BOARD of DIRECTORS PUBLIC MEETING MINUTES October 16
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
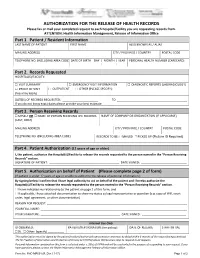
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

BCNU - EDMP Contact List
BCNU - EDMP Contact List Representative Region Sites Vancouver Coastal (VCHA) Dawn Tonge Coastal Mountain/ Richmond: Acute, Community & [email protected] RIVA Long-Term Care (Minoru, Lions Cell: 604 862 1063 Manor), Lions Gate Hospital, Sunshine Coast-Sechelt, Powell River, Whistler, Pemberton/ Squamish, Bella Bella, Bella Coola Silvia Kuntze Central Vancouver/ Vancouver Acute, UBC, TCU– [email protected] RIVA Koerner Pavilion, Mary Pack, Cell: 604 862 0186 Broadway Corporate Offices, CST, Tertiary Mental Health (Willow/Segal), Banfield Jaspreet Gill Central Vancouver/ Community Care, George [email protected] RIVA Pearson Centre, G.F. Strong Cell: 604 312 0826 Vancouver Island (VIHA) Elaine Greer South Islands Victoria (except RJH & Mental [email protected] Health), SPH, Lady Minto, PHS Cell: 250 889 0228 Holly Anderson Pacific Rim NRGH, Oceanside, Port Alberni [email protected] (except Westhaven), Tofino/ Cell: 250 713 8772 Ucleulet, Comox/Courtenay, Campbell River, Mt. Waddington Laura Rachwalski Pacific Rim/ RJH, Victoria Mental Health (all [email protected] South Islands sites & programs), Duncan, Cell: 250 893 1774 Chemainus, Ladysmith, Nanaimo (except NRGH), Trillium, Westhaven, Eagle Park Fraser Health (FHA) Nicole Ng Fraser Valley/ Ridge Meadows Hospital, ARH, [email protected] South Fraser Valley/ Abbotsford Community, Langley Cell: 604 785 7644 Simon Fraser Memorial Hospital, Langley Community, Cottage/Worthington October 2020 Representative Region Sites Cathy Ellen Queen South Fraser Valley Delta Hospital -

Trauma Services BC a Service of the Provincial Health Services Authority Contents
2015 ANNUAL REPORT Trauma Services BC A service of the Provincial Health Services Authority Contents 3 Foreword 4 Overview 5 BC’s system of organized trauma care 6 Trauma Services BC 7 Vision for BC’s trauma system 8 Governance 9 Trauma Services BC council 10 Strategic plan (2014-2016) 11 Partnerships & collaborations 12 BC Trauma Registry 13 Overview 14 Registry data quality monitoring 15 BC Trauma Registry operations 16 Key achievements 17 Future plans 18 Mechanism of Injury – Provincial overview 19 Regional health authority and partners trauma program report 20 Fraser Health 22 Interior Health 24 Island Health 26 Northern Health 28 Vancouver Coastal Health 30 BC Children’s Hospital 32 Special initiatives 33 Specialist Services Committee Project 34 Performance monitoring & evaluation plan 36 Accreditation Canada Trauma Distinction program 38 Looking forward 40 References and photo credits 42 Appendices 43 Appendix 1 – Inclusion/exclusion criteria for the BC Trauma Registry 44 Appendix 2 – Data quality 46 Appendix 3 – BC trauma program membership Foreword The 2015 annual report describes events and activities Our editor “in-situ” Mr. Beide Bekele, Trauma Services that took place within the calendar year supported by BC’s project manager, who discretely pushed us data from 2013/14. 2015 has been an exciting year of on timelines, content and continuity while working acquisition and building infrastructure for Trauma Services with our graphic artist, Mr. Ernest Stelzer, and PHSA BC with a strategic focus on advancing: communications, all of whom contributed to the look • Optimal service delivery for BC residents reflected in and tone of the report. -

Breast Biopsy Limit Any Arm Strain on the Side You Had Jim Pattison Outpatient Care 604-533-3308 the Biopsy
Care at home Locations Abbotsford-Regional Hospital 604-851-4868 Your breast will be tender and a little Medical Imaging 2nd Floor, Fraser Wing, 32900 Marshall Road, Abbotsford swollen. You might get a bruise at the BC Cancer Agency 604-877-6000 needle site. This is normal and should go Medical Imaging, 3rd Floor, 600 West 10th Ave, Vancouver Chilliwack General Hospital 604-795-4122 away within a few days. Medical Imaging, Main Floor, 45600 Menholm Rd, Chilliwack Return to your regular daily activities. Delta Hospital 604-946-1121 Medical Imaging, 5800 Mountain View Boulevard, Delta Breast Biopsy Limit any arm strain on the side you had Jim Pattison Outpatient Care 604-533-3308 the biopsy. and Surgery Centre ext. 63926 Medical Imaging, 2nd Floor, 9750 140th Street, Surrey Langley Memorial Hospital 604-533-6405 For the next 24 hours: Medical Imaging, Main Floor, 22051 Fraser Highway, Langley Wear a supportive bra. Lions Gate Hospital 604-984-5775 Place an ice pack over your bra on the Medical Imaging, Lower Level, 231 East 15th Street, North Vancouver needle site for 10 to 15 minutes at a Mount Saint Joseph Hospital 604-877-8323 Medical Imaging, Level one, 3080 Prince Edward Street, Vancouver time. Peace Arch Hospital 604-531-5512 If needed, take plain acetaminophen Medical Imaging, Main Floor, 15521 Russell Ave, White Rock (Tylenol) for pain. Powell River General Hospital 604-485-3282 Medical Imaging, 5000 Joyce Avenue, Powell River Richmond Hospital 604-278-9711 Medical Imaging, Main Floor, 7000 Westminster Hwy, Richmond When to get help Ridge Meadows Hospital 604-463-1800 Call your doctor if you have: Medical Imaging, Main Floor, 11666 Laity St., Maple Ridge Fever above 38.5°C (101°F), aches and Royal Columbian Hospital 604-520-4640 Medical Imaging, Columbia Tower, 330 E. -

1 Delta Seniors Planning Team February 18, 2014 Benediction
Delta Seniors Planning Team February 18, 2014 Benediction Lutheran Church, Tsawwassen Minutes Chair: Val Windsor Recorder: Kay Dennison, Coordinator Attendance: Gerry Bouman, Don Browning, Lynda Brummitt, Kay Dennison, Ralph D’Souza, Lindsay Eldridge, Marg Kennett, Louise Long, Margaret Toews, Joanne Van Snellenberg, Val Windsor, George Winkelhorst, Lyn Walker, Sheila Zerr. Item Discussion/Information Action 1. Welcome Presentation: Judith McBride, Tsawwassen Stroke Recovery Group See notes of presentation at end of minutes 2. Approval of Agenda approved with addition - updates – Update from United Way Moved Val Windsor Agenda second Lindsay Eldridge 3. Approval of Minutes on the January 21, 2014 meeting approved as circulated Moved Val Windsor Minutes second Lindsay Eldridge 4. Follow up 4.1 Fraser Health Authority – Public Board meeting and request for from January information – Kay Dennison and Lynda Brummitt attended meeting Minutes and provided reports. Kay Dennison David Mitchell is the Chair of the Board and Dr. Nigel Murray, CEO welcomed a packed room at the Delta Town and Country Inn. After the formal meeting an open microphone was available to anyone wanting to ask questions or make a statement. David asked that people use the Fraser Health website to search out information. He gave the example of when there is a long wait for a surgeon you can go on the website and may find a surgeon in another 1 Item Discussion/Information Action community that would be available sooner. Information on Delta: Delta Hospital has the lowest infection rate in FHA - highest patient approval - fastest surgical recovery rate Delta Municipality has a good health status for seniors, healthier, better educated, better off financially and has a free bus service for seniors in North Delta. -

Ultrasound Guided Thyroid Biopsy Over…
When to get help Locations Abbotsford-Regional Hospital 604-851-4866 Call your doctor if you have any of the Medical Imaging 2nd Floor, Fraser Wing following: 32900 Marshall Road, Abbotsford BC Cancer Agency 604-877-6000 rd Fever above 38.5°C (101°F), aches, and Medical Imaging, 3 Floor chills 600 West 10th Ave, Vancouver Burnaby Hospital 604-434-4211 Increased pain or any redness at or Medical Imaging, 3rd Floor around the biopsy site 3935 Kincaid St., Burnaby Ultrasound Chilliwack General Hospital 604-795-4122 Medical Imaging, Main Floor Go to the nearest Emergency 45600 Menholm Rd, Chilliwack Guided Thyroid Department if you have any of the Delta Hospital 604-946-1121 following: Medical Imaging, 5800 Mountain View Boulevard, Delta Biopsy Jim Pattison Outpatient Care 604-533-3308 Swelling of the neck and Surgery Centre ext. 63926 Medical Imaging, 2nd Floor Severe weakness 9750 140th Street, Surrey Lions Gate Hospital 604-984-5775 Trouble breathing Medical Imaging, Lower Level th Trouble swallowing 231 East 15 Street, North Vancouver Peace Arch Hospital 604-531-5512 Medical Imaging, Main Floor 15521 Russell Ave, White Rock Richmond Hospital 604-278-9711 Medical Imaging, Main Floor 7000 Westminster Hwy, Richmond Ridge Meadows Hospital 604-463-1800 Medical Imaging, Main Floor 11666 Laity Street, Maple Ridge St. Paul’s Hospital 604-806-8006 Medical Imaging, 2nd Floor, Providence Building 1081 Burrard Street, Vancouver Surrey Memorial Hospital 604-588-3308 st Medical Imaging, 1 Floor, Lower Level th 13750 96 Avenue, Surrey HealthLinkBC 8-1-1 UBC Hospital 604-822-7076 Medical Imaging, Main Floor Call any time you have any questions or concerns. -

Fraser Health Authority
Consolidated Financial Statements of FRASER HEALTH AUTHORITY Year ended March 31, 2011 ABCD KPMG Enterprise™ Telephone (604) 527-3600 Metrotower II Fax (604) 527-3636 Suite 2400 - 4720 Kingsway Internet www.kpmg.ca/enterprise Burnaby BC V5H 4N2 Canada INDEPENDENT AUDITORS' REPORT To the Board of Fraser Health Authority We have audited the accompanying consolidated financial statements of the Fraser Health Authority ("the Entity"), which comprise the consolidated statement of financial position as at March 31, 2011 the consolidated statements of operations, changes in net assets (deficiency) and cash flows for the year then ended, and notes, comprising a summary of significant accounting policies and other explanatory information. Management's Responsibility for the Financial Statements Management is responsible for the preparation and fair presentation of these consolidated financial statements in accordance with Canadian generally accepted accounting principles, and for such internal control as management determines is necessary to enable the preparation of financial statements that are free from material misstatement, whether due to fraud or error. Auditor's Responsibility Our responsibility is to express an opinion on these consolidated financial statements based on our audit. We conducted our audit in accordance with Canadian generally accepted auditing standards. Those standards require that we comply with ethical requirements and plan and perform an audit to obtain reasonable assurance about whether the consolidated financial statements are free from material misstatement. An audit involves performing procedures to obtain audit evidence about the amounts and disclosures in the financial statements. The procedures selected depend on the auditor's judgment, including the assessment of the risks of material misstatement of the financial statements, whether due to fraud or error. -

PATH Unit Patient Assessment and Transition to Home
What you will need to bring: PATH Units in Fraser Health Appropriate footwear/street clothes Abbotsford Regional Hospital Toothbrush/Toothpaste/Denture 604 - 851-4849 cleaner / Shaving equipment Comb / Brush / Deodorant Burnaby Hospital 604 - 434-4211 Personal unscented creams or lotions Chilliwack General Hospital 604-795-4141 Special pillow or blanket Delta Hospital 604-946-1121 When you leave PATH Eagle Ridge Hospital PATH Unit The team will plan with you and 604-461-2022 your family for your return to home or community. Langley Memorial Hospital 604-534-4121 Patient Assessment You should ensure you have the and Transition following with you: Peace Arch Hospital 604 - 531-5512 All personal items to Home Medications from home and Queen’s Park Care Centre 604-519-8561 new prescriptions Dates and referrals for follow- Ridge Meadows Hospital 604-463-1822 up appointments You or your family are responsible Print Shop # 256155 for making follow-up appointments. PATH – Patient Assessment and Transition to Home PATH Working Together The PATH Team….. The PATH team is here to help The PATH unit will provide an You and your family you improve your ability to environment that promotes your Physician manage your care needs as strengths and abilities. The team Patient Care Coordinator independently as possible to will work with you and your family Quick Response Case Manager assist you in your transition to to develop a plan for your care Nursing Staff home or community. that is based on your needs. Care Aides Physiotherapist The team will keep you and your In order to maintain your well- Rehabilitation Assistant family informed of your care, being, the PATH team will Occupational Therapist share information, or review any encourage you to: Social Worker appropriate discharge planning. -
Community Resource Guide
Community Resource Guide Practical information when caring for a family member with a life-threatening illness at home. In every community there are people who care. Harold & Veronica Savage Centre for Supportive Care Operated by the Delta Hospice Society Hours: 9 am to 4 pm, Monday to Friday or by appointment Phone: 604-948-0660 Fax: 604-948-0651 Location: 4631 Clarence Taylor Crescent Delta, BC V4K 4L8 Irene Thomas Hospice Operated by the Delta Hospice Society Hours: 24 hour facility Phone: 604-948-4828 Fax: 604-948-4842 Location: 4635 Clarence Taylor Crescent Deta, BC V4K 4L8 Email: [email protected] Web: www.deltahospice.org 2 Table of Contents Page Introduction ...................................................................................................5 Caregivers ....................................................................................................6 Emergency Telephone Numbers ..................................................................7 Health Resources .........................................................................................8 Hospital Phone Numbers ..............................................................8 Home Care Nursing Services ........................................................9 Lifeline Program .........................................................................10 Respite .......................................................................................10 Adult Day Care ............................................................................10 Supportive -

Diagnostic Imaging
DIAGNOSTIC ACCREDITATION PROGRAM College of Physicians and Surgeons of British Columbia 300–669 Howe Street Telephone: 604-733-7758 Vancouver BC V6C 0B4 Toll free: 1-800-461-3008 (in BC) www.cpsbc.ca Fax: 604-733-3503 Accredited Facilities – Diagnostic Imaging As of 2021-09-20 Facility Name Address Scope of Expiry Date Organization Medical Director Accreditation of Accreditation 100 Mile District General Hospital 555 Cedar Drive Radiology 2023-04-19 Interior Health Authority Dr. Vipal Vedd 100 Mile House, BC, V0K 2E0 Abbotsford MRI Clinic Suite 5 - 2151 McCallum Road Magnetic Resonance 2024-09-04 Fraser Health Authority Dr. Amarjit Bajwa Abbotsford, BC, V2S 3N8 Imaging Abbotsford Regional Hospital and 32900 Marshall Road Radiology, Ultrasound, 2024-02-27 Fraser Health Authority Dr. Amarjit Bajwa Cancer Centre Abbotsford, BC, V2S 1K2 Computed Tomography, Nuclear Medicine, Mammography, Echocardiography, Magnetic Resonance Imaging, Bone Densitometry Abbotsford Regional Hospital and 32900 Marshall Road Vascular Ultrasound - 2025-12-17 Fraser Health Authority Dr. Husain Khambati Cancer Centre - Vascular Lab Abbotsford, BC, V2S 0C2 Limited Scope Aberdeen Ultrasound and X-Ray 272 - 1320 W. Trans Canada Hwy Radiology, Ultrasound 2025-02-05 Aberdeen Ultrasound Dr. Micheal Burns Kamloops, BC, V1S 1J2 and X-Ray Access MRI 104 - 15137 56 Avenue Magnetic Resonance 2026-02-10 Access MRI Dr. Spencer Lister Surrey, BC, V3S 9A5 Imaging, Ultrasound, Echocardiography AIM Medical Imaging Inc. 1371 West Broadway Magnetic Resonance 2024-10-24 AIM Medical Imaging Dr. Raj Attariwala Vancouver, BC, V6H 1G9 Imaging Inc. Arrow Lakes Hospital 97 1st Avenue NE Radiology 2023-04-10 Interior Health Authority Dr. -

393059 Delta Hospice.Indd
Community Resource Guide Practical information when caring for a family member with a life-threatening illness at home In every community there are people who care. Harold & Veronica Savage Centre for Supportive Care Operated by the Delta Hospice Society Hours: 9 am to 4 pm, Monday to Friday or by appointment Phone: 604-948-0660 Fax: 604-948-0651 Location: 4631 Clarence Taylor Crescent Delta, BC V4K 4L8 Irene Thomas Hospice Operated by the Delta Hospice Society Hours: 24 hour facility Phone: 604-948-4828 Fax: 604-948-4842 Location: 4635 Clarence Taylor Crescent Delta, BC V4K 4L8 Email: [email protected] Web: www.deltahospice.org Table of Contents Page Introduction …………………………………………..... 1 Caregivers ……………………………………………….. 2 Emergency Telephone Numbers ……………………. 3 Health Resources …………………………………....... 4 Hospital Phone Numbers................................. 4 Home Care Nursing Services ……………………. 5 Lifeline Program ……………………………………. 6 Respite ……………………………………………….. 6 Adult Day Care ……………………………………… 6 Supportive & End of Life Care …………………... 7 Hospice Societies & Hospice Residences ...……. 7 Community Services …………………………………… 8 Support in Daily Living …..………………………. 8 Deltassist Family & Community Services ……. 9 Delta Hospice – Centre for Supportive Care … 10 Other Support Services ………………………………. 11 Medical Equipment & Supplies …………………..... 13 Transportation …………………………………………. 16 Financial Services …………………………………….. 17 Legal Services ………………………………………….. 19 Counselling Services …………………………………. 20 Support Groups ………………………………….……. 21 i Table of Contents -

Delta Hospital Services
Delta Hospital Services Delta Council Regular Meeting March 9, 2015 Background • 1980: 0pened as a full service hospital. • 2002: FHA budget cuts resulted in closure of acute surgical program and critical care unit and Delta Hospital downgraded from acute to sub-acute care facility. Background • 2003-2008: community campaign to restore services – Declaration of Dependence. • Community fund-raising gradually restored many services and added new services eg. CT scanner. • 2008: regained status as acute care facility but surgical program remained downgraded to day surgery only. Background • 2009 – surgical program budget cut by $1.2 million. • Since then there has been a gradual erosion of services through budget cuts and loss of professional staff – difficulty recruiting and retaining specialists eg. anesthetists. Voicing Concerns • In October 2014, the Delta Hospital Medical Staff Association wrote to the Minister of Health regarding an “impending medical crisis” at Delta Hospital. • Requested immediate restoration of 4 surgical acute care beds. Patient Transfers • Operating rooms at Delta Hospital close at 3pm and weekends. • 150 patients a year transferred from Delta Hospital to other hospitals for emergency surgeries. • Increased costs (average $700 per patient transferred), time and patient stress. Orthopaedic Program • Need for comprehensive orthopaedic program, which would include a cast clinic. • Historical connections between Delta, Richmond and Vancouver but patients are now being directed to New Westminster. • Challenging for seniors or people without cars to go for follow-up appointments. Psychiatric Beds • No psychiatric beds at Delta Hospital. • Options – police custody, Surrey Memorial Emergency Dept. or release back to the community. • Significant drain on police resources. • Patients not getting proper treatment – cycle repeats itself.