Angiomyolipoma of the Kidneys: Current Perspectives and Challenges in Diagnostic Imaging and Image-Guided Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Angiomyolipoma of the Cervix – Report of a Rare Entity
Internet Journal of Medical Update. 2017 July;12(2):13-15. doi: 10.4314/ijmu.v12i2.4 Internet Journal of Medical Update Journal home page: http://www.akspublication.com/ijmu Case Report Angiomyolipoma of the cervix – report of a rare entity N. Hariharanadha Sarmaᴪ1, Rama Srivastava2, Smriti Agnihotri3 1Consultant Pathologist, Department of Pathology, RDT Hospital, Bathalapalli, Andhra Pradesh, India 2Professor, Department of Pathology, SSR Medical College, Belle Rive, Mauritius 3Professor, Department of Pathology, American University of Antigua College of Medicine, Antigua & Barbuda, WI (Received 22 September 2017 and accepted 04 October 2017) ABSTRACT: Angiomyolipoma (AML) is a mesenchymal neoplasm seen usually in the kidney. Few cases of extra renal AML have been documented in various organs including the female genital tract, where the uterus is the most common site. To the best of our knowledge, only 4 cases of AML in the cervix have been reported in the literature. Association of AML with tuberous sclerosis is well known. Presently AML is included in the spectrum of disease entities called PEComa. We report a case of AML without tuberous sclerosis arising from the uterine cervix, which has to be differentiated from lipoleiomyoma. KEY WORDS: Angiomyolipoma; Uterine cervix; PEComas; Uterine tumor INTRODUCTIONV localization8, and mostly in females over 409. The occurrence of AML in the cervix without Angiomyolipoma (AML) occurs most frequently in concurrent incidence in the kidney is extremely the kidney, where it is closely related to tuberous rare, and only four cases have been reported in the sclerosis complex (TSC)1,2, occasionally in other scientific literature10. We are reporting a case of organs, most commonly the liver, but occurrence at uterine cervix AML without tuberous sclerosis other sites is extremely rare3. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

Non-Wilms Renal Cell Tumors in Children
PEDIATRIC UROLOGIC ONCOLOGY 0094-0143/00 $15.00 + .OO NON-WILMS’ RENAL TUMORS IN CHILDREN Bruce Broecker, MD Renal tumors other than Wilms’ tumor are tastases occur in 40% to 60% of patients with infrequent in childhood. Wilms’ tumors ac- clear cell sarcoma of the kidney, whereas they count for 6% to 7% of childhood cancer, are found in less than 2% of patients with whereas the remaining renal tumors account Wilms’ tumor.**,26 This distinct clinical behav- for less than l%.27The most common non- ior is one of the features that has led to its Wilms‘ tumors are clear cell sarcoma of the designation as a separate tumor. Other clini- kidney, rhabdoid tumor of the kidney (both cal features include a lack of association with formerly considered unfavorable Wilms’ tu- sporadic aniridia or hemihypertrophy. mor variants but now considered separate tu- Clear cell sarcoma of the kidney has not mors), renal cell carcinoma, mesoblastic been reported to occur bilaterally and is not nephroma, and multilocular cystic nephroma. associated with nephroblastomatosis. It has Collectively, these tumors account for less been reported in infancy and adulthood, but than 10% of the primary renal neoplasms in the peak incidence is between 3 and 5 years childhood. of age. It has an aggressive behavior that responds poorly to treatment with vincristine and actinomycin alone, leading to its original CLEAR CELL SARCOMA designation by Beckwith as an unfavorable histology pattern. The addition of doxorubi- Clear cell sarcoma of the kidney is cur- cin in aggressive chemotherapy regimens has rently considered a separate tumor distinct improved outcome. -
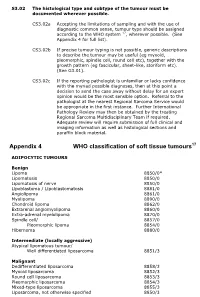
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

The Identification of a Girl with Tuberous Sclerosis and an Unexpected Large Sized Renal Angiomyolipoma: a Case Report and Literature Review Study
Case Report Annals of Clinical Case Reports Published: 24 Aug, 2020 The Identification of a Girl with Tuberous Sclerosis and an Unexpected Large Sized Renal Angiomyolipoma: A Case Report and Literature Review Study Mitra Naseri1, Farah Ashrafzadeh2, Fatemeh Ghalibafan3* and Paria Dehghanian4 1Department of Pediatric Nephrology, Mashhad University of Medical Sciences, Iran 2Department of Pediatric Neurology, Mashhad University of Medical Sciences, Iran 3Department of Medicine, Mashhad University of Medical Sciences, Iran 4Department of Pathology, Mashhad University of Medical Sciences, Iran Abstract Background: The TSC1 mutated gene, hamartin, and the TSC2 gene, tuberin, cause tuberous sclerosis, the autosomal dominant tumor syndrome. The angiomyolipoma of the kidney is a benign tumor that often happens along with tuberous sclerosis. Large renal angiomyolipoma’s associated with tuberous sclerosis are in danger of fatal hemorrhage. This study reported a case with an unexpected large size of renal angiomyolipoma’s associated with tuberous sclerosis. Case Presentation: We report a girl aged 5 years and 9 months old with tuberous sclerosis who referred to nephrology clinic due to abdominal pain. Physical examination revealed a large mass in the right flank. Kidney ultrasound reported a large mass with approximate size of 90 mm × 60 mm in the right kidney, and abdominal CT scan also showed a non-hemogenic solid mass in the right kidney with size of 91 mm × 68 mm × 67 mm, was highly suspected for Wilms' tumor. Since OPEN ACCESS the large size -

Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010)
DOI: 10.2478/v10163-012-0008-6 ACTA CHIRURGICA LATVIENSIS • 2011 (11) ORIGINAL ARTICLE Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010) Ivanda Franckeviča*,**, Regīna Kleina*, Ivars Melderis** *Riga Stradins University, Riga, Latvia **Children’s Clinical University Hospital, Riga, Latvia Summary Introduction. Paediatric renal tumours represent 7% of all childhood malignancies. The variable appearances of the tumours and their rarity make them especially challenging group of lesions for the paediatric pathologist. In Latvia diagnostics and treatment of childhood malignancies is concentrated in Children’s Clinical University Hospital. Microscopic evaluation of them is realised in Pathology office of this hospital. Aim of the study is to analyze morphologic spectrum of children kidney tumours in Latvia and to characterise them from modern positions with wide range of immunohistochemical markers using morphological material of Pathology bureau of Children’s Clinical University Hospital. Materials and methods. We have analyzed surgically removed primary renal tumours in Children Clinical University Hospital from the year 1997 till 2010. Samples were fixed in 10% formalin fluid, imbedded in paraffin and haematoxylin-eosin stained slides were re-examined. Immunohistochemical re-investigation was made in 65.91% of cases. For differential diagnostic purposes were used antibodies for the detection of bcl-2, CD34, EMA, actin, desmin, vimentin, CKAE1/AE3, CK7, Ki67, LCA, WT1, CD99, NSE, chromogranin, synaptophyzin, S100, myoglobin, miogenin, MyoD1 (DakoCytomation) and INI1 protein (Santa Cruz Biotechnology). Results. During the revised period there were diagnosed 44 renal tumours. Accordingly of morphological examination data neoplasms were divided: 1) nephroblastoma – 75%, 2) clear cell sarcoma – 2.27%, 3) rhabdoid tumour – 4.55%, 4) angiomyolipoma – 4.55%, 5) embrional rhabdomyosarcoma – 2.27%, 6) mesoblastic nephroma – 4.55%, 7) multicystic nephroma – 4.55%, 8) angiosarcoma – 2.27%. -

Pediatric Abdominal Masses
Pediatric Abdominal Masses Andrew Phelps MD Assistant Professor of Pediatric Radiology UCSF Benioff Children's Hospital No Disclosures Take Home Message All you need to remember are the 5 common masses that shouldn’t go to pathology: 1. Infection 2. Adrenal hemorrhage 3. Renal angiomyolipoma 4. Ovarian torsion 5. Liver hemangioma Keys to (Differential) Diagnosis 1. Location? 2. Age? 3. Cystic? OUTLINE 1. Kidney 2. Adrenal 3. Pelvis 4. Liver OUTLINE 1. Kidney 2. Adrenal 3. Pelvis 4. Liver Renal Tumor Mimic – Any Age Infection (Pyelonephritis) Don’t send to pathology! Renal Tumor Mimic – Any Age Abscess Don’t send to pathology! Peds Renal Tumors Infant: 1) mesoblastic nephroma 2) nephroblastomatosis 3) rhabdoid tumor Child: 1) Wilm's tumor 2) lymphoma 3) angiomyolipoma 4) clear cell sarcoma 5) multilocular cystic nephroma Teen: 1) renal cell carcinoma 2) renal medullary carcinoma Peds Renal Tumors Infant: 1) mesoblastic nephroma 2) nephroblastomatosis 3) rhabdoid tumor Child: 1) Wilm's tumor 2) lymphoma 3) angiomyolipoma 4) clear cell sarcoma 5) multilocular cystic nephroma Teen: 1) renal cell carcinoma 2) renal medullary carcinoma Renal Tumors - Infant 1) mesoblastic nephroma 2) nephroblastomatosis 3) rhabdoid tumor Renal Tumors - Infant 1) mesoblastic nephroma 2) nephroblastomatosis 3) rhabdoid tumor - Most common - Can’t distinguish from congenital Wilms. Renal Tumors - Infant 1) mesoblastic nephroma 2) nephroblastomatosis 3) rhabdoid tumor Look for Multiple biggest or diffuse and masses. ugliest. Renal Tumors - Infant 1) mesoblastic -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

The 2020 WHO Classification of Soft Tissue Tumours: News and Perspectives
PATHOLOGICA 2021;113:70-84; DOI: 10.32074/1591-951X-213 Review The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives Marta Sbaraglia1, Elena Bellan1, Angelo P. Dei Tos1,2 1 Department of Pathology, Azienda Ospedale Università Padova, Padova, Italy; 2 Department of Medicine, University of Padua School of Medicine, Padua, Italy Summary Mesenchymal tumours represent one of the most challenging field of diagnostic pathol- ogy and refinement of classification schemes plays a key role in improving the quality of pathologic diagnosis and, as a consequence, of therapeutic options. The recent publica- tion of the new WHO classification of Soft Tissue Tumours and Bone represents a major step toward improved standardization of diagnosis. Importantly, the 2020 WHO classi- fication has been opened to expert clinicians that have further contributed to underline the key value of pathologic diagnosis as a rationale for proper treatment. Several rel- evant advances have been introduced. In the attempt to improve the prediction of clinical behaviour of solitary fibrous tumour, a risk assessment scheme has been implemented. NTRK-rearranged soft tissue tumours are now listed as an “emerging entity” also in con- sideration of the recent therapeutic developments in terms of NTRK inhibition. This deci- sion has been source of a passionate debate regarding the definition of “tumour entity” as well as the consequences of a “pathology agnostic” approach to precision oncology. In consideration of their distinct clinicopathologic features, undifferentiated round cell sarcomas are now kept separate from Ewing sarcoma and subclassified, according to the underlying gene rearrangements, into three main subgroups (CIC, BCLR and not Received: October 14, 2020 ETS fused sarcomas) Importantly, In order to avoid potential confusion, tumour entities Accepted: October 19, 2020 such as gastrointestinal stroma tumours are addressed homogenously across the dif- Published online: November 3, 2020 ferent WHO fascicles. -

Angioleiomyoma of the Sinonasal Tract: Analysis of 16 Cases and Review of the Literature
Head and Neck Pathol (2015) 9:463–473 DOI 10.1007/s12105-015-0636-y ORIGINAL PAPER Angioleiomyoma of the Sinonasal Tract: Analysis of 16 Cases and Review of the Literature 1 2 3 2 Abbas Agaimy • Michael Michal • Lester D. R. Thompson • Michal Michal Received: 7 April 2015 / Accepted: 30 May 2015 / Published online: 6 June 2015 Ó Springer Science+Business Media New York 2015 Abstract Angioleiomyoma (ALM; synonyms: angiomy- The covering mucosa was ulcerated in 6 cases and showed oma, vascular leiomyoma) is an uncommon benign tumor squamous metaplasia in one case. There were no recur- of skin and subcutaneous tissue. Most arise in the rences after local excision. Submucosal sinonasal ALMs extremities (90 %). Head and neck ALMs are uncommon are rare benign tumors similar to their reported cutaneous (*10 % of all ALMs) and those arising beneath the counterparts with frequent adipocytic differentiation. They sinonasal tract mucosa are very rare (\1 %) with 38 cases should be distinguished from renal-type angiomyolipoma. reported so far. We herein analyzed 16 cases identified Simple excision is curative. from our routine and consultation files. Patients included seven females and nine males aged 25–82 years (mean 58; Keywords Angioleiomyoma Á Sinonasal tract Á median 62). Symptoms were intermittent nasal obstruction, Angiomyolipoma Á Vascular leiomyoma Á Angiomyoma Á sinusitis, recurrent epistaxis, and a slow-growing mass. PEComa Á Nasal Fifteen lesions originated within different regions of the nasal cavity and one lesion was detected incidentally in an ethmoid sinus sample. Size range was 6–25 mm (mean 11). Introduction Histologically, all lesions were well circumscribed but non- encapsulated and most (12/16) were of the compact solid Mesenchymal tumors of the sinonasal tract are rare. -

Review of Myofibroblastoma of Breast and Its Most Common Mimickers
38 Jan 2012 Vol 5 No.1 North American Journal of Medicine and Science Review Review of Myofibroblastoma of Breast and Its Most Common Mimickers Ying Huang, MD, PhD; Frank Chen, MD, PhD Department of Pathology, Buffalo General Hospital, State University of New York, Buffalo, NY Myofibroblastoma (MFB) is characterized as a benign stromal neoplasm composed of uniform, bland- looking spindle cells that are often arranged in fascicles separated by thick band of collagenous stroma. Variable cellularity is common. Immunohistochemically, the spindle cells are positive for CD34, vimentin, BCL-2, ER, PR, focally positive for smooth muscle actin and negative for cytokeratin, S-100 and CD117. Although classic MFB is typically a bland-looking spindle cell tumor, some unusual morphologic variants may show worrisome malignant-looking cells. Recognition of MFB variants and its wide variety of mimickers is very important for pathologists to arrive at the correct diagnosis, and avoid misdiagnosis of malignancy. [N A J Med Sci. 2012;5(1):38-42.] Key Words: breast, myofibroblastoma, solitary fibrous tumor, spindle cell lipoma, metaplastic spindle cell carcinoma, myofibroblastic sarcoma, Phyllodes tumor INTRODUCTION Myofibroblastoma of breast (MFB) is a rare benign spindle homogeneously solid mass devoid of microcalcifications.4 cell tumor of mammary stroma composed of myofibroblasts. Grossly, MFB reveals a well circumscribed nodule or a This entity was first described in 1981 by Toker et al. as a multiloculated mass, with most measuring less than 4 cm in benign spindle cell tumor.1 The term “myofibroblastoma” diameter (2.3 cm on average, ranging from 1 to 4 cm).16 In was established by Wargotz et al in 1987.2 The original rare cases, it can be large (> 10 cm).17 The cut section report demonstrated that MFB had a male predominance.2 reveals a homogeneous, buldging pink to gray whirled However, later studies illustrated that it can occur in both surface.