Medication Therapy Management in Pharmacy Practice Core Elements of an MTM Service Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
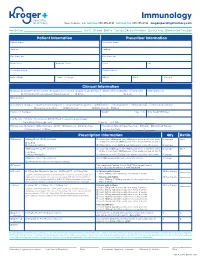
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®) Policy Number: 2021D0088F Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Rationale ....................................................................... 1 • Intravenous Iron Replacement Therapy (Feraheme®, Definitions ...................................................................................... 3 Injectafer®, & Monoferric®) Applicable Codes .......................................................................... 3 Background.................................................................................... 4 Benefit Considerations .................................................................. 4 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 7 Centers for Medicare and Medicaid Services ............................. 8 References ..................................................................................... 8 Policy History/Revision Information ............................................. 9 Instructions for Use ....................................................................... 9 Coverage Rationale See Benefit Considerations This policy refers to the following intravenous iron replacements: Feraheme® (ferumoxytol) Injectafer® (ferric carboxymaltose) Monoferric® (ferric derisomaltose)* The following -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Pharmacy/Medical Drug Prior Authorization Form
High Cost Medical Drugs List High Cost Medical Drugs administered by Health Alliance™ providers within physician offices, infusion centers or hospital outpatient settings must be acquired from preferred specialty vendors. Health Alliance will not reimburse any drug listed as a “High Cost Medical Drug,” whether obtained from the provider’s own stock or via “buy-and-bill.” This drug list does not apply to members with Medicare coverage. Information on how to acquire these medications is located at the end of this document. Recent Updates Preferred Contact Drug Therapy Drug Name Code PA Effective Change Vendor Number Oncology – Injectable DARZALEX FASPRO J9144 YES 10/1/2021 CVS/Caremark® 800-237-2767 Added High Cost Medical Drug List Preferred Contact Drug Therapy Drug Name Code PA Effective Vendor Number Acromegaly SANDOSTATIN J2353 YES 7/1/2020 CVS/Caremark® 800-237-2767 Acromegaly SOMATULINE J1930 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products JETREA J7316 YES 7/1/2020 LDD Additional Products PROLASTIN J0256 YES 7/1/2020 LDD Additional Products QUTENZA J7336 NO 7/1/2020 LDD Additional Products REVCOVI J3590 YES 7/1/2020 LDD Additional Products RADICAVA J1301 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products SIGNIFOR J2502 YES 7/1/2020 Accredo® 866-759-1557 Additional Products SPRAVATO J3490 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products STRENSIQ J3590 YES 7/1/2020 LDD Additional Products THIOTEPA J9340 YES 7/1/2020 CVS/Caremark® 800-237-2767 Allergic Asthma CINQAIR J2786 YES 7/1/2020 CVS/Caremark® 800-237-2767 -

Mir-205: a Potential Biomedicine for Cancer Therapy
cells Review miR-205: A Potential Biomedicine for Cancer Therapy Neeraj Chauhan 1,2 , Anupam Dhasmana 1,2, Meena Jaggi 1,2, Subhash C. Chauhan 1,2 and Murali M. Yallapu 1,2,* 1 Department of Immunology and Microbiology, School of Medicine, University of Texas Rio Grande Valley, McAllen, TX 78504, USA; [email protected] (N.C.); [email protected] (A.D.); [email protected] (M.J.); [email protected] (S.C.C.) 2 South Texas Center of Excellence in Cancer Research, School of Medicine, University of Texas Rio Grande Valley, McAllen, TX 78504, USA * Correspondence: [email protected]; Tel.: +1-(956)-296-1734 Received: 3 June 2020; Accepted: 21 August 2020; Published: 25 August 2020 Abstract: microRNAs (miRNAs) are a class of small non-coding RNAs that regulate the expression of their target mRNAs post transcriptionally. miRNAs are known to regulate not just a gene but the whole gene network (signaling pathways). Accumulating evidence(s) suggests that miRNAs can work either as oncogenes or tumor suppressors, but some miRNAs have a dual nature since they can act as both. miRNA 205 (miR-205) is one such highly conserved miRNA that can act as both, oncomiRNA and tumor suppressor. However, most reports confirm its emerging role as a tumor suppressor in many cancers. This review focuses on the downregulated expression of miR-205 and discusses its dysregulation in breast, prostate, skin, liver, gliomas, pancreatic, colorectal and renal cancers. This review also confers its role in tumor initiation, progression, cell proliferation, epithelial to mesenchymal transition, and tumor metastasis. -

Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals
Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals The Board of Registration in Allied Health evaluates the qualifications of applicants for licensure and grants licenses to those who qualify. It establishes rules and regulations to ensure the integrity and competence of licensees. The Board is the link between the consumer and the allied health professional and, as such, promotes the public health, welfare and safety. Allied health professionals are occupational therapists and assistants, athletic trainers, and physical therapists and assistants. Occupational Therapists/Occupational Therapist Assistants Occupational therapists are health professionals who use occupational activities with specific goals in helping people of all ages to prevent, lessen or overcome physical, psychological or developmental disabilities. Occupational Therapists and Occupational Therapist Assistants help people with physical, psychological, or developmental problems regain abilities or adjust to handicaps. They work with physicians, physical and speech therapists, nurses, social workers, psychologists, teachers and other specialists. Patients may face handicaps, injuries, illness, psychological or social problems, or barriers due to age, economic, and cultural factors. Occupational Therapists: Consult with treatment teams to develop individualized treatment programs. Select and teach activities based on the needs and capabilities of each patient Evaluate each patient's progress, attitude and behavior. Design special equipment to aid patients with disabilities. Teach patients how to adjust to home, work, and social environments. Test and evaluate patients' physical and mental abilities. Educate others about occupational therapy. The goal of occupational therapy (OT) is for persons to achieve the highest level of independence after an injury or illness. OT addresses the whole person - cognitive, physical and emotional status. -

Current Status of Immunology Education in US Schools And
American Journal of Pharmaceutical Education 2019; 83 (7) Article 6994. RESEARCH Current Status of Immunology Education in US Schools and Colleges of Pharmacy Yuan Zhao, PhD,a Dana Ho, PharmD,a Benjamin Oldham, PharmD,a Bonnie Dong, PharmD,a Daniel Malcom, PharmDa,b a Sullivan University College of Pharmacy, Louisville, Kentucky b Associate Editor, American Journal of Pharmaceutical Education, Arlington, Virginia Submitted February 2, 2018; accepted June 17, 2018; published September 2019. Objective. To determine the extent of immunology education in US Doctor of Pharmacy (PharmD) programs. Methods. Curricular information on immunology education was collected from the web pages of US PharmD programs (N5142). The data were sorted, comparisons were made, and trends were identified. Results. Of 142 PharmD programs studied, 100% posted curriculum information on their websites. Among them, 73 programs (51.4%) had a dedicated immunology course in their curriculum, either as an independent course or a course combined with another subject. Most immunology education was offered in the first professional year (72.5%). Of the programs that offered immunology as an in- dependent course, the number of semester hours dedicated to the course varied from 1.5 to 3.5 (median53, mode53, mean52.7). More three-year programs offered immunology as a core compo- nent in the didactic curriculum than did four-year programs (64.7% vs 49.6%). Similarly, more private programs offered immunology than did public programs (64% vs 37.3%). Conclusion. Immunology education in US schools and colleges of pharmacy lacks consensus. Not all PharmD programs indicated they offered specific, focused immunology education in their curricula. -

Telepharmacy Rules and Statutes: a 50-State Survey
American Journal of Medical Research 5(2), 2018 pp. 7–23, ISSN 2334-4814, eISSN 2376-4481 doi:10.22381/AJMR5220181 TELEPHARMACY RULES AND STATUTES: A 50-STATE SURVEY GEORGE TZANETAKOS Department of Health Management and Policy, College of Public Health, The University of Iowa FRED ULLRICH Department of Health Management and Policy, College of Public Health, The University of Iowa KEITH MUELLER [email protected] Department of Health Management and Policy, College of Public Health, The University of Iowa (corresponding author) ABSTRACT. There has been a significant decline in the number of independently owned rural pharmacies serving non-metropolitan areas, thereby limiting access to pharmaceutical services for rural residents, particularly for those most vulnerable and in need of these services. The use of telepharmacy is one potential solution to this problem. Telepharmacies deliver pharmaceutical care to outpatients at a distance via telecommunication and other advanced technologies. This study identifies rules and laws enacted by states authorizing the use of community telepharmacy initiatives within their respective jurisdictions. As of August 2016, the use of telepharmacy was authorized, in varying capacities, in 23 states (46%). Pilot program development that could apply to telepharmacy initiatives was authorized by six states (12%). Waivers to administrative or legislative pharmacy practice requirements that could allow for telepharmacy initiatives were permitted in five states (10%). Nearly one-third of the states (16, or 32%) did not authorize the use of telepharmacy, nor did they authorize the pursuit of telepharmacy initiatives via pilot programs or waivers. Keywords: telepharmacy; rule; statute; rural; community; outpatient How to cite: Tzanetakos, George, Fred Ullrich, and Keith Mueller (2018). -

Health Science: Biomedicine Public Service Endorsement
INNOVATE • COLLABORATE • EDUCATE • INNOVATE • COLLABORATE • EDUCATE Health Science: Biomedicine Public Service Endorsement Career Pathways • Biochemist • Biomedical Engineer • Biophysicist • Physician, Surgeon Certifications / Certificate Options • CPR • OSHA Program Highlights Biomedical engineering represents new areas of medical research and • Pathogen Analysis product development; biomedical engineers’ work helps pave the way • Human Anatomy & Physiology for new ways to help treat injuries and diseases. As medicine is a field • DNA / Genomics with vast numbers of specific disciplines, there are many different sub- • Laboratory Procedures fields in which biomedical engineers work. Some work to improve and • Dissection develop new machinery, such as robotic surgery equipment; others • Grow and Culture Bacteria endeavor to create better, more reliable replacement limbs (or parts • Real World Research which help existing limbs function better, such as joint replacements). • Learn to Treat Patients New and more comfortable patient beds, monitoring equipment, and electronics are also products that often begin as concepts from the CTSO(s) biomedical engineer’s or involve some level of input from them. • HOSA - Future Health Professionals KISD Biomedical Program: Program Fees / Requirements Biomedicine classes in KISD aim to prepare students to enter the • HOSA membership (Optional) health care field by giving them a foundation in real world problems, medical treatments, and a better understanding of the human body. Program Location Students will investigate causes and treatments of diseases that R Course(s) available at CHS affect the entire world as well as ones found in our own community. R Course(s) available at FRHS Students learn advanced techniques used in hospitals and research R Course(s) available at KHS labs and will become familiar with protocols used by doctors and R Course(s) available at TCHS researchers today. -

Massage Therapy Admission Packet
Caldwell Community College and Technical Institute Welcome to Caldwell Community College and Technical Institute. In this packet, you will find information about our Massage Therapy Program including costs, requirements, and details on how to prepare for your new career. Caldwell Campus 2855 Hickory Blvd Hudson, NC 28638 828.726.2200 Watauga Campus 372 Community College Drive Boone, NC 28607 828.297.8120 Amy Swink Massage Therapy Program Coordinator Watauga Campus E-mail: [email protected] Phone: (828)726-2242 and (828) 297-3811 MASSAGE THERAPY COURSE HEA 3021 This course is designed to prepare the student for the certification examination required for the North Carolina licensure application process. Through class work and practical “hands-on” training, students obtain a solid foundation for professional practice as a Massage Therapist. Upon successful completion of the course, the student is eligible to sit for the state exam and apply for state licensure in North Carolina. Competitive Admissions: Students, who successfully complete Massage Therapy training at CCC&TI, will receive two (2) points toward admission into the Physical Therapy Assistant program at CCC&TI Educational Pathway Example: Massage Therapy training > Licensure by examination > Licensed Massage and Bodywork Therapist Estimated Hourly Earnings: According to the Bureau of Labor Statistics website ( www.bls.gov/oes/current/oes319011.htm), current mean annual wage is $44,950. Employment Opportunities: • Chiropractic offices • Home care agencies • Hospice • Hospitals • Medical offices • Retirement homes • Self-employment • Spas FAQs • Is massage therapy training required to become licensed in North Carolina? o Yes. The North Carolina Board of Massage and Bodywork Therapy (NCBMBT) requires an applicant to successfully complete a state approved training program consisting of a minimum 500 in-class training hours. -

Staphylococcus Aureus Bloodstream Infection Treatment Guideline
Staphylococcus aureus Bloodstream Infection Treatment Guideline Purpose: To provide a framework for the evaluation and management patients with Methicillin- Susceptible (MSSA) and Methicillin-Resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI). The recommendations below are guidelines for care and are not meant to replace clinical judgment. The initial page includes a brief version of the guidance followed by a more detailed discussion of the recommendations with supporting evidence. Also included is an algorithm describing management of patients with blood cultures positive for gram-positive cocci. Brief Key Points: 1. Don’t ignore it – Staphylococcus aureus isolated from a blood culture is never a contaminant. All patients with S. aureus in their blood should be treated with appropriate antibiotics and evaluated for a source of infection. 2. Control the source a. Removing infected catheters and prosthetic devices – Retention of infected central venous catheters and prosthetic devices in the setting of S. aureus bacteremia (SAB) has been associated with prolonged bacteremia, treatment failure and death. These should be removed if medically possible. i. Retention of prosthetic material is associated with an increased likelihood of SAB relapse and removal should be considered even if not clearly infected b. Evaluate for metastatic infections (endocarditis, osteomyelitis, abscesses, etc.) – Metastatic infections and endocarditis are quite common in SAB (11-31% patients with SAB have endocarditis). i. All patients should have a thorough history taken and exam performed with any new complaint evaluated for possible metastatic infection. ii. Echocardiograms should be strongly considered for all patients with SAB iii. All patients with a prosthetic valve, pacemaker/ICD present, or persistent bacteremia (follow up blood cultures positive) should undergo a transesophageal echocardiogram 3.