Spreading Ideas: the Integrated District Evidence-To-Action Program to Improve Maternal, Newborn and Child Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mozambique, [email protected]
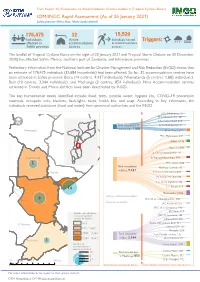
Flash Report 15 | Evacuations to Accommodation Centres Update 2 (Tropical Cyclone Eloise) IOM/INGC Rapid Assessment (As of 25 January 2021) Sofala province (Beira, Buzi, Nhamatanda district) 176,475 32 15,520 Individuals Active Individuals hosted Triggers: in accommodations aected in accommodation Sofala province centres centres The landfall of Tropical Cyclone Eloise on the night of 23 January 2021 and Tropical Storm Chalane on 30 December 2020) has aected Sofala, Manica, southern part of Zambezia, and Inhambane provinces. Preliminary information from the National Institute for Disaster Management and Risk Reduction (INGD) shows that an estimate of 176,475 individuals (35,684 households) had been aected. So far, 32 accommodation centres have been activated in Sofala province: Beira (14 centres, 9,437 individuals), Nhamatanda (5 centres, 1,885 individuals), Buzi (10 centres, 3,344 individuals), and Machanga (3 centres, 854 individuals). Nine Accommodation centres activated in Dondo and Muasa districts have been deactivated by INGD. The top humanitarian needs identied include: food, tents, potable water, hygiene kits, COVID-19 prevention materials, mosquito nets, blankets, ash-lights, tarps, health kits, and soap. According to key informants, the individuals received assistance (food and water) from provincial authorities and the INGD. EPC- Nhampoca: 27 Maringue EPC Nhamphama: 107 EPC Felipe Nyusi: 418 Total evacuations in EPC Nhatiquiriqui: 74 Cheringoma Nhamatanda: Gorongosa 1,885 ES de Tica: 1,259 EPC- Matadouro: 493 IFAPA: 1,138 Muavi 1: 1,011 Muanza E. Comunitaria SEMO: 170 Nhamatanda E. Especial Macurungo: 990 5 EPC- Chota: 600 Total evacuations Munhava Central: 315 in Beira: 9,437 Dondo E S Sansao Mutemba: 428 ES Samora Machel: 814 E. -

Manica Tambara Sofala Marromeu Mutarara Manica Cheringoma Sofala Ndoro Chemba Maringue
MOZAMBIQUE: TROPICAL CYCLONE IDAI AND FLOODS MULTI-SECTORAL LOCATION ASSESSMENT - ROUND 14 Data collection period 22 - 25 July 2020 73 sites* 19,628 households 94,220 individuals 17,005 by Cyclone Idai 82,151 by Cyclone Idai 2,623 by floods 12,069 by floods From 22 to 25 July 2020, in close coordination with Mozambique’s National Institute for Disaster Management (INGC), IOM’s Displacement Tracking Matrix (DTM) teams conducted multi-sectoral location assessments (MSLA) in resettlement sites in the four provinces affected by Cyclone Idai (March 2019) and the floods (between December 2019 and February 2020). The DTM teams interviewed key informants capturing population estimates, mobility patterns, and multi-sectoral needs and vulnerabilities. Chemba Tete Nkganzo Matundo - unidade Chimbonde Niassa Mutarara Morrumbala Tchetcha 2 Magagade Marara Moatize Cidade de Tete Tchetcha 1 Nhacuecha Tete Tete Changara Mopeia Zambezia Sofala Caia Doa Maringue Guro Panducani Manica Tambara Sofala Marromeu Mutarara Manica Cheringoma Sofala Ndoro Chemba Maringue Gorongosa Gorongosa Mocubela Metuchira Mocuba Landinho Muanza Mussaia Ndedja_1 Sofala Maganja da Costa Nhamatanda Savane Zambezia Brigodo Inhambane Gogodane Mucoa Ronda Digudiua Parreirão Gaza Mutua Namitangurini Namacurra Munguissa 7 Abril - Cura Dondo Nicoadala Mandruzi Maputo Buzi Cidade da Beira Mopeia Maquival Maputo City Grudja (4 de Outubro/Nhabziconja) Macarate Maxiquiri alto/Maxiquiri 1 Sussundenga Maxiquiri 2 Chicuaxa Buzi Mussocosa Geromi Sofala Chibabava Maximedje Muconja Inhajou 2019 -

World Bank Documents
Document of The World Bank Public Disclosure Authorized Report No.: 84667-MZ Public Disclosure Authorized PROJECT PERFORMANCE ASSESSMENT REPORT THE REPUBLIC OF MOZAMBIQUE DECENTRALIZED PLANNING AND FINANCE PROJECT (IDA-HO670-MOZ) February 18, 2014 Public Disclosure Authorized IEG Public Sector Evaluation Independent Evaluation Group Public Disclosure Authorized ii Currency Equivalents (annual averages) Currency Unit = Mozambican metical (MZM) 2004 US$1.00 MZN 22,144.71 2005 US$1.00 MZN 22,850.81 2006 US$1.00 MZN 25,758.32 (January to July) 2006 US$1.00 MZN 25.89 (July to December) 2007 US$1.00 MZN 25.79 2008 US$1.00 MZN 24.19 2009 US$1.00 MZN 27.58 2010 US$1.00 MZN 34.24 Abbreviations and Acronyms CCAGG Concerned Citizens of Abra for Good Government CPIA Country Program and Institutional Assessments DGA Development Grant Agreement DPFP Decentralized Planning and Finance Project FCA Fundo de Compensação Autárquica FIL Fundo de Iniciativa Local FRELIMO Frente de Libertação de Moçambique GTZ German Technical Cooperation ICR Implementation Completion Report IDA International Development Association IEG Independent Evaluation Group IEGPS IEG Public Sector Evaluation M&E Monitoring and Evaluation MOPH Ministry of Public Works and Housing MOZ Mozambique NDPFP National Decentralized Planning and Finance Project PAD Project Appraisal document PARPA Action Plan for Reduction of Absolute Poverty PEDD Plano Estratégico de Desenvolvimento Distrital PEFA Public Expenditure and Financial Accountability PESOD Plano Económico Social e Orçamento Distrital PPAR Project Performance Assessment Report PRSCs Poverty Reduction Strategy Credits PSRP Public Sector Reform Project UNCDF United Nations Capital Development Fund UNDP United Nations Development Program UNICEF United Nations Children's Fund Fiscal Year Government: January I - December 31 Acting Director-General, Independent Evaluation Mr. -

World Bank Document
Report No. 47876-MZ Mozambique Municipal Development in Mozambique Lessons from the First Decade Public Disclosure AuthorizedPublic Disclosure Authorized (In Two Volumes) Volume II : Full Report May 2009 Urban and Water, AFTUW Country Department, AFCS2 Africa Region Public Disclosure AuthorizedPublic Disclosure Authorized Public Disclosure AuthorizedPublic Disclosure Authorized Document of the World Bank Public Disclosure AuthorizedPublic Disclosure Authorized Table of Contents Acronyms ……………………………………………………………………………….7 Executive Summary .........................................................................................................12 Chapter 1 An Introduction to Urbanization and Municipal Development in Mozambique .................................................................................................22 1.1 Objective ........................................................................................................22 1.2 “Urban” and “Municipal” in Mozambique ....................................................22 1.3 A Brief Socio-Economic Profile of Municipalities in Mozambique .............26 1.4 Rationale and Key Questions of the Study ....................................................28 1.5 Structure of the Study ....................................................................................30 1.6 Outline of the Study .......................................................................................32 Annex 1.2 Population by Municipality in Mozambique. 1997 and 2007 estimates ...........39 Chapter -

The Mozambican National Resistance (Renamo) As Described by Ex-Patticipants
The Mozambican National Resistance (Renamo) as Described by Ex-patticipants Research Report Submitted to: Ford Foundation and Swedish International Development Agency William Minter, Ph.D. Visiting Researcher African Studies Program Georgetown University Washington, DC March, 1989 Copyright Q 1989 by William Minter Permission to reprint, excerpt or translate this report will be granted provided that credit is given rind a copy sent to the author. For more information contact: William Minter 1839 Newton St. NW Washington, DC 20010 U.S.A. INTRODUCTION the top levels of the ruling Frelirno Party, local party and government officials helped locate amnestied ex-participants For over a decade the Mozambican National Resistance and gave access to prisoners. Selection was on the basis of the (Renamo, or MNR) has been the principal agent of a desuuctive criteria the author presented: those who had spent more time as war against independent Mozambique. The origin of the group Renamo soldiers. including commanders, people with some as a creation of the Rhodesian government in the mid-1970s is education if possible, adults rather than children. In a number of well-documented, as is the transfer of sponsorship to the South cases, the author asked for specific individuals by name, previ- African government after white Rhodesia gave way to inde- ously identified from the Mozambican press or other sources. In pendent Zimbabwe in 1980. no case were any of these refused, although a couple were not The results of the war have attracted increasing attention geographically accessible. from the international community in recent years. In April 1988 Each interview was carried out individually, out of hearing the report written by consultant Robert Gersony for the U. -

Southern Africa Tropical Cyclone Idai Fact Sheet #5
SOUTHERN AFRICA – TROPICAL CYCLONE IDAI FACT SHEET #5, FISCAL YEAR (FY) 2019 APRIL 5, 2019 NUMBERS AT HIGHLIGHTS HUMANITARIAN FUNDING A GLANCE FOR THE SOUTHERN AFRICA CYCLONE & Health agencies reach 32,000 people during FLOODS RESPONSE IN FY 2019 cholera vaccination campaign in one day USAID/OFDA1 $4,569,083 598 USAID food and nutrition commodities begin to arrive in Mozambique Official Confirmed Deaths USAID/FFP2 $35,658,852 in Mozambique UN releases revised flash appeal for GoM – April 2019 Zimbabwe, requesting $60 million to respond DoD3 $3,192,488 to Tropical Cyclone Idai 299 USAID staff assess damages and humanitarian $43,420,423 Number of Deaths in needs generated by cyclone-related flooding in Zimbabwe Malawi OCHA – April 2019 KEY DEVELOPMENTS 1.85 As of April 5, the official number of confirmed deaths in Mozambique remained constant at 598 and the number of injuries remained unchanged at more than 1,600, according to million the Government of the Republic of Mozambique (GRM). The GRM reports that Estimated Number of approximately 129,800 people were sheltering in 129 accommodation sites in Manica, People in Need of Sofala, Tete, and Zambézia provinces as of April 5. In addition, the number of homes Assistance in Mozambique damaged or destroyed by the cyclone has increased to more than 216,700, according to UN – March 2019 the GRM. The GRM Ministry of Health (MoH) had reported nearly 2,100 cholera cases, including two deaths, in Sofala’s Beira and Dondo towns and Buzi District as of April 5, according 129,800 to the UN. -

Projectos De Energias Renováveis Recursos Hídrico E Solar
FUNDO DE ENERGIA Energia para todos para Energia CARTEIRA DE PROJECTOS DE ENERGIAS RENOVÁVEIS RECURSOS HÍDRICO E SOLAR RENEWABLE ENERGY PROJECTS PORTFÓLIO HYDRO AND SOLAR RESOURCES Edition nd 2 2ª Edição July 2019 Julho de 2019 DO POVO DOS ESTADOS UNIDOS NM ISO 9001:2008 FUNDO DE ENERGIA CARTEIRA DE PROJECTOS DE ENERGIAS RENOVÁVEIS RECURSOS HÍDRICO E SOLAR RENEWABLE ENERGY PROJECTS PORTFOLIO HYDRO AND SOLAR RESOURCES FICHA TÉCNICA COLOPHON Título Title Carteira de Projectos de Energias Renováveis - Recurso Renewable Energy Projects Portfolio - Hydro and Solar Hídrico e Solar Resources Redação Drafting Divisão de Estudos e Planificação Studies and Planning Division Coordenação Coordination Edson Uamusse Edson Uamusse Revisão Revision Filipe Mondlane Filipe Mondlane Impressão Printing Leima Impressões Originais, Lda Leima Impressões Originais, Lda Tiragem Print run 300 Exemplares 300 Copies Propriedade Property FUNAE – Fundo de Energia FUNAE – Energy Fund Publicação Publication 2ª Edição 2nd Edition Julho de 2019 July 2019 CARTEIRA DE PROJECTOS DE RENEWABLE ENERGY ENERGIAS RENOVÁVEIS PROJECTS PORTFOLIO RECURSOS HÍDRICO E SOLAR HYDRO AND SOLAR RESOURCES PREFÁCIO PREFACE O acesso universal a energia em 2030 será uma realidade no País, Universal access to energy by 2030 will be reality in this country, mercê do “Programa Nacional de Energia para Todos” lançado por thanks to the “National Energy for All Program” launched by Sua Excia Filipe Jacinto Nyusi, Presidente da República de Moçam- His Excellency Filipe Jacinto Nyusi, President of the -
Environmental and Social Management Framework (Esmf)
REPUBLIC OF MOZAMBIQUE MINISTRY OF EDUCATION AND HUMAN DEVELOPMENT (MINEDH) IMPROVING LEARNING AND EMPOWERING GIRLS IN MOZAMBIQUE (P172657) ENVIRONMENTAL AND SOCIAL MANAGEMENT FRAMEWORK (ESMF) February, 2021 TABLE OF CONTENTS LIST OF ABBREVIATIONS ............................................................................................................ 1 LIST OF TABLES AND FIGURES .................................................................................................. 2 EXECUTIVE SUMMARY ................................................................................................................ 4 SUMARIO EXECUTIVO ................................................................................................................. 8 1. INTRODUCTION ................................................................................................................. 133 1.1. Overview ......................................................................................................................... 13 1.2. Scope and Objectives of the ESMF................................................................................... 15 1.3. Methodology Used to Develop ESMF .............................................................................. 15 2 PROJECT DESCRIPTION AND INSTITUTIONAL ARRANGEMENTS .............................. 17 2.1 The Project Area (Geographical Areas Covered) ............................................................ 177 2.2 Project Development Objective (PDO) ............................................................................ -

Manica Province
Back to National Overview OVERVIEW FOR MANICA PROVINCE Tanzania Zaire Comoros Malawi Cabo Del g ad o Niassa Zambia Nampul a Tet e Manica Zambezi a Manica Zimbabwe So f al a Madagascar Botswana Gaza Inhambane South Africa Maput o N Swaziland 200 0 200 400 Kilometers Overview for Manica Province 2 The term “village” as used herein has the same meaning as “the term “community” used elsewhere. Schematic of process. MANICA PROVINCE 678 Total Villages C P EXPERT OPINION o m l COLLECTION a n p n o i n n e g TARGET SAMPLE n t 136 Villages VISITED INACCESSIBLE 121 Villages 21 Villages LANDMINE- UNAFFECTED BY AFFECTED NO INTERVIEW LANDMINES 60 Villages 3 Villages 58 Villages 110 Suspected Mined Areas DATA ENTERED INTO D a IMSMA DATABASE t a E C n o t r m y p a MINE IMPACT SCORE (SAC/UNMAS) o n n d e A n t n a HIGH IMPACT MODERATE LOW IMPACT l y 2 Villages IMPACT 45 Villages s i s 13 Villages FIGURE 1. The Mozambique Landmine Impact Survey (MLIS) visited 9 of 10 Districts in Manica. Cidade de Chimoio was not visited, as it is considered by Mozambican authorities not to be landmine-affected. Of the 121 villages visited, 60 identified themselves as landmine-affected, reporting 110 Suspected Mined Areas (SMAs). Twenty-one villages were inaccessible, and three villages could not be found or were unknown to local people. Figure 1 provides an overview of the survey process: village selection; data collection; and data-entry into the Information Management System for Mine Action (IMSMA) database, out of which is generated the Mine Impact Score (Appendix I). -

MULTI-SECTORAL RAPID NEEDS ASSESSMENT POST-CYCLONE ELOISE Sofala and Manica Provinces, Mozambique Page 0 of 23
MRNA - Cyclone Eloise Miquejo community in Beira after Cyclone Eloise, Photo by Dilma de Faria MULTI-SECTORAL RAPID NEEDS ASSESSMENT POST-CYCLONE ELOISE Sofala and Manica Provinces, Mozambique Page 0 of 23 27 January – 5 February 2021 MRNA - Cyclone Eloise Contents ACKNOWLEDGEMENTS ............................................................................................................................. 2 Executive Summary Cyclone Eloise ............................................................................................................. 2 Key Findings ............................................................................................................................................. 3 Multi-Sectoral Recommendations ............................................................................................................. 3 OVERVIEW ................................................................................................................................................... 5 METHODOLOGY & DATA COLLECTION .................................................................................................... 6 LIMITATIONS ............................................................................................................................................ 7 Geographical Coverage ........................................................................................................................ 7 Generalizability ..................................................................................................................................... -

Bds Needs Assessment in Nacala and Beira Corridor
USAID AgriFUTURO Mozambique Agribusiness and Trade Competitiveness Program Business Development Services Needs Assessment FINAL REPORT June 2010 By: Carlos Fumo (Senior Expert) TABLE OF CONTENTS 0. Note of Thanks .............................................................................................. 3 1. Acronyms and abbreviations.......................................................................... 4 2. General introduction ...................................................................................... 6 2.1. Background and introduction ................................................................. 6 3. Overall objectives of the Assessment ............................................................ 7 4. Deliverables ................................................................................................... 8 5. Methodology .................................................................................................. 8 5.1. Secondary Research .................................................................................. 9 5.2. Primary Research ................................................................................... 9 5.3. Data analysis and report writing ........................................................... 11 5.4. Sampling ............................................................................................... 11 6. The needs assessment process .................................................................. 13 7. The limitations of the study ......................................................................... -

Drinking Water Supply and Sanitation Interventions in Rural Mozambique
Report | no. 360 Report | no. Impact evaluation of drinking water supply and sanitation interventions in rural Mozambique Since 2006, the UNICEF–Netherlands Partnership evaluation office. It found evidence of a large Programme for Water Supply and Sanitation has increase in the use of improved water sources been supporting Water Supply and Sanitation and in the ownership and use of latrines. Much of programmes in Mozambique. The largest the increase can be attributed to an innovative programme, the ‘One Million Initiative’ aims to approach to sanitation. However, water from bring improved sanitation and clean water to improved sources and even more importantly, over one million people in rural Mozambique. stored water, are not always safe to drink. An Half-way through the programme, a joint impact element of subsidy will continue to be needed to evaluation was carried out by IOB and UNICEF’s sustain facilities and services. More than Water Published by: Ministry of Foreign Affairs Impact evaluation of drinking water supply and sanitation interventions in rural Mozambique Policy and Operations Evaluation Department (IOB) P.O. box 20061 | 2500 eb The Hague | The Netherlands www.minbuza.nl/iob © Ministry of Foreign Affairs | October 2011| ISBN 978-90-5328-414-8 11Buz283729 | E This project was a product of a cooperation between: Impact evaluation of drinking water supply and sanitation interventions in rural Mozambique More than Water Mid-term impact evaluation: UNICEF – Government of The Netherlands Partnership for Water Supply, Sanitation and Hygiene ‘One Million Initiative’, Mozambique Impact evaluation of drinking water supply and sanitation interventions in rural Mozambique Preface Drinking water supply and basic sanitation has been a priority for the Netherlands’ development co-operation and for UNICEF for many years.