Telepharmacy Rules and Statutes: a 50-State Survey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
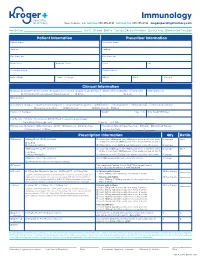
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

World Journal of Advanced Research and Reviews
World Journal of Advanced Research and Reviews, 2020, 07(02), 218–226 World Journal of Advanced Research and Reviews e-ISSN: 2581-9615, Cross Ref DOI: 10.30574/wjarr Journal homepage: https://www.wjarr.com (RESEARCH ARTICLE) Implementation and evaluation of telepharmacy during COVID-19 pandemic in an academic medical city in the Kingdom of Saudi Arabia: paving the way for telepharmacy Abdulsalam Ali Asseri *, Mohab Mohamed Manna, Iqbal Mohamed Yasin, Mashael Mohamed Moustafa, Fatmah Mousa Roubie, Salma Moustafa El-Anssasy, Samer Khalaf Baqawie and Mohamed Ahmed Alsaeed Associate Professor Imam Abdulrahman Bin Faisal University; Director of Pharmacy services at King Fahad University Hospital, KSA. Publication history: Received on 07 July 2020; revised on 22 August 2020; accepted on 25 August 2020 Article DOI: https://doi.org/10.30574/wjarr.2020.7.2.0250 Abstract King Fahad University Hospital, a leading public healthcare institution in the Eastern region of KSA, implemented a disruptive innovation of Telepharmacy in pursuit of compliance with the National COVID-19 Response Framework. It emerged and proved to be an essential and critical pillar in suppression and mitigation strategies. Telepharmacy innovation resulted in Pharmacy staffing protection and provided uninterrupted access and care continuum to the pharmaceutical services, both for COVID-19 and Collateral care. This reform-oriented initiative culminated in adopting engineering and administrative controls to design the workflows, practices, and interactions between healthcare providers, patients, and pharmaceutical frontline staff. Pharmaceutical services enhanced its surge capacity (14,618 OPD requests & 10,030 Inpatient orders) and improved capability (41,242 counseling sessions) to address the daunting challenge of complying with the inpatient needs and robust outpatient pharmaceutical consumer services. -

Clinical Pharmacy Specialist
SAMPLE JOB DESCRIPTION Clinical Pharmacist Specialist I. JOB SUMMARY The Clinical Pharmacist Specialists are responsible and accountable for the provision of safe, effective, and prompt medication therapy. Through various assignments within the department, they provide support of centralized and decentralized medication-use systems as well as deliver optimal medication therapy to patients with a broad range of disease states. Clinical Pharmacist Specialists proficiently provide direct patient-centered care and integrated pharmacy operational services in a decentralized practice setting with physicians, nurses, and other hospital personnel. These clinicians are aligned with target interdisciplinary programs and specialty services to deliver medication therapy management within specialty patient care services and to ensure pharmaceutical care programs are appropriately integrated throughout the institution. In these clinical roles, Clinical Pharmacist Specialists participate in all necessary aspects of the medication-use system while providing comprehensive and individualized pharmaceutical care to the patients in their assigned areas. Pharmaceutical care services include but are not limited to assessing patient needs, incorporating age and disease specific characteristics into drug therapy and patient education, adjusting care according to patient response, and providing clinical interventions to detect, mitigate, and prevent medication adverse events. Clinical Pharmacist Specialists serve as departmental resources and liaisons to other -

Patient Care Through Telepharmacy September 2016
Patient Care through Telepharmacy September 2016 Gregory Janes Objectives 1. Describe why telepharmacy started and how it has evolved with technology 2. Explain how telepharmacy is being used to provide better patient care, especially in rural areas 3. Understand the current regulatory environment around the US and what states are doing with regulation Agenda ● Origins of Telepharmacy ● Why now? ● Telepharmacy process ● Regulatory environment ● Future Applications Telepharmacy Prescription verification CounselingPrescription & verification Education History Origins of Telepharmacy 1942 Australia’s Royal Flying Doctor Service 2001 U.S. has first state pass telepharmacy regulation 2003 Canada begins first telepharmacy service 2010 Hong Kong sees first videoconferencing consulting services US Telepharmacy Timeline 2001 North Dakota first state to allow 2001 Community Health Association in Spokane, WA launches program 2002 NDSU study begins 2003 Alaska Native Medical Center program 2006 U.S. Navy begins telepharmacy 2012 New generation begins in Iowa Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii NDSU Telepharmacy Study Study from 2002-2008 ● 81 pharmacies ○ 53 retail and 28 hospital ● Rate of dispensing errors <1% ○ Compared to national average of ~2% ● Positive outcomes, mechanisms could be improved Source: The North Dakota Experience: Achieving High-Performance -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

A Tool to Help Clinicians Do What They Value Most
Health Information Technology: a Tool to Help Clinicians Do What They Value Most Health care professionals like you play a vital role in improving the health outcomes, quality of care, and the health care experience of patients. Health information technology (health IT) is an important tool that you can use to improve clinical practice and the health of your patients. Health IT can help health care professionals to do what you do best: provide excellent care to your patients. Research shows that when patients are Health IT encompasses a wide range of electronic tools that can help you: engaged in their health care, it can lead to • Access up-to-date evidence-based clinical guidelines and decision measurable improvements in safety and support quality. • Improve the quality of care and safety of your patients Source: Agency for Healthcare Research and Quality (AHRQ) • Provide proactive health maintenance for your patients • Better coordinate patients’ care with other providers through the secure and private sharing of clinical information. Health IT can help you to solve clinical problems with real-time data Quality improvement and clinical decision support rely on information about your patient population being readily available in digital form. Health IT can help you monitor your patients’ health status and make specific and targeted recommendations to improve your patients’ health. Access to real-time data through electronic health records and health IT will help you: A MAJORITY OF PROVIDERS • Use clinical decision support to highlight care options tailored to believe that electronic health information your patients has the potential to improve the quality of patient care and care coordination. -

Pharmacist-Physician Team Approach to Medication-Therapy
Pharmacist-Physician Team Approach to Medication-Therapy Management of Hypertension The following is a synopsis of “Primary-Care-Based, Pharmacist-Physician Collaborative Medication-Therapy Management of Hypertension: A Randomized, Pragmatic Trial,” published online in June 2014 in Clinical Therapeutics. What is already known on this topic? found that the role of the pharmacist differed within each study; whereas some pharmacists independently initiated and High blood pressure, also known as hypertension, is a changed medication therapy, others recommended changes major risk factor for cardiovascular disease, the leading to physicians. Pharmacists were already involved in care in all cause of death for U.S. adults. Helping patients achieve but one study. blood pressure control can be difficult for some primary care providers (PCPs), and this challenge may increase with After reviewing the RCTs, the authors conducted a randomized the predicted shortage of PCPs in the United States by 2015. pragmatic trial to investigate the processes and outcomes that The potential shortage presents an opportunity to expand result from integrating a pharmacist-physician team model. the capacity of primary care through pharmacist-physician Participants were randomly selected to receive PharmD-PCP collaboration for medication-therapy management (MTM). MTM or usual care from their PCPs. The authors conducted MTM performed through a collaborative practice agreement the trial within a university-based internal medicine medical allows pharmacists to initiate and change medications. group where the collaborative PharmD-PCP MTM team Researchers have found positive outcomes associated included an internal medicine physician and two clinical with having a pharmacist on the care team; however, the pharmacists, both with a Doctor of Pharmacy degree, at least evidence is limited to only a few randomized controlled 1 year of pharmacy practice residency training, and more than trials (RCTs). -

Updated Pharmacy Technician Duties Policy and Procedure #140
Approved Technician Duties Policy and Procedure #140 An employee of a pharmacy holding a pharmacy permit not registered with the SC Board of Pharmacy may perform many clerical functions associated with the practice of pharmacy. A non-registered employee is prohibited from performing the following functions: • Entering data beyond demographic information (name, address, date of birth, gender, contact information, insurance, etc) • Interpreting prescription drug orders • Handling non-dispensed legend drugs or devices. • Compounding of any over-the-counter or legend drug A Registered or Certified Pharmacy Technician may perform many clerical functions associated with the practice of pharmacy at a facility holding a pharmacy permit. While fulfilling clerical functions, up to the point of dispensing requiring clinical interpretation and/or product selection, as defined in Section 40-43-30(15), registered or certified technicians would not be considered in the pharmacist to technician ratio as indicated by Sec. 40-43-86 (B)(4)(b). A Registered Pharmacy Technician may perform many technical functions associated with the practice of pharmacy at a facility holding a pharmacy permit; however, even under the direct supervision of a pharmacist, the pharmacy technician is prohibited from performing the following functions: • Performing any duty required by law or regulation to be performed by a state- certified technician, pharmacy intern or extern, or a pharmacist • Administering immunizations • Counseling a patient on a new or refill prescription -

Use of Electronic Health Record Data in Clinical Investigations Guidance for Industry1
Use of Electronic Health Record Data in Clinical Investigations Guidance for Industry U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) Center for Devices and Radiological Health (CDRH) July 2018 Procedural Use of Electronic Health Record Data in Clinical Investigations Guidance for Industry Additional copies are available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10001 New Hampshire Ave., Hillandale Bldg., 4th Floor Silver Spring, MD 20993-0002 Phone: 855-543-3784 or 301-796-3400; Fax: 301-431-6353 Email: [email protected] https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm and/or Office of Communication, Outreach and Development Center for Biologics Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Bldg. 71, Room 3128 Silver Spring, MD 20993-0002 Phone: 800-835-4709 or 240-402-8010 Email: [email protected] https://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/default.htm and/or Office of Communication and Education CDRH-Division of Industry and Consumer Education Center for Devices and Radiological Health Food and Drug Administration 10903 New Hampshire Ave., Bldg. 66, Room 4621 Silver Spring, MD 20993-0002 Phone: 800-638-2041 or 301-796-7100; Fax: 301-847-8149 Email: [email protected] https://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/default.htm U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) Center for Devices and Radiological Health (CDRH) July 2018 Procedural Contains Nonbinding Recommendations TABLE OF CONTENTS I. -

Health Information Technology
Published for 2020-21 school year. Health Information Technology Primary Career Cluster: Business Management and Technology Course Contact: [email protected] Course Code: C12H34 Introduction to Business & Marketing (C12H26) or Health Science Prerequisite(s): Education (C14H14) Credit: 1 Grade Level: 11-12 Focused Elective This course satisfies one of three credits required for an elective Graduation Requirements: focus when taken in conjunction with other Health Science courses. This course satisfies one out of two required courses to meet the POS Concentrator: Perkins V concentrator definition, when taken in sequence in an approved program of study. Programs of Study and This is the second course in the Health Sciences Administration Sequence: program of study. Aligned Student HOSA: http://www.tennesseehosa.org Organization(s): Teachers are encouraged to use embedded WBL activities such as informational interviewing, job shadowing, and career mentoring. Coordinating Work-Based For information, visit Learning: https://www.tn.gov/content/tn/education/career-and-technical- education/work-based-learning.html Available Student Industry None Certifications: 030, 031, 032, 034, 037, 039, 041, 052, 054, 055, 056, 057, 152, 153, Teacher Endorsement(s): 158, 201, 202, 203, 204, 311, 430, 432, 433, 434, 435, 436, 471, 472, 474, 475, 476, 577, 720, 721, 722, 952, 953, 958 Required Teacher None Certifications/Training: https://www.tn.gov/content/dam/tn/education/ccte/cte/cte_resource Teacher Resources: _health_science.pdf Course Description Health Information Technology is a third-level applied course in the Health Informatics program of study intended to prepare students with an understanding of the changing world of health care information. -

Pharmacy/Medical Drug Prior Authorization Form
High Cost Medical Drugs List High Cost Medical Drugs administered by Health Alliance™ providers within physician offices, infusion centers or hospital outpatient settings must be acquired from preferred specialty vendors. Health Alliance will not reimburse any drug listed as a “High Cost Medical Drug,” whether obtained from the provider’s own stock or via “buy-and-bill.” This drug list does not apply to members with Medicare coverage. Information on how to acquire these medications is located at the end of this document. Recent Updates Preferred Contact Drug Therapy Drug Name Code PA Effective Change Vendor Number Oncology – Injectable DARZALEX FASPRO J9144 YES 10/1/2021 CVS/Caremark® 800-237-2767 Added High Cost Medical Drug List Preferred Contact Drug Therapy Drug Name Code PA Effective Vendor Number Acromegaly SANDOSTATIN J2353 YES 7/1/2020 CVS/Caremark® 800-237-2767 Acromegaly SOMATULINE J1930 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products JETREA J7316 YES 7/1/2020 LDD Additional Products PROLASTIN J0256 YES 7/1/2020 LDD Additional Products QUTENZA J7336 NO 7/1/2020 LDD Additional Products REVCOVI J3590 YES 7/1/2020 LDD Additional Products RADICAVA J1301 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products SIGNIFOR J2502 YES 7/1/2020 Accredo® 866-759-1557 Additional Products SPRAVATO J3490 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products STRENSIQ J3590 YES 7/1/2020 LDD Additional Products THIOTEPA J9340 YES 7/1/2020 CVS/Caremark® 800-237-2767 Allergic Asthma CINQAIR J2786 YES 7/1/2020 CVS/Caremark® 800-237-2767