Adrenaline and Nebulized Salbutamol in Acute Asthma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FSI-D-16-00226R1 Title
Elsevier Editorial System(tm) for Forensic Science International Manuscript Draft Manuscript Number: FSI-D-16-00226R1 Title: An overview of Emerging and New Psychoactive Substances in the United Kingdom Article Type: Review Article Keywords: New Psychoactive Substances Psychostimulants Lefetamine Hallucinogens LSD Derivatives Benzodiazepines Corresponding Author: Prof. Simon Gibbons, Corresponding Author's Institution: UCL School of Pharmacy First Author: Simon Gibbons Order of Authors: Simon Gibbons; Shruti Beharry Abstract: The purpose of this review is to identify emerging or new psychoactive substances (NPS) by undertaking an online survey of the UK NPS market and to gather any data from online drug fora and published literature. Drugs from four main classes of NPS were identified: psychostimulants, dissociative anaesthetics, hallucinogens (phenylalkylamine-based and lysergamide-based materials) and finally benzodiazepines. For inclusion in the review the 'user reviews' on drugs fora were selected based on whether or not the particular NPS of interest was used alone or in combination. NPS that were use alone were considered. Each of the classes contained drugs that are modelled on existing illegal materials and are now covered by the UK New Psychoactive Substances Bill in 2016. Suggested Reviewers: Title Page (with authors and addresses) An overview of Emerging and New Psychoactive Substances in the United Kingdom Shruti Beharry and Simon Gibbons1 Research Department of Pharmaceutical and Biological Chemistry UCL School of Pharmacy -

Octopamine and Tyramine Regulate the Activity of Reproductive Visceral Muscles in the Adult Female Blood-Feeding Bug, Rhodnius Prolixus Sam Hana* and Angela B
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 1830-1836 doi:10.1242/jeb.156307 RESEARCH ARTICLE Octopamine and tyramine regulate the activity of reproductive visceral muscles in the adult female blood-feeding bug, Rhodnius prolixus Sam Hana* and Angela B. Lange ABSTRACT Monastirioti et al., 1996). Octopamine and tyramine signal via The role of octopamine and tyramine in regulating spontaneous G-protein coupled receptors (GPCRs), leading to changes in second contractions of reproductive tissues was examined in the messenger levels. The recently updated receptor classification α β female Rhodnius prolixus. Octopamine decreased the amplitude of (Farooqui, 2012) divides the receptors into Oct -R, Oct -Rs β β β spontaneous contractions of the oviducts and reduced RhoprFIRFa- (Oct 1-R, Oct 2-R, Oct 3-R), TYR1-R and TYR2-R. In general, β α induced contractions in a dose-dependent manner, whereas tyramine Oct -Rs lead to elevation of cAMP while Oct -R and TYR-Rs lead to 2+ only reduced the RhoprFIRFa-induced contractions. Both octopamine an increase in Ca (Farooqui, 2012). and tyramine decreased the frequency of spontaneous bursal The movement of eggs in the reproductive system of contractions and completely abolished the contractions at Rhodnius prolixus starts at the ovaries, the site of egg maturation. 5×10−7 mol l−1 and above. Phentolamine, an octopamine receptor Upon ovulation, mature eggs are released into the oviducts antagonist, attenuated the inhibition induced by octopamine on the (Wigglesworth, 1942). Eggs are then guided, via oviductal oviducts and the bursa. Octopamine also increased the levels of peristaltic and phasic contractions, to the common oviduct, where cAMP in the oviducts, and this effect was blocked by phentolamine. -
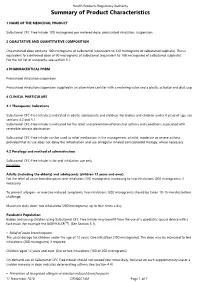
Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE MEDICINAL PRODUCT Salbutamol CFC-Free Inhaler 100 micrograms per metered dose, pressurised inhalation, suspension 2 QUALITATIVE AND QUANTITATIVE COMPOSITION One metered dose contains 100 micrograms of salbutamol (equivalent to 120 micrograms of salbutamol sulphate). This is equivalent to a delivered dose of 90 micrograms of salbutamol (equivalent to 108 micrograms of salbutamol sulphate). For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Pressurised inhalation suspension Pressurised inhalation suspension supplied in an aluminium canister with a metering valve and a plastic actuator and dust cap. 4 CLINICAL PARTICULARS 4.1 Therapeutic Indications Salbutamol CFC-Free Inhaler is indicated in adults, adolescents and children. For babies and children under 4 years of age, see sections 4.2 and 5.1. Salbutamol CFC-Free Inhaler is indicated for the relief and prevention of bronchial asthma and conditions associated with reversible airways obstruction. Salbutamol CFC-Free Inhaler can be used as relief medication in the management of mild, moderate or severe asthma, provided that its use does not delay the introduction and use of regular inhaled corticosteroid therapy, where necessary. 4.2 Posology and method of administration Salbutamol CFC-Free Inhaler is for oral inhalation use only. Posology Adults (including the elderly) and adolescents (children 12 years and over): For the relief of acute bronchospasm, one inhalation (100 micrograms) increasing to two inhalations (200 micrograms), if necessary. To prevent allergen- or exercise-induced symptoms, two inhalations (200 micrograms) should be taken 10-15 minutes before challenge. Maximum daily dose: two inhalations (200 micrograms) up to four times a day. -

Can Hepatic Coma Be Caused by a Reduction of Brain Noradrenaline Or Dopamine?
Gut: first published as 10.1136/gut.18.9.688 on 1 September 1977. Downloaded from Gut, 1977, 18, 688-691 Can hepatic coma be caused by a reduction of brain noradrenaline or dopamine? L. ZIEVE AND R. L. OLSEN From the Department ofMedicine, Minneapolis Veterans Hospital, University of Minnesota, Minneapolis, and Department of Chemistry, Hamline University, St. Paul, Minnesota, USA SUMMARY Intraventricular infusions of octopamine which raised brain octopamine concentrations more than 20 000-fold resulted in reductions in brain noradrenaline and dopamine by as much as 90% without affecting the alertness or activity of normal rats. As this reduction of brain catechol- amines is much greater than any reported in hepatic coma, we do not believe that values observed in experimental hepatic failure have aetiological significance for the encephalopathy that ensues. Though catecholaminergic nerve terminals represent dopamine and noradrenaline had no discernible only a small proportion of brain synapses (Snyder et effect on the state of alertness of the animals. al., 1973), the reduction in brain dopamine or nor- adrenaline by the accumulation of false neuro- Methods transmitterssuch as octopamine or of aromaticamino acids such as phenylalanine or tyrosine has been ANIMALS suggested as a cause of hepatic coma (Fischer and Male Sprague-Dawley rats weighing between 300 and Baldessarini, 1971; Dodsworth et al., 1974; Fischer 350 were g prepared by the method of Peterson and http://gut.bmj.com/ and Baldessarini, 1975; Munro et al., 1975). The Sparber (1974) for intraventricular infusions of following data have been cited in support of this octopamine. Rats of 250-400 g were used as controls. -

Supporting Information a Analysed Substances
Electronic Supplementary Material (ESI) for Analyst. This journal is © The Royal Society of Chemistry 2020 List of contents: Tab. A1 Detailed list and classification of analysed substances. Tab. A2 List of selected MS/MS parameters for the analytes. Tab. A1 Detailed list and classification of analysed substances. drug of therapeutic doping agent analytical standard substance abuse drug (WADA class)* supplier (+\-)-amphetamine ✓ ✓ S6 stimulants LGC (+\-)-methamphetamine ✓ S6 stimulants LGC (+\-)-3,4-methylenedioxymethamphetamine (MDMA) ✓ S6 stimulants LGC methylhexanamine (4-methylhexan-2-amine, DMAA) S6 stimulants Sigma cocaine ✓ ✓ S6 stimulants LGC methylphenidate ✓ ✓ S6 stimulants LGC nikethamide (N,N-diethylnicotinamide) ✓ S6 stimulants Aldrich strychnine S6 stimulants Sigma (-)-Δ9-tetrahydrocannabinol (THC) ✓ ✓ S8 cannabinoids LGC (-)-11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THC-COOH) S8 cannabinoids LGC morphine ✓ ✓ S7 narcotics LGC heroin (diacetylmorphine) ✓ ✓ S7 narcotics LGC hydrocodone ✓ ✓ Cerillant® oxycodone ✓ ✓ S7 narcotics LGC (+\-)-methadone ✓ ✓ S7 narcotics Cerillant® buprenorphine ✓ ✓ S7 narcotics Cerillant® fentanyl ✓ ✓ S7 narcotics LGC ketamine ✓ ✓ LGC phencyclidine (PCP) ✓ S0 non-approved substances LGC lysergic acid diethylamide (LSD) ✓ S0 non-approved substances LGC psilocybin ✓ S0 non-approved substances Cerillant® alprazolam ✓ ✓ LGC clonazepam ✓ ✓ Cerillant® flunitrazepam ✓ ✓ LGC zolpidem ✓ ✓ LGC VETRANAL™ boldenone (Δ1-testosterone / 1-dehydrotestosterone) ✓ S1 anabolic agents (Sigma-Aldrich) -

Structure-Cytotoxicity Relationship Profile of 13 Synthetic Cathinones In
Neurotoxicology 75 (2019) 158–173 Contents lists available at ScienceDirect Neurotoxicology journal homepage: www.elsevier.com/locate/neuro Structure-cytotoxicity relationship profile of 13 synthetic cathinones in differentiated human SH-SY5Y neuronal cells T ⁎ Jorge Soaresa, , Vera Marisa Costaa, Helena Gasparb,c, Susana Santosd,e, Maria de Lourdes Bastosa, ⁎ Félix Carvalhoa, João Paulo Capelaa,f, a UCIBIO, REQUIMTE (Rede de Química e Tecnologia), Laboratório de Toxicologia, Departamento de Ciências Biológicas, Faculdade de Farmácia, Universidade do Porto, Portugal b BioISI – Instituto de Biossistemas e Ciências Integrativas, Faculdade de Ciências, Universidade de Lisboa, Portugal c MARE - Centro de Ciências do Mar e do Ambiente, Escola Superior de Turismo e Tecnologia do Mar, Instituto Politécnico de Leiria, Portugal d Centro de Química e Bioquímica (CQB), Departamento de Química e Bioquímica, Faculdade de Ciências, Universidade de Lisboa, Portugal e Centro de Química Estrutural, Faculdade de Ciências, Universidade de Lisboa, Portugal f FP-ENAS (Unidade de Investigação UFP em Energia, Ambiente e Saúde), CEBIMED (Centro de Estudos em Biomedicina), Faculdade de Ciências da Saúde, Universidade Fernando Pessoa, Portugal ARTICLE INFO ABSTRACT Keywords: Synthetic cathinones also known as β-keto amphetamines are a new group of recreational designer drugs. We Synthetic cathinones aimed to evaluate the cytotoxic potential of thirteen cathinones lacking the methylenedioxy ring and establish a Classical amphetamines putative structure-toxicity profile using differentiated SH-SY5Y cells, as well as to compare their toxicity to that Cytotoxicity of amphetamine (AMPH) and methamphetamine (METH). Cytotoxicity assays [mitochondrial 3-(4,5-dimethyl-2- SH-SY5Y cells thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) reduction and lysosomal neutral red (NR) uptake] per- Structure-toxicity relationship formed after a 24-h or a 48-h exposure revealed for all tested drugs a concentration-dependent toxicity. -

Prodrugs Design Based on Inter- and Intramolecular Chemical Processes
Chem Biol Drug Des 2013; 82: 643–668 Review Prodrugs Design Based on Inter- and Intramolecular Chemical Processes Rafik Karaman1,2,* compound satisfies a number of preset criteria to start clinical development. The number of years it takes to intro- 1Bioorganic Chemistry Department, Faculty of Pharmacy, duce a drug to the pharmaceutical market is over 10 years Al-Quds University, P.O. Box 20002, Jerusalem, Palestine with a cost of more than $1 billion dollars (1,2). 2Department of Science, University of Basilicata, Via dell’Ateneo Lucano 10, 85100, Potenza, Italy Modifying the absorption, distribution, metabolism, and *Corresponding author: Rafik Karaman, elimination (ADME) properties of an active drug requires a [email protected] complete understanding of the physicochemical and bio- logical behavior of the drug candidate (3 6). This includes This review provides the reader a concise overview of – the majority of prodrug approaches with the emphasis comprehensive evaluation of drug-likeness involving on the modern approaches to prodrug design. The prediction of ADME properties. These predictions can be chemical approach catalyzed by metabolic enzymes attempted at several levels: in vitro–in vivo using data which is considered as widely used among all other obtained from tissue or recombinant material from human approaches to minimize the undesirable drug physico- and preclinical species, and in silico or computational pre- chemical properties is discussed. Part of this review dictions projecting in vitro or in vivo data, involving the will shed light on the use of molecular orbital methods evaluation of various ADME properties, using computa- such as DFT, semiempirical and ab initio for the design tional approaches such as quantitative structure activity of novel prodrugs. -

The 2013 "Research on Drug Evidence"
The 2013 “Research on Drug Evidence” Report [From the 17th ICPO / INTERPOL Forensic Science Symposium] Robert F. X. Klein U.S. Department of Justice Drug Enforcement Administration Special Testing and Research Laboratory 22624 Dulles Summit Court Dulles, VA 20166 [[email protected]] ABSTRACT: A reprint of the 2013 “Research on Drug Evidence” Report (a review) is provided. KEYWORDS: INTERPOL, Illicit Drugs, Controlled Substances, Forensic Chemistry. Important Information: Distributed at the 17th ICPO / INTERPOL Forensic Science Symposium, Lyon, France, October 8 - 10, 2013.* Authorized Reprint. Copyright INTERPOL. All rights reserved. May not be reprinted without express permission from INTERPOL. For pertinent background, see: Klein RFX. ICPO / INTERPOL Forensic Science Symposia, 1995 - 2016. “Research on Drug Evidence”. Prefacing Remarks (and a Request for Information). Microgram Journal 2016;13(1-4):1-3. Citations in this report from the Journal of the Clandestine Laboratory Investigating Chemists Association were (and remain) Law Enforcement Restricted. The "General Overview" (Talking Paper) was removed from this reprint (Editor's discretion). This reprint is derived from the original electronic document, and is not an image of the best available hard copy (as was utilized for the 1995 and 1998 reports). For this reason, the pagination in the Proceedings is not retained in this reprint, some minor reformatting was done to eliminate deadspace, and all widow and orphan lines were left as is. [* Due to travel restrictions in effect in late 2013, this report and the associated "General Overview" (Talking Paper) was not actually presented, but rather the report was only distributed to the attendees.] Microgram Journal 2016, Volume 13; Numbers 1-4 511 Research on Drug Evidence January 1, 2010 - June 30, 2013 Presented by: Jeffrey H. -

Annex 2B Tariff Schedule of the United States See General Notes to Annex 2B for Staging Explanation HTSUS No
Annex 2B Tariff Schedule of the United States See General Notes to Annex 2B for Staging Explanation HTSUS No. Description Base Rate Staging 0101 Live horses, asses, mules and hinnies: 0101.10.00 -Purebred breeding animals Free E 0101.90 -Other: 0101.90.10 --Horses Free E 0101.90.20 --Asses 6.8% B --Mules and hinnies: 0101.90.30 ---Imported for immediate slaughter Free E 0101.90.40 ---Other 4.5% A 0102 Live bovine animals: 0102.10.00 -Purebred breeding animals Free E 0102.90 -Other: 0102.90.20 --Cows imported specially for dairy purposes Free E 0102.90.40 --Other 1 cent/kg A 0103 Live swine: 0103.10.00 -Purebred breeding animals Free E -Other: 0103.91.00 --Weighing less than 50 kg each Free E 0103.92.00 --Weighing 50 kg or more each Free E 0104 Live sheep and goats: 0104.10.00 -Sheep Free E 0104.20.00 -Goats 68 cents/head A 0105 Live poultry of the following kinds: Chickens, ducks, geese, turkeys and guineas: -Weighing not more than 185 g: 0105.11.00 --Chickens 0.9 cents each A 0105.12.00 --Turkeys 0.9 cents each A 0105.19.00 --Other 0.9 cents each A -Other: 0105.92.00 --Chickens, weighing not more than 2,000 g 2 cents/kg A 0105.93.00 --Chickens, weighing more than 2,000 g 2 cents/kg A 0105.99.00 --Other 2 cents/kg A 0106 Other live animals: -Mammals: 0106.11.00 --Primates Free E 0106.12.00 --Whales, dolphins and porpoises (mammals of the order Cetacea); manatees and dugongs (mammals of the order Sirenia) Free E 0106.19 --Other: 2B-Schedule-1 HTSUS No. -

Orciprenaline Sulphate (Alupent): Planned Withdrawal from the UK Market Following a Risk-Benefit Analysis
MHRA PUBLIC ASSESSMENT REPORT Orciprenaline sulphate (Alupent): planned withdrawal from the UK market following a risk-benefit analysis November 2009 Executive summary 2 1. Introduction 3 2. Summary of data 3 2.1 Clinical pharmacology 3 2.2 Efficacy 3 2.3 Safety 4 3. Conclusions 8 4. References 9 5. Glossary 10 1 EXECUTIVE SUMMARY (Please note that this summary is intended to be accessible to all members of the public, including health professionals) Background The Medicines and Healthcare products Regulatory Agency (MHRA) is the government agency responsible for regulating the effectiveness and safety of medicines and medical devices in the UK. We continually review the safety of all medicines in the UK, and inform healthcare professionals and the public of the latest safety updates. In our Public Assessment Reports, we discuss the evidence for a safety issue with a particular drug or drug class, and changes made to the product information for the drug on the basis of this evidence, which will help safeguard public health. This MHRA Public Assessment Report discusses a review of the risks and benefits of a medicine called orciprenaline sulphate. Orciprenaline sulphate is available for oral administration as a syrup used to treat reversible airways obstructiona, which is a symptom of asthmab and chronic obstructive pulmonary diseasec. It acts on specific areas in the body called β- receptors, which relaxes the muscles used for breathing and opens the airways in the lungs. Orciprenaline sulphate was licensed in 1972 and is marketed in the UK under the brand name Alupent Syrup. As with any medicine, the use of orciprenaline sulphate may lead to adverse reactions (side-effects) in some individuals, which are described in the product information, including the patient information leaflet (see the Electronic Medicines Compendium (product information) website). -

Methedrine, Neo-Synephrine, Paredrine, and Pholedrine
Br Heart J: first published as 10.1136/hrt.6.4.214 on 1 October 1944. Downloaded from CLINICAL EVALUATION OF THE PRESSOR ACTIVITY OF METHEDRINE, NEO-SYNEPHRINE, PAREDRINE, AND PHOLEDRINE BY FREDERICK PRESCOTT From the Wellcome Research Institution, London Received October 10, 1944 Recently a number of pressor drugs of the adrenaline type have come into clinical use for the treatment of low blood pressure following surgical procedures, spinal anxsthesia, circu- latory collapse, and surgical and traumatic shock. For therapeutic purposes the ideal pressor drug should be effective by the intramuscular or intravenous route; it should act rapidly; it should produce a sustained elevation of blood pressure, so that frequent injections of the drug are not necessary; and it should have no undesirable effects on the cardiovascular system and no untoward side effects. Adrenaline and ephedrine were the first drugs to be used clinically to raise the blood pressure in cases of operative shock. Their limitations, however, are nowv well known. Adrenaline may do more harm than good beca4se in thera- peutic doses intrayenously it causes a considerable rise of blood pressure, e.g. 200 mm. to 300 mm. of mercury, with a precipitous fall after a few minutes to a level lower than before. Similarly ephedrine, which for dependable results must be given intravenously, produces a http://heart.bmj.com/ sharp rise of blood pressure that lasts only for ten to twenty minutes. Other pressor drugs have been introduced with a more sustained action. In most of the studies reported on these, however, no definite criteria seem to have been employed in their evaluation, nor have the conditions of administration been standardized. -

The Organic Chemistry of Drug Synthesis
The Organic Chemistry of Drug Synthesis VOLUME 2 DANIEL LEDNICER Mead Johnson and Company Evansville, Indiana LESTER A. MITSCHER The University of Kansas School of Pharmacy Department of Medicinal Chemistry Lawrence, Kansas A WILEY-INTERSCIENCE PUBLICATION JOHN WILEY AND SONS, New York • Chichester • Brisbane • Toronto Copyright © 1980 by John Wiley & Sons, Inc. All rights reserved. Published simultaneously in Canada. Reproduction or translation of any part of this work beyond that permitted by Sections 107 or 108 of the 1976 United States Copyright Act without the permission of the copyright owner is unlawful. Requests for permission or further information should be addressed to the Permissions Department, John Wiley & Sons, Inc. Library of Congress Cataloging in Publication Data: Lednicer, Daniel, 1929- The organic chemistry of drug synthesis. "A Wiley-lnterscience publication." 1. Chemistry, Medical and pharmaceutical. 2. Drugs. 3. Chemistry, Organic. I. Mitscher, Lester A., joint author. II. Title. RS421 .L423 615M 91 76-28387 ISBN 0-471-04392-3 Printed in the United States of America 10 987654321 It is our pleasure again to dedicate a book to our helpmeets: Beryle and Betty. "Has it ever occurred to you that medicinal chemists are just like compulsive gamblers: the next compound will be the real winner." R. L. Clark at the 16th National Medicinal Chemistry Symposium, June, 1978. vii Preface The reception accorded "Organic Chemistry of Drug Synthesis11 seems to us to indicate widespread interest in the organic chemistry involved in the search for new pharmaceutical agents. We are only too aware of the fact that the book deals with a limited segment of the field; the earlier volume cannot be considered either comprehensive or completely up to date.