The Pterygopalatine Fossa and Its Connections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -
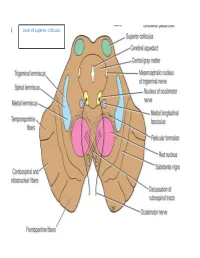
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Palatal Injection Does Not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth
Open Access Review Article DOI: 10.7759/cureus.2120 Palatal Injection does not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth Joe Iwanaga 1 , R. Shane Tubbs 2 1. Seattle Science Foundation 2. Neurosurgery, Seattle Science Foundation Corresponding author: Joe Iwanaga, [email protected] Abstract The superior alveolar nerves course lateral to the maxillary sinus and the greater palatine nerve travels through the hard palate. This difficult three-dimensional anatomy has led some dentists and oral surgeons to a critical misunderstanding in developing the anterior and middle superior alveolar (AMSA) nerve block and the palatal approach anterior superior alveolar (P-ASA) nerve block. In this review, the anatomy of the posterior, middle and anterior superior alveolar nerves, greater palatine nerve, and nasopalatine nerve are revisited in order to clarify the anatomy of these blocks so that the perpetuated anatomical misunderstanding is rectified. We conclude that the AMSA and P-ASA nerve blockades, as currently described, are not based on accurate anatomy. Categories: Anesthesiology, Medical Education, Other Keywords: anatomy, innervation, local anesthesia, maxillary nerve, nerve block, tooth Introduction And Background Anesthetic blockade of the posterior superior alveolar (PSA) branch of the maxillary nerve has played an important role in the endodontic treatment of irreversible acute pulpitis of the upper molar teeth except for the mesiobuccal root of the first molar tooth [1, 2]. This procedure requires precise anatomical knowledge of the pterygopalatine fossa and related structures in order to avoid unnecessary complications and to make the blockade most effective. The infraorbital nerve gives rise to middle superior alveolar (MSA) and anterior superior alveolar (ASA) branches. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

Endocrine Block اللهم ال سهل اال ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل
OSPE ENDOCRINE BLOCK اللهم ﻻ سهل اﻻ ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل Important Points 1. Don’t forget to mention right and left. 2. Read the questions carefully. 3. Make sure your write the FULL name of the structures with the correct spelling. Example: IVC ✕ Inferior Vena Cava ✓ Aorta ✕ Abdominal aorta ✓ 4. There is NO guarantee whether or not the exam will go out of this file. ممكن يأشرون على أجزاء مو معلمه فراح نحط بيانات إضافية حاولوا تمرون عليها كلها Good luck! Pituitary gland Identify: 1. Anterior and posterior clinoidal process of sella turcica. 2. Hypophyseal fossa (sella turcica) Theory • The pituitary gland is located in middle cranial fossa and protected in sella turcica (hypophyseal fossa) of body of sphenoid. Relations Of Pituitary Gland hypothalamus Identify: 1. Mamillary body (posteriorly) 2. Optic chiasma (anteriorly) 3. Sphenoidal air sinuses (inferior) 4. Body of sphenoid 5. Pituitary gland Theory • If pituitary gland became enlarged (e.g adenoma) it will cause pressure on optic chiasma and lead to bilateral temporal eye field blindness (bilateral hemianopia) Relations Of Pituitary Gland Important! Identify: 1. Pituitary gland. 2. Diaphragma sellae (superior) 3. Sphenoidal air sinuses (inferior) 4. Cavernous sinuses (lateral) 5. Abducent nerve 6. Oculomotor nerve 7. Trochlear nerve 8. Ophthalmic nerve 9. Trigeminal (Maxillary) nerve Structures of lateral wall 10. Internal carotid artery Note: Ophthalmic and maxillary are both branches of the trigeminal nerve Divisions of Pituitary Gland Identify: 1. Anterior lobe (Adenohypophysis) 2. Optic chiasma 3. Infundibulum 4. Posterior lobe (Neurohypophysis) Theory Anterior Lobe Posterior Lobe • Adenohypophysis • Neurohypophysis • Secretes hormones • Stores hormones • Vascular connection to • Neural connection to hypothalamus by hypothalamus by Subdivisions hypophyseal portal hypothalamo-hypophyseal system (from superior tract from supraoptic and hypophyseal artery) paraventricular nuclei. -

Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery
brain sciences Article Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery Grzegorz Wysiadecki 1,* , Maciej Radek 2 , R. Shane Tubbs 3,4,5,6,7 , Joe Iwanaga 3,5,8 , Jerzy Walocha 9 , Piotr Brzezi ´nski 10 and Michał Polguj 1 1 Department of Normal and Clinical Anatomy, Chair of Anatomy and Histology, Medical University of Lodz, ul. Zeligowskiego˙ 7/9, 90-752 Łód´z,Poland; [email protected] 2 Department of Neurosurgery, Spine and Peripheral Nerve Surgery, Medical University of Lodz, University Hospital WAM-CSW, 90-549 Łód´z,Poland; [email protected] 3 Department of Neurosurgery, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA; [email protected] (R.S.T.); [email protected] (J.I.) 4 Department of Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, LA 70433, USA 5 Department of Neurology, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA 6 Department of Anatomical Sciences, St. George’s University, Grenada FZ 818, West Indies 7 Department of Surgery, Tulane University School of Medicine, New Orleans, LA 70112, USA 8 Department of Anatomy, Kurume University School of Medicine, 67 Asahi-machi, Kurume, Fukuoka 830-0011, Japan Citation: Wysiadecki, G.; Radek, M.; 9 Department of Anatomy, Jagiellonian University Medical College, 33-332 Kraków, Poland; Tubbs, R.S.; Iwanaga, J.; Walocha, J.; [email protected] Brzezi´nski,P.; Polguj, M. -

The Anatomic Analysis of the Vidian Canal and the Surrounding
Braz J Otorhinolaryngol. 2019;85(2):136---143 Brazilian Journal of OTORHINOLARYNGOLOGY www.bjorl.org ORIGINAL ARTICLE The anatomic analysis of the vidian canal and the surrounding structures concerning vidian neurectomy ଝ using computed tomography scans a,∗ a b Gülay Ac¸ar , Aynur Emine C¸ic¸ekcibas¸ı , ˙Ibrahim C¸ukurova , c a d Kemal Emre Özen , Muzaffer ¸ekerS , ˙Ibrahim Güler a Necmettin Erbakan University, Meram Faculty of Medicine, Department of Anatomy, Konya, Turkey b Health Sciences University, Izmir Tepecik Trainig and Research Hospital, Department of Otolaryngology-Head and Neck Surgery, Izmir, Turkey c Katip C¸elebi University, Faculty of Medicine, Department of Anatomy, Izmir, Turkey d Selcuk University, Faculty of Medicine, Department of Radiology, Konya, Turkey Received 15 September 2017; accepted 8 November 2017 Available online 26 December 2017 KEYWORDS Abstract Intrasphenoid Introduction: The type of endoscopic approach chosen for vidian neurectomy can be specified septum; by evaluating the vidian canal and the surrounding sphenoid sinus structures. Morphometric Objective: The variations and morphometry of the vidian canal were investigated, focusing on analysis; the functional correlations between them which are crucial anatomical landmarks for preoper- Pterygoid process ative planning. pneumatization; Methods: This study was performed using paranasal multidetector computed tomography Vidian canal; images that were obtained with a section thickening of 0.625 mm of 250 adults. Vidian neurectomy Results: The distributions of 500 vidian canal variants were categorized as follows; Type 1, within the sphenoid corpus (55.6%); Type 2, partially protruding into the sphenoid sinus (34.8%); Type 3, within the sphenoid sinus (9.6%). The pneumatization of the pterygoid process is mostly seen in vidian canal Type 2 (72.4%) and Type 3 (95.8%) (p < 0.001). -

Orbital Malignant Peripheral Nerve Sheath Tumours
Br J Ophthalmol: first published as 10.1136/bjo.73.9.731 on 1 September 1989. Downloaded from British Journal of Ophthalmology, 1989, 73, 731-738 Orbital malignant peripheral nerve sheath tumours CHRISTOPHER J LYONS,' ALAN A McNAB,l ALEC GARNER,2 AND JOHN E WRIGHT' From the I Orbital clinic, Moorfields Eye Hospital, City Road, London EC] V 2PD, and the 2Department of Pathology, Institute ofOphthalmology, London EC] V 9A T SUMMARY We describe three patients with malignant peripheral nerve tumours in the orbit and review the existing literature on these rare lesions. Malignant peripheral nerve sheath tumours are Sensation was diminished over the distribution of the unusual in any part of the body and very rare in the second division of the right trigeminal nerve. The left orbit, where only 13 cases have previously been globe was normal. Plain anteroposterior skull x-rays described. These tumours can spread rapidly along showed a normal appearance, but undertilted the involved nerve to the middle cranial fossa. They occipitomental tomographic views revealed enlarge- are radioresistant, and total surgical excision offers ment of the right infraorbital canal (Fig. 1). copyright. the only hope of cure. Our experience with three An inferior orbital margin incision revealed patients may help clinicians to recognise these lesions tumour protruding from the infraorbital foramen and and excise them at an early stage. extending beneath the soft tissues of the cheek. The tumour had a firm consistency and a pale grey cut Case reports surface. The orbital periosteum on the floor of the orbit was elevated and a mass over 18 mm in diameter PATIENT 1 was found within an expanded infraorbital canal Four years prior to presentation a man which extended posteriorly into the superior orbital 55-year-old http://bjo.bmj.com/ noted a small lump at the medial end of his right fissure. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

Comparison of Greater Palatine Nerve Block with Intravenous Fentanyl for Postoperative Analgesia Following Palatoplasty in Children
Jemds.com Original Research Article Comparison of Greater Palatine Nerve Block with Intravenous Fentanyl for Postoperative Analgesia Following Palatoplasty in Children Amol Singam1, Saranya Rallabhandi2, Tapan Dhumey3 1Department of Anaesthesiology, JNMC, DMIMS, Sawangi Meghe, Wardha Maharashtra, India. 2Department of Anaesthesiology, JNMC, DMIMS, Sawangi Meghe, Wardha, Maharashtra, India. 3Department of Anaesthesiology, JNMC, DMIMS, Sawangi Meghe, Wardha, Maharashtra, India. ABSTRACT BACKGROUND Good pain relief after palatoplasty is important as inadequate analgesia with vigorous Corresponding Author: cry leads to wound dehiscence, removal of sutures and extra nursing care. Decrease Dr. Saranya Rallabhandi, in oxygen requirement and cardio-respiratory demand occur with good pain relief Assisstant Professor, and also promotes early recovery. Preoperative opioids have concerns like sedation, Department of Anesthesiology, AVBRH, DMIMS (DU), Sawangi Meghe, respiratory depression and airway compromise. Greater palatine nerve block with Wardha- 442001, Maharashtra, India. bupivacaine is safe and effective without the risk of respiratory depression. The study E-mail: [email protected] was done to compare pain relief postoperatively with intravenous fentanyl and greater palatine nerve block in children following palatoplasty. DOI: 10.14260/jemds/2020/549 METHODS How to Cite This Article: 80 children of ASA I & II, between 1 to 7 years were included and allocated into two Singam A, Rallabhandi S, Dhumey T. Comparison of greater palatine nerve block groups of 40 each. Analgesic medication was given preoperatively after induction of with intravenous fentanyl for postoperative general anaesthesia, children in Group B received greater palatine nerve block with analgesia following palatoplasty in -1 2 mL 0.25% inj. Bupivacaine (1 mL on each side) and Group F received 2 μg Kg I.V. -

Trigeminal Nerve, Mandibular Division Basic Anatomy and a Bit More
The palate and the faucial isthmus He who guards his mouth and his tongue keeps himself from calamity. Proverbs 21:23 Ph.D., Dr. David Lendvai Parts of the oral cavity Parts of the oral cavity 1. Vestibule of the oral cavity Borders: - lips and cheek (bucca) - dental arches 2. Oral cavity proper Borders: - roof: hard and soft palate - floor: oral diaphragm (mylohoid m.) - antero-laterally: dental arches - posteriorly: isthmus of the fauces Etrance of the oral cavity - Philtrum - Upper & lower lip - Angulus - Rubor labii - Nasolabial groove (Facial palsy) Sobotta Szentágothai - Réthelyi Aspectus anterior 1 zygomatic process 2 frontal process 2 4 alveolar process 1 4 Faller (left) lateral aspect 1 zygomatic process 2 frontal process 3 orbital surface 4 alveolar process 2 3 Sobotta 1 4 Faller (right) Medial aspect Sobotta Superior aspect Sobotta Inferior aspect Sobotta http://www.almanahmedical.eu Sobotta Florian Dental – Dr. S. Kovách Fehér Fehér Szél Szél http://www.hc-bios.com Structures of the hard palate - incisive papilla - palatine rugae - palatine raphe - torus Hard and soft palate Muscles of the soft palate - Levator veli palatini m. - Tensor veli palatini m. - Palatoglossus m. - Palatopharyngeus m. - M. uvulae Muscles of the soft palate Muscles of the soft palate Structures of the hard and soft palate - mucous membrane - palatine glands - bone / muscles Histology of the hard palate Mucoperiosteum Histology of the soft palate NASAL SURFACE - pseudostratified ciliated columnar epithelium - lamina propria - mucous glands - striated