the Vestibulo-ocular Reflex Heather Kathryn Titley Doctor of Philosophy Department of Physiology University of Toronto 2011 Abstract The vestibulo-ocular reflex (VOR) is a simple reflex that stabilizes gaze by moving the eyes in the opposite direction to the head. The gain of the VOR (ratio of head to eye velocity) can be increased or decreased during motor learning. It is thought that the memory for learned changes in the VOR gain is initially encoded within the cerebellar flocculus. Furthermore, these learned gain changes can be disrupted or consolidated into a long-term memory. In this thesis we describe novel results that show that consolidation of the VOR can take place rapidly, within 1 hour after learning has stopped. Furthermore, we demonstrated that unlike learning, which has been shown to have frequency selectivity, disruption and rapid consolidation generalize across the range of frequencies. We suggest that disruption and rapid consolidation in the VOR are local mechanisms within the cerebellar cortex, and do not require new learning. This thesis also provides additional evidence for the idea that learned gain increases and decreases are the result of separate mechanisms, most likely long-term depression and potentiation respectively, at the parallel fibre-Purkinje cell synapses. We demonstrate that learned gain increases, but not decreases, require the activation of type 1 metabotropic glutamate receptors (mGluR1) and B type γ-aminobutyric acid (GABAB) receptors.