Can Hepatic Coma Be Caused by a Reduction of Brain Noradrenaline Or Dopamine?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FSI-D-16-00226R1 Title
Elsevier Editorial System(tm) for Forensic Science International Manuscript Draft Manuscript Number: FSI-D-16-00226R1 Title: An overview of Emerging and New Psychoactive Substances in the United Kingdom Article Type: Review Article Keywords: New Psychoactive Substances Psychostimulants Lefetamine Hallucinogens LSD Derivatives Benzodiazepines Corresponding Author: Prof. Simon Gibbons, Corresponding Author's Institution: UCL School of Pharmacy First Author: Simon Gibbons Order of Authors: Simon Gibbons; Shruti Beharry Abstract: The purpose of this review is to identify emerging or new psychoactive substances (NPS) by undertaking an online survey of the UK NPS market and to gather any data from online drug fora and published literature. Drugs from four main classes of NPS were identified: psychostimulants, dissociative anaesthetics, hallucinogens (phenylalkylamine-based and lysergamide-based materials) and finally benzodiazepines. For inclusion in the review the 'user reviews' on drugs fora were selected based on whether or not the particular NPS of interest was used alone or in combination. NPS that were use alone were considered. Each of the classes contained drugs that are modelled on existing illegal materials and are now covered by the UK New Psychoactive Substances Bill in 2016. Suggested Reviewers: Title Page (with authors and addresses) An overview of Emerging and New Psychoactive Substances in the United Kingdom Shruti Beharry and Simon Gibbons1 Research Department of Pharmaceutical and Biological Chemistry UCL School of Pharmacy -

MDPV Bath Salts Test
One Step Methylenedioxypyrovalerone Drug of Abuse Test MATERIALS Analytical Sensitivity The cut-off concentration of the One Step Methylenedioxypyrovalerone Drug of Abuse Test is determined to be 1,000ng/mL. (Dip Card) Materials Provided: Test was run in 30 replicates with negative urine and standard control at ±25% cut-off and ±50% cut-off concentration levels. Test results ● Dip cards are summarized below. For Forensic Use Only ● Desiccants ● Package insert Test Result INTENDED USE Percent of Cut-off n Materials Required But Not Provided: Methylenedioxypyrovalerone Concentration in ng/mL The One Step Methylenedioxypyrovalerone Drug of Abuse Test is a lateral flow chromatographic immunoassay for the ● Specimen collection container Negative Positive qualitative detection of Methylenedioxypyrovalerone (MDPV) in human urine specimen at the cut-off level of 1,000ng/mL. This ● Disposable gloves 0% Cut-off assay is intended for forensic use only. ● Timer 30 30 0 This assay provides only a preliminary qualitative test result. A more specific confirmatory reference method, such as Liquid (No Drug Present) chromatogra -50% Cut-off phy tandem mass spectrometry (LC/MS/MS) or gas chromatography/mass spectrometry (GC/MS) must be use in INSTRUCTIONS FOR USE] 30 30 0 order to obtain a confirmed analytical result. (500ng/mL) 1) Remove the dip card from the foil pouch. -25% Cut-off 30 30 0 BACKGROUND 2) Remove the cap from the dip card. Label the device with patient or control identifications. (750ng/mL) 3) Immerse the absorbent tip into the urine sample for 5 seconds. Urine sample should not touch the plastic device. Cut-off ‘Bath salts’, a form of designer drugs, also promoted as ‘plant food’ or ‘research chemicals’, is sold mainly in head shops, on 4) Replace the cap over the absorbent tip and lay the dip card on a clean, flat, and non-absorptive surface. -

Octopamine and Tyramine Regulate the Activity of Reproductive Visceral Muscles in the Adult Female Blood-Feeding Bug, Rhodnius Prolixus Sam Hana* and Angela B
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 1830-1836 doi:10.1242/jeb.156307 RESEARCH ARTICLE Octopamine and tyramine regulate the activity of reproductive visceral muscles in the adult female blood-feeding bug, Rhodnius prolixus Sam Hana* and Angela B. Lange ABSTRACT Monastirioti et al., 1996). Octopamine and tyramine signal via The role of octopamine and tyramine in regulating spontaneous G-protein coupled receptors (GPCRs), leading to changes in second contractions of reproductive tissues was examined in the messenger levels. The recently updated receptor classification α β female Rhodnius prolixus. Octopamine decreased the amplitude of (Farooqui, 2012) divides the receptors into Oct -R, Oct -Rs β β β spontaneous contractions of the oviducts and reduced RhoprFIRFa- (Oct 1-R, Oct 2-R, Oct 3-R), TYR1-R and TYR2-R. In general, β α induced contractions in a dose-dependent manner, whereas tyramine Oct -Rs lead to elevation of cAMP while Oct -R and TYR-Rs lead to 2+ only reduced the RhoprFIRFa-induced contractions. Both octopamine an increase in Ca (Farooqui, 2012). and tyramine decreased the frequency of spontaneous bursal The movement of eggs in the reproductive system of contractions and completely abolished the contractions at Rhodnius prolixus starts at the ovaries, the site of egg maturation. 5×10−7 mol l−1 and above. Phentolamine, an octopamine receptor Upon ovulation, mature eggs are released into the oviducts antagonist, attenuated the inhibition induced by octopamine on the (Wigglesworth, 1942). Eggs are then guided, via oviductal oviducts and the bursa. Octopamine also increased the levels of peristaltic and phasic contractions, to the common oviduct, where cAMP in the oviducts, and this effect was blocked by phentolamine. -

Structure-Cytotoxicity Relationship Profile of 13 Synthetic Cathinones In
Neurotoxicology 75 (2019) 158–173 Contents lists available at ScienceDirect Neurotoxicology journal homepage: www.elsevier.com/locate/neuro Structure-cytotoxicity relationship profile of 13 synthetic cathinones in differentiated human SH-SY5Y neuronal cells T ⁎ Jorge Soaresa, , Vera Marisa Costaa, Helena Gasparb,c, Susana Santosd,e, Maria de Lourdes Bastosa, ⁎ Félix Carvalhoa, João Paulo Capelaa,f, a UCIBIO, REQUIMTE (Rede de Química e Tecnologia), Laboratório de Toxicologia, Departamento de Ciências Biológicas, Faculdade de Farmácia, Universidade do Porto, Portugal b BioISI – Instituto de Biossistemas e Ciências Integrativas, Faculdade de Ciências, Universidade de Lisboa, Portugal c MARE - Centro de Ciências do Mar e do Ambiente, Escola Superior de Turismo e Tecnologia do Mar, Instituto Politécnico de Leiria, Portugal d Centro de Química e Bioquímica (CQB), Departamento de Química e Bioquímica, Faculdade de Ciências, Universidade de Lisboa, Portugal e Centro de Química Estrutural, Faculdade de Ciências, Universidade de Lisboa, Portugal f FP-ENAS (Unidade de Investigação UFP em Energia, Ambiente e Saúde), CEBIMED (Centro de Estudos em Biomedicina), Faculdade de Ciências da Saúde, Universidade Fernando Pessoa, Portugal ARTICLE INFO ABSTRACT Keywords: Synthetic cathinones also known as β-keto amphetamines are a new group of recreational designer drugs. We Synthetic cathinones aimed to evaluate the cytotoxic potential of thirteen cathinones lacking the methylenedioxy ring and establish a Classical amphetamines putative structure-toxicity profile using differentiated SH-SY5Y cells, as well as to compare their toxicity to that Cytotoxicity of amphetamine (AMPH) and methamphetamine (METH). Cytotoxicity assays [mitochondrial 3-(4,5-dimethyl-2- SH-SY5Y cells thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) reduction and lysosomal neutral red (NR) uptake] per- Structure-toxicity relationship formed after a 24-h or a 48-h exposure revealed for all tested drugs a concentration-dependent toxicity. -

Octopamine Regulates Sleep Indrosophilathrough Protein Kinase A-Dependent Mechanisms
The Journal of Neuroscience, September 17, 2008 • 28(38):9377–9385 • 9377 Behavioral/Systems/Cognitive Octopamine Regulates Sleep in Drosophila through Protein Kinase A-Dependent Mechanisms Amanda Crocker and Amita Sehgal Department of Neuroscience, Howard Hughes Medical Institute, University of Pennsylvania, Philadelphia, Pennsylvania 19104 Sleep is a fundamental process, but its regulation and function are still not well understood. The Drosophila model for sleep provides a powerful system to address the genetic and molecular mechanisms underlying sleep and wakefulness. Here we show that a Drosophila biogenic amine, octopamine, is a potent wake-promoting signal. Mutations in the octopamine biosynthesis pathway produced a pheno- type of increased sleep, which was restored to wild-type levels by pharmacological treatment with octopamine. Moreover, electrical silencing of octopamine-producing cells decreased wakefulness, whereas excitation of these neurons promoted wakefulness. Because protein kinase A (PKA) is a putative target of octopamine signaling and is also implicated in Drosophila sleep, we investigated its role in the effects of octopamine on sleep. We found that decreased PKA activity in neurons rendered flies insensitive to the wake-promoting effects of octopamine. However, this effect of PKA was not exerted in the mushroom bodies, a site previously associated with PKA action on sleep. These studies identify a novel pathway that regulates sleep in Drosophila. Key words: Drosophila; octopamine; sleep; locomotion; norepinephrine; biogenic amine; arousal Introduction The only arousal-promoting signal identified in Drosophila is Sleep is a core process that spans genetically diverse eukaryotes dopamine (Andretic et al., 2005; Kume et al., 2005). from mammals to arthropods (Tobler, 2005). -

Recent Trends in the Quantification of Biogenic Amines in Biofluids
Journal of Clinical Medicine Review Recent Trends in the Quantification of Biogenic Amines in Biofluids as Biomarkers of Various Disorders: A Review Alina Plenis 1,* , Ilona Ol˛edzka 1 , Piotr Kowalski 1 , Natalia Mi˛ekus 1,2 and Tomasz B ˛aczek 1 1 Department of Pharmaceutical Chemistry, Medical University of Gda´nsk,Hallera 107, 80-416 Gda´nsk, Poland; [email protected] (I.O.); [email protected] (P.K.); [email protected] (N.M.); [email protected] (T.B.) 2 Department of Animal and Human Physiology, Faculty of Biology, University of Gda´nsk,Wita Stwosza 59, 80-308 Gda´nsk,Poland * Correspondence: [email protected]; Fax: +48-58-349-16-35 Received: 4 April 2019; Accepted: 6 May 2019; Published: 9 May 2019 Abstract: Biogenic amines (BAs) are bioactive endogenous compounds which play a significant physiological role in many cell processes like cell proliferation and differentiation, signal transduction and membrane stability. Likewise, they are important in the regulation of body temperature, the increase/decrease of blood pressure or intake of nutrition, as well as in the synthesis of nucleic acids and proteins, hormones and alkaloids. Additionally, it was confirmed that these compounds can be considered as useful biomarkers for the diagnosis, therapy and prognosis of several neuroendocrine and cardiovascular disorders, including neuroendocrine tumours (NET), schizophrenia and Parkinson’s Disease. Due to the fact that BAs are chemically unstable, light-sensitive and possess a high tendency for spontaneous oxidation and decomposition at high pH values, their determination is a real challenge. Moreover, their concentrations in biological matrices are extremely low. -

Methedrine, Neo-Synephrine, Paredrine, and Pholedrine
Br Heart J: first published as 10.1136/hrt.6.4.214 on 1 October 1944. Downloaded from CLINICAL EVALUATION OF THE PRESSOR ACTIVITY OF METHEDRINE, NEO-SYNEPHRINE, PAREDRINE, AND PHOLEDRINE BY FREDERICK PRESCOTT From the Wellcome Research Institution, London Received October 10, 1944 Recently a number of pressor drugs of the adrenaline type have come into clinical use for the treatment of low blood pressure following surgical procedures, spinal anxsthesia, circu- latory collapse, and surgical and traumatic shock. For therapeutic purposes the ideal pressor drug should be effective by the intramuscular or intravenous route; it should act rapidly; it should produce a sustained elevation of blood pressure, so that frequent injections of the drug are not necessary; and it should have no undesirable effects on the cardiovascular system and no untoward side effects. Adrenaline and ephedrine were the first drugs to be used clinically to raise the blood pressure in cases of operative shock. Their limitations, however, are nowv well known. Adrenaline may do more harm than good beca4se in thera- peutic doses intrayenously it causes a considerable rise of blood pressure, e.g. 200 mm. to 300 mm. of mercury, with a precipitous fall after a few minutes to a level lower than before. Similarly ephedrine, which for dependable results must be given intravenously, produces a http://heart.bmj.com/ sharp rise of blood pressure that lasts only for ten to twenty minutes. Other pressor drugs have been introduced with a more sustained action. In most of the studies reported on these, however, no definite criteria seem to have been employed in their evaluation, nor have the conditions of administration been standardized. -

Catecholamines and the Hydroxylation of Tyrosine in Synaptosomes Isolated from Rat Brain (DOPA/Tyramine/Dopamine/Norepinephrine/Octopamine) M
Proc. Nat. Acad. Sci. USA Vol. 68, No. 10, pp. 2370-2373, October 1971 Catecholamines and the Hydroxylation of Tyrosine in Synaptosomes Isolated from Rat Brain (DOPA/tyramine/dopamine/norepinephrine/octopamine) M. KAROBATH Psychiatric Research Laboratories, Massachusetts General Hospital, Boston, Mass. 02114 Communicated by Seymour S. Kety, July 16, 1971 ABSTRACT Tyrosine hydroxylase activity of synapto- removing transmitters from an extraneuronal location at the somes isolated from rat brain was examined. A modified synapse, then incubation of synaptosomes with catechol- tritium-displacement assay was used, which allowed the measurement of tyrosine hydroxylase activity without the amines should inhibit the formation of DOPA from tyrosine. addition of either inhibitors of the metabolism of the The experiments demonstrate that tyrosine hydroxylase hydroxylated products or added exogenous cofactor. The activity is affected by catecholamine uptake. The concentra- enzyme activity was strongly inhibited by the addition of tions required to inhibit the synthesis of catechols are in the exogenous catecholamines and 3,4-dihydroxy-L-phenyl- M. alanine. Aromatic amines other than catechols did not range of 10-7 markedly influence tyrosine hydroxylase activity. These MATERIALS AND METHODS in vitro findings support the hypothesis that synthesis of catecholamines is regulated by a mechanism of end- [3,5-H]HifTyrosine (Tracerlab) was purified by column chro- product inhibition at the tyrosine hydroxylase step. matography. Catechol impurities were absorbed on alumina and tritiated water and anions were removed by Synaptosomes are pinched-off nerve endings with relatively columns (8), by non-neuronal elements (1, 2). They absorption on Dowex-50 resin. Tyrosine was eluted from little contamination Dowex-50 with 25 ml of 4 N HCl; after distillation of the eluate contain the enzymes necessary for the synthesis of dopamine (v/v) from tyrosine (3, 4). -
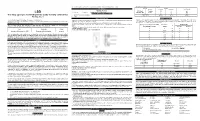
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Amphetamine, 3,4
0026-895X/01/6006-1181–1188$3.00 MOLECULAR PHARMACOLOGY Vol. 60, No. 6 Copyright © 2001 The American Society for Pharmacology and Experimental Therapeutics 1304/951292 Mol Pharmacol 60:1181–1188, 2001 Printed in U.S.A. ACCELERATED COMMUNICATION Amphetamine, 3,4-Methylenedioxymethamphetamine, Lysergic Acid Diethylamide, and Metabolites of the Catecholamine Neurotransmitters Are Agonists of a Rat Trace Amine Receptor JAMES R. BUNZOW, MARK S. SONDERS, SEKSIRI ARTTAMANGKUL, LAURA M. HARRISON, GE ZHANG, DENISE I. QUIGLEY, TRISTAN DARLAND, KATHERINE L. SUCHLAND, SHAILAJA PASUMAMULA, JAMES L. KENNEDY, SUSAN B. OLSON, R. ELLEN MAGENIS, SUSAN G. AMARA, and DAVID K. GRANDY Departments of Physiology & Pharmacology (J.R.B., S.A., L.M.H., G.Z., D.I.Q., T.D., K.L.S., S.P., S.B.O., R.E.M., D.K.G.) and Molecular and Medical Genetics (S.B.O., R.E.M), School of Medicine, the Vollum Institute (M.S.S., S.G.A.), and the Howard Hughes Medical Institute (S.G.A.), Oregon Health & Science University, Portland, Oregon; and Centre for Addiction and Mental Health, University of Toronto, Canada (J.L.K.) Received August 21, 2001; accepted September 28, 2001 This paper is available online at http://molpharm.aspetjournals.org ABSTRACT The trace amine para-tyramine is structurally and functionally re- goline derivatives, adrenergic ligands, and 3-methylated metabo- lated to the amphetamines and the biogenic amine neurotrans- lites of the catecholamine neurotransmitters are also good ago- mitters. It is currently thought that the biological activities elicited nists at the rat trace amine receptor 1 (rTAR1). These results by trace amines such as p-tyramine and the psychostimulant suggest that the trace amines and catecholamine metabolites amphetamines are manifestations of their ability to inhibit the may serve as the endogenous ligands of a novel intercellular clearance of extracellular transmitter and/or stimulate the efflux of signaling system found widely throughout the vertebrate brain and transmitter from intracellular stores. -

'Bath Salts' Constituents MDPV, Mephedrone, and Methylone Serena Allen East Tennessee State University
East Tennessee State University Digital Commons @ East Tennessee State University Electronic Theses and Dissertations Student Works 5-2018 The ombinedC Neuropharmacology and Toxicology of Major 'Bath Salts' Constituents MDPV, Mephedrone, and Methylone Serena Allen East Tennessee State University Follow this and additional works at: https://dc.etsu.edu/etd Part of the Medicinal Chemistry and Pharmaceutics Commons, Neuroscience and Neurobiology Commons, Pharmacology Commons, Pharmacy and Pharmaceutical Sciences Commons, and the Toxicology Commons Recommended Citation Allen, Serena, "The ombC ined Neuropharmacology and Toxicology of Major 'Bath Salts' Constituents MDPV, Mephedrone, and Methylone" (2018). Electronic Theses and Dissertations. Paper 3431. https://dc.etsu.edu/etd/3431 This Dissertation - Open Access is brought to you for free and open access by the Student Works at Digital Commons @ East Tennessee State University. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons @ East Tennessee State University. For more information, please contact [email protected]. The Combined Neuropharmacology and Toxicology of Major ‘Bath Salts’ Constituents MDPV, Mephedrone, and Methylone A dissertation presented to the faculty of the Department of Biomedical Sciences East Tennessee State University In partial fulfillment of the requirements for the degree Doctor of Philosophy in Biomedical Sciences, Pharmaceutical Science Concentration by Serena A. Allen May 2018 Dr. Brooks Pond, -

Adrenergic-Like Octopamine Receptor Affects Locomotion and Reproduction of Tribolium Castaneum
International Journal of Molecular Sciences Article Knockdown of a β-Adrenergic-Like Octopamine Receptor Affects Locomotion and Reproduction of Tribolium castaneum Li-Sha Zheng 1,2,†, Xiao-Qiang Liu 1,3,†, Ge-Ge Liu 1, Qian-Qiao Huang 1, Jin-Jun Wang 1,2 and Hong-Bo Jiang 1,2,* 1 Key Laboratory of Entomology and Pest Control Engineering, College of Plant Protection, Southwest University, Chongqing 400715, China; [email protected] (L.-S.Z.); [email protected] (X.-Q.L.); [email protected] (G.-G.L.); [email protected] (Q.-Q.H.); [email protected] (J.-J.W.) 2 Academy of Agricultural Sciences, Southwest University, Chongqing 400715, China 3 Laboratory of Integrated Pest Management on Tropical Crops, Environment and Plant Protection Institute, Chinese Academy of Tropical Agriculture Sciences, Ministry of Agriculture, Haikou 570100, China * Correspondence: [email protected]; Tel.: +86-23-6825-0255; Fax: +86-23-6825-1269 † These authors contributed equally to this work. Abstract: The neurohormone octopamine regulates many crucial physiological processes in insects and exerts its activity via typical G-protein coupled receptors. The roles of octopamine receptors in regulating behavior and physiology in Coleoptera (beetles) need better understanding. We used the red flour beetle, Tribolium castaneum, as a model species to study the contribution of the octopamine receptor to behavior and physiology. We cloned the cDNA of a β-adrenergic-like octopamine receptor (TcOctb2R). This was heterologously expressed in human embryonic kidney (HEK) 293 cells and Citation: Zheng, L.-S.; Liu, X.-Q.; was demonstrated to be functional using an in vitro cyclic AMP assay.