RETRACTED – Effects of Sahaj Samadhi Meditation on Heart Rate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Microcosmic Alchemical Tantrik Architecture of Hangseshwari Temple तेज ो यत्ते रूपं कल्य
The Microcosmic Alchemical Tantrik Architecture of Hangseshwari Temple तेजो यते रपं कलाणतमं तते पशािम योऽसावसौ पुरषः सोऽहमिस ॥१६॥ tejo yat te rūpaṃ kalyāṇatamaṃ tat te paśyāmi yo 'sāv [asau puruṣaḥ] so'ham asmi "The light which is thy fairest form, I see it. I am what He is" ~ Isha Upanishad (verse 16), One of the most beautiful, alchemical, castle-like temples is the Hangseshwari Temple of the Hoogy District of Bengal. It is the spiritual center of a Tantrik astral dream sect that inspired a King to build this temple in a dream, combining the Mother Goddess with his own mother's symbolic name into one of the most beautiful Tantrik temples in the world. We use this temple and its symbolism to introduce key teachings, practices and symbols and invite those interested to inquire for further details in our alchemical missionary work. The Hangeshwari Temple has been called the abode of “Our Lady of the Cosmic Goose” by scholars aware of the alchemical significance. This name combines alchemically with the Black Virgin in the Western Tradition, as well as the alchemical immortals of diverse traditions. This temple is a true example of “Tantrik Satchakrabhed" or the “sat-chakra-bhed or piercing of the chakra nerve plexuses.” This is sacred Tantrik architecture expressing the microcosm in the temple's structure, which is symbolic of the Human Body. Built by wise sthapatis (temple architects), these temples encode the divine proportions and inner secrets of the microcosm and subtle body in sacred architectural principles dating back to the Vastu Shastra, which may be the oldest known architectural treatise in the world. -

Use of Theses
THESES SIS/LIBRARY TELEPHONE: +61 2 6125 4631 R.G. MENZIES LIBRARY BUILDING NO:2 FACSIMILE: +61 2 6125 4063 THE AUSTRALIAN NATIONAL UNIVERSITY EMAIL: [email protected] CANBERRA ACT 0200 AUSTRALIA USE OF THESES This copy is supplied for purposes of private study and research only. Passages from the thesis may not be copied or closely paraphrased without the written consent of the author. THE PRATYUTPANNA-BUDDHA-SAMMUKHAVASTHITA- SAMADHI-SUTRA AN ANNOTATED ENGLISH TRANSLATION OF THE TIBETAN VERSION WITH SEVERAL APPENDICES A Thesis submitted for the Degree of Doctor of Philosophy in the Australian National University August, 1979 by Paul Harrison This thesis is based on my own research carried out from 1976 to 1979 at the Australian National University. ABSTRACT The present work consists of a study of the Pratyutpanna-buddha- sammukhavasthita-samadhi-sutra (hereafter: PraS), a relatively early example of Mahayana Buddhist canonical literature. After a brief Intro duction (pp. xxi-xli), which attempts to place the PraS in its historical context, the major portion of the work (pp. 1-186) is devoted to an annotated English translation of the Tibetan version of the sutra, with detailed reference to the three main Chinese translations. Appendix A (pp. 187-252) then attempts a resolution of some of the many problems surrounding the various Chinese versions of the PraS. These are examined both from the point of view of internal evidence and on the basis of bibliographical information furnished by the Chinese Buddhist scripture-catalogues. Some tentative conclusions are advanced concerning the textual history of the PraS in China. -

1. Hamsa Sandesam V1
Thirumaliruncholai Thirupathi Thiruvarangam ThiruveLLarai Thirukkacchi Sincere Thanks To: 1. Smt.Krishnapriya for compilation of source document 2. Smt.Jayashree Muralidharan for eBook assembly sadagopan.org C O N T E N T S Introduction 1 Hamsa Sandesam - Rahasyartham 6 sadagopan.org sadagopan.org Swami Desikan - Satyagalam (Thanks:Sri.Laskhminarasimhan Sridhar) . ïI>. ïImte ingmaNtmhadeizkay nm> . INTRODUCTION sadagopan.org I want to share with you the tribute that Swami Desikan paid to Sri Ranganatha through one of his Kavyams known as Hamsa sandesam. The other Kavyams of Swami Desikan are: Subhashitaneevi, Yadavaabhudhyam and Padhuka Sahasram. Hamsa Sandesam is what is known as a Sandesa Kavyam. This Kavyam follows the style of AandaaL and Nammazhwar, when they requested clouds, birds and bees to take a message to their Lord and asked them to help in uniting them with their beloved Lord. In more recent times, Poet Kalidasa Composed Megha Sandesam, where he asks NamperumAL - SrIRangam (Thanks: Sri. Murali BhaTTar) 1 the hurrying clouds to take a message to his beloved one in the Northern region. Swami Desikan sets Hamsa Sandesam as a Kavyam, where Sri Ramachandra languishing from the sorrow of separation from His beloved Sita sights a Raja Hamsam and implores it to take a southward journey to Lankapuri and asks the hamsam to convey to Sita his sense of anguish and inconsolable desolation. There are 110 slokas in this Kavyam set by Swami Desikan in the Mandaakrantha Meter. Sri Rama points out the landmarks that the hamsam will fly over in its southward journey. In this Kavyam, we get a glimpse of the Sarva Tantra Swatantrar’s extraordinary knowledge about the geography of Bharata Desam. -

Yamas and Niyamas.Pdf
Yamas & Niyamas Teacher Training Yamas and Niyamas What are the Yamas and Niyamas? The Yamas and Niyamas are yoga's ten ethical guidelines and are the first two limbs of Yoga's eight-limbed path (Yama, Niyama, Asana, Pranayama, Pratyahara, Dharana, Dhyana and Samadhi). http://en.wikipedia.org/wiki/Yoga_Sutras_of_Patanjali EIGHT LIMBS 1. Yama ~ Moral restraints (how to behave in society) - outer 2. Niyama ~ The personal disciplines (your private practices) - outer 3. Asana ~ Physical postures - outer 4. Pranayama ~ Controlling the breath - outer 5. Pratyahara ~ Sense withdrawal – outer 6. Dharana ~ Intense focus, concentration - inner 7. Dhyana ~ Meditation - inner 8. Samadhi ~ Bliss, Joy, Peace - inner Where and when did the Yamas and Niyamas Originate? Many attribute the text of the Yamas and Niyamas to Patañjali therefore dating it to 2nd century BCE. Others believe the Yamas and Niyamas are a collection of fragments and traditions of texts stemming from the second or third century, not necessarily written by Patañjali. Still others provide an even wider period of potential composition of between 100 BCE and 500 CE. Beginning the Journey (Yamas) Living ethically, according to Patanjali's Yoga Sutra, is the first step on the true path of yoga. By Judith Lasater http://www.yogajournal.com/wisdom/462 When our children were young, my husband and I would occasionally summon up the courage to take them out for dinner. Before entering the restaurant, one of us would remind them to "be good" or we would leave. This warning was only mildly successful, but then one day my husband reasoned out a more effective approach. -

Notes on the Avatamsaka Sutra
View metadata, citation and similar papers at core.ac.uk brought to you by CORE NOTES ON THE AVATAMSAKA SUTRA bpO understand the Avatamsaka Sutra, the following remarks -®- will be found useful. Besides the general Mahayana notions, the Avatamsaka has its own philosophy or world-conception constituting the fundamental tenets of the Kegon School of Buddhism, which is regarded by some to be the culmination of the Buddhist experience of life. First, the Buddha as the central figure naturally occupies the most important position throughout the discourse. Un like in the other sutras, the Buddha himself does not deliver a sermon, or a series of sermons; all the lecturing whatever there is done by the attending Bodhisattvas: not only the lecturing but the praising of the Buddha’s holy merits, of which there is a great deal in this sutra, in fact more than in other sutras,—all this is the doing of the Bodhisattvas. The part played by the Buddha is just to show himself in radiance, and this is the important point in the understanding of the Avatamsaka. The Buddha here is not the historical Buddha, but one in the Sagara-mudra Samadhi, which means “ Ocean-Seal Samadhi.” According to Kegon scholars, the Buddha in this Samadhi keeps his mind so serene and transparent as the ocean in which all things are sealed or im pressed, that is, reflected as they are in themselves; the world thus appearing to him is not a world of the senses, but one of light and spirit. This world is called the Dharmadhatu, that is a world of pure beings, or simply a spiritual world, and is technically known as the “ World of the Lotus Treasure.” When the world is contemplated by the Buddha in this Samadhi, it is radiant with light; for the light issues from 234 THE EASTERN BUDDHIST his body, from every part of his body, in fact from every pore in his skin, illuminating the ten quarters of the universe and revealing the past, the present, and the future. -

The Serpent Power by Woodroffe Illustrations, Tables, Highlights and Images by Veeraswamy Krishnaraj
The Serpent Power by Woodroffe Illustrations, Tables, Highlights and Images by Veeraswamy Krishnaraj This PDF file contains the complete book of the Serpent Power as listed below. 1) THE SIX CENTRES AND THE SERPENT POWER By WOODROFFE. 2) Ṣaṭ-Cakra-Nirūpaṇa, Six-Cakra Investigation: Description of and Investigation into the Six Bodily Centers by Tantrik Purnananda-Svami (1526 CE). 3) THE FIVEFOLD FOOTSTOOL (PĀDUKĀ-PAÑCAKA THE SIX CENTRES AND THE SERPENT POWER See the diagram in the next page. INTRODUCTION PAGE 1 THE two Sanskrit works here translated---Ṣat-cakra-nirūpaṇa (" Description of the Six Centres, or Cakras") and Pādukāpañcaka (" Fivefold footstool ")-deal with a particular form of Tantrik Yoga named Kuṇḍalinī -Yoga or, as some works call it, Bhūta-śuddhi, These names refer to the Kuṇḍalinī-Śakti, or Supreme Power in the human body by the arousing of which the Yoga is achieved, and to the purification of the Elements of the body (Bhūta-śuddhi) which takes place upon that event. This Yoga is effected by a process technically known as Ṣat-cakra-bheda, or piercing of the Six Centres or Regions (Cakra) or Lotuses (Padma) of the body (which the work describes) by the agency of Kuṇḍalinī- Sakti, which, in order to give it an English name, I have here called the Serpent Power.1 Kuṇḍala means coiled. The power is the Goddess (Devī) Kuṇḍalinī, or that which is coiled; for Her form is that of a coiled and sleeping serpent in the lowest bodily centre, at the base of the spinal column, until by the means described She is aroused in that Yoga which is named after Her. -

Om: One God Universal a Garland of Holy Offerings * * * * * * * * Viveka Leads to Ānanda
Om: One God Universal A Garland of Holy Offerings * * * * * * * * Viveka Leads To Ānanda VIVEKNANDA KENDRA PATRIKĀ Vol. 22 No. 2: AUGUST 1993 Represented By Murari and Sarla Nagar Truth is One God is Truth . God is One Om Shanti Mandiram Columbia MO 2001 The treasure was lost. We have regained it. This publication is not fully satisfactory. There is a tremendous scope for its improvement. Then why to publish it? The alternative was to let it get recycled. There is a popular saying in American academic circles: Publish or Perish. The only justification we have is to preserve the valuable contents for posterity. Yet it is one hundred times better than its original. We have devoted a great deal of our time, money, and energy to improve it. The entire work was recomposed on computer. Figures [pictures] were scanned and inserted. Diacritical marks were provided as far as possible. References to citations were given in certain cases. But when a vessel is already too dirty it is very difficult to clean it even in a dozen attempts. The original was an assemblage of scattered articles written by specialists in their own field. Some were extracted from publications already published. It was issued as a special number of a journal. It needed a competent editor. Even that too was not adequate unless the editor possessed sufficient knowledge of and full competence in all the subject areas covered. One way to make it correct and complete was to prepare a kind of draft and circulate it among all the writers, or among those who could critically examine a particular paper in their respective field. -

Disentangling the Neural Mechanisms Involved in Hinduism- And
Brain and Cognition 90 (2014) 32–40 Contents lists available at ScienceDirect Brain and Cognition journal homepage: www.elsevier.com/locate/b&c Disentangling the neural mechanisms involved in Hinduism- and Buddhism-related meditations ⇑ Barbara Tomasino a, , Alberto Chiesa b,c, Franco Fabbro a,d a Department of Human Science, University of Udine, Italy b Department of Biomedical and NeuroMotor Sciences, University of Bologna, Italy c Department of Clinical and Experimental Medicine, University of Messina, Italy d Perceptual Robotics (PERCRO) Laboratory, Scuola Superiore Sant’Anna, Pisa, Italy article info abstract Article history: The most diffuse forms of meditation derive from Hinduism and Buddhism spiritual traditions. Different Accepted 20 March 2014 cognitive processes are set in place to reach these meditation states. According to an historical-philolog- Available online 27 June 2014 ical hypothesis (Wynne, 2009) the two forms of meditation could be disentangled. While mindfulness is the focus of Buddhist meditation reached by focusing sustained attention on the body, on breathing and Keywords: on the content of the thoughts, reaching an ineffable state of nothigness accompanied by a loss of sense of Meditation self and duality (Samadhi) is the main focus of Hinduism-inspired meditation. It is possible that these dif- Mindfulness ferent practices activate separate brain networks. We tested this hypothesis by conducting an activation Yoga likelihood estimation (ALE) meta-analysis of functional magnetic resonance imaging (fMRI) studies. The Executive attention Default system network related to Buddhism-inspired meditation (16 experiments, 263 subjects, and 96 activation foci) Superior medial gyrus included activations in some frontal lobe structures associated with executive attention, possibly confirming the fundamental role of mindfulness shared by many Buddhist meditations. -

Freedom of Religion and the Indian Supreme Court: The
FREEDOM OF RELIGION AND THE INDIAN SUPREME COURT: THE RELIGIOUS DENOMINATION AND ESSENTIAL PRACTICES TESTS A THESIS SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI‘I AT MĀNOA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS IN RELIGION MAY 2019 By Coleman D. Williams Thesis Committee: Ramdas Lamb, Chairperson Helen Baroni Ned Bertz Abstract As a religiously diverse society and self-proclaimed secular state, India is an ideal setting to explore the complex and often controversial intersections between religion and law. The religious freedom clauses of the Indian Constitution allow for the state to regulate and restrict certain activities associated with religious practice. By interpreting the constitutional provisions for religious freedom, the judiciary plays an important role in determining the extent to which the state can lawfully regulate religious affairs. This thesis seeks to historicize the related development of two jurisprudential tests employed by the Supreme Court of India: the religious denomination test and the essential practices test. The religious denomination test gives the Court the authority to determine which groups constitute religious denominations, and therefore, qualify for legal protection. The essential practices test limits the constitutional protection of religious practices to those that are deemed ‘essential’ to the respective faith. From their origins in the 1950s up to their application in contemporary cases on religious freedom, these two tests have served to limit the scope of legal protection under the Constitution and legitimize the interventionist tendencies of the Indian state. Additionally, this thesis will discuss the principles behind the operation of the two tests, their most prominent criticisms, and the potential implications of the Court’s approach. -
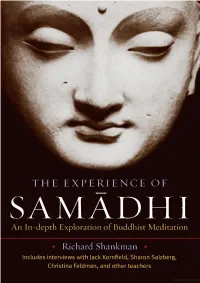
Experience of Samadhi
THE EXPERIENCE OF SAM API 11 An In-depth Exploration of Buddhist Meditation ■ Richard Shan km an ■ Includes interviews with Jack Kornfield, Sharon Salzberg, Christina Feldman, and other teachers The Experience of Samadhi THE EXPERIENCE OF SAMADHI An In-depth Exploration of Buddhist Meditation Richard Shankman SHAMBHALA Boston & London 2 0 0 8 Shambhala Publications, Inc. Horticultural Hall 300 Massachusetts Avenue Boston, Massachusetts 02115 •^^w.shambhala.com © 2008 by Richard Shankman Pages 219-20 constitute a continuation of the copyright page. A l rights reserved. No part of this book may be reproduced in any form or by any means, electronic or mechanical, including photocopying, recording, orby any information storage and retrieval system, without permission in writing from the publisher. 987654321 First Edition Printed in Canada @ This edition is printed on acid-free paper that meets the American National Standards Institute Z39.48 Standard. O This book was printed on 100% postconsumer recycled paper. For more information please visit us at •^^w.shambhala.com. Distributed in the United States by Random House, Inc., and in Canada by Random. House of Canada Ltd Interior design and composition: Greta D. Sibley & Associates Library of Congress Cataloging-in-Publication- Data Shankman, Richard. The experience of samadhi: an in-depth exploration of Buddhist meditation / Richard Shankman.—1st ed. p. cm. ■ Includes bibliographical references and index. ISBN 978-1-59030-521-8 (pbk.: alk. paper) 1. Samadhi. 2. Buddhist literature, Pali—History and criticism. 3. Buddhists—Interviews. 1. Title. BQ5630.S16S43 2008 294^3 '4435 DC22 2008017613 CONTENTS Preface | ix Acknowledgments | xii Introduction | xiii PART ONE SAMADHI IN THE PALI TEXTS I. -

Concept of Redemption in the World Religions: a Comparative Analysis of the Account of Redemption in Semitic Religions and Indian Religions
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 21, Issue 3, Ver. I (Mar. 2016) PP 53-64 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Concept of Redemption in the World Religions: A Comparative Analysis of the Account of Redemption in Semitic Religions and Indian Religions Binoj Mathew, Research Scholar, Bharatiyar University, Coimbatore. I. Introduction The ultimate aim of any religion is salvation / redemption of those who believe in it. They embark various paths to experience redemption according to their beliefs and the life of the founders and prominent figures of these religions. Redemption is a common word in the world religions including the Semitic Religions and the Indian Religions. The Semitic Religions are Judaism, Christianity and Islam and the Indian Religions includes Hinduism, Jainism, Buddhism and Sikhism. Semitic Religions are monotheistic for they believe in one God. They hold fast to the belief of the creation of the world out of nothing and God alone is eternal and all the other things like soul, matter, and scripture are created. Whereas the Indian Religions like Buddhism, Jainism and Sikhism have their origin from Hinduism. According to Hinduism, God, Soul, Matter and Scripture are eternal. They believe not in one God but many. In Semitic Religion, salvation is the saving of the soul from sin and its consequences. It may also be called „deliverance‟ or „redemption‟ from sin and its effects. Salvation is considered to be caused either by the free will and grace of a deity or by personal efforts through prayer, asceticism, or some combination of the two. -

Internationalisation of a Contemporary Hindu Movement Alexis Avdeeff
Internationalisation of a contemporary Hindu Movement Alexis Avdeeff To cite this version: Alexis Avdeeff. Internationalisation of a contemporary Hindu Movement: Between universalist ambi- tion and nationalist orientations: the case of The Art of Living Foundation (Vyakti vikas Kendra) and its transnational community. 21th European Conference on Modern South Asian Studies (ECMSAS) - Panel 41 - ”Religious Reform Movements in South Asia from Nineteenth Century to the Present” convened by Professor Gwilym Beckerlegge (The Open University, Manchester), Jul 2010, Bonn, Germany. hal-00975129 HAL Id: hal-00975129 https://hal.archives-ouvertes.fr/hal-00975129 Submitted on 8 Apr 2014 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Internationalisation of a contemporary Hindu Movement Between universalist ambition and nationalist orientations: the case of The Art of Living Foundation (Vyakti vikas Kendra) and its transnational community1 Alexis Avdeeff PhD in Social and Historical Anthropology, EHESS (Toulouse) (LISST-CAS, UMR 5193) The Art of Living Foundation, also known in India as Vyakti Vikas Kendra2, is a new religious movement whose popularity has not ceased to grow in the whole Indian sub- continent, and beyond. Founded and carried out by Sri Sri Ravi Shankar – “the fastest growing guru in the market place of happiness”3 – the movement promotes a spirituality accessible to all, based on simplified yogic practices and a philosophical teaching of neo- vedantic inspiration.