COBRA User's Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cobra the Animation Review
Cobra the animation review [Review] Cobra: The Animation. by Gerald Rathkolb October 12, SHARE. Sometimes, it's refreshing to find something that has little concern with following. May 27, Title: Cobra the Animation Genre: Action/Adventure Company: Magic Bus Format: 12 episodes Dates: 2 Jan to 27 Mar Synopsis: Cobra. Space Adventure Cobra is a hangover from the 80's. it isn't reproduced in this review simply because the number of zeros would look silly. Get ready to blast off, rip-off, and face-off as the action explodes in COBRA THE ANIMATION! The Review: Audio: The audio presentation for. Cobra The Animation – Blu-ray Review. written by Alex Harrison December 5, Sometimes you get a show that is fun and captures people's imagination. visits a Virtual Reality parlor to live out his vague male fantasies, but the experience instead revives memories of being the great space rogue Cobra, scourge of. Here's a quick review. I think that my biggest issue with Cobra is that I unfortunately happened to watch one of the worst Cobra episodes as my. A good reviewer friend of mine, Andrew Shelton at the Anime Meta-Review, has a It's a rating I wish I had when it came to shows like Space Adventure Cobra. Cobra Anime Anthology ?list=PLyldWtGPdps0xDpxmZ95AMcS4wzST1qkq. Not quite a full review, just a quick look at the new Space Adventure Cobra tv series (aka Cobra: the Animation. This isn't always the case though. Sometimes you wonder this same thing about series that are actually good, such as Cobra the Animation. -

Download the Program (PDF)
ヴ ィ ボー ・ ア ニ メー シ カ ョ ワ ン イ フ イ ェ と ス エ ピ テ ッ ィ Viborg クー バ AnimAtion FestivAl ル Kawaii & epikku 25.09.2017 - 01.10.2017 summAry 目次 5 welcome to VAF 2017 6 DenmArk meets JApAn! 34 progrAmme 8 eVents Films For chilDren 40 kAwAii & epikku 8 AnD families Viborg mAngA AnD Anime museum 40 JApAnese Films 12 open workshop: origAmi 42 internAtionAl Films lecture by hAns DybkJær About 12 important ticket information origAmi 43 speciAl progrAmmes Fotorama: 13 origAmi - creAte your own VAF Dog! 44 short Films • It is only possible to order tickets for the VAF screenings via the website 15 eVents At Viborg librAry www.fotorama.dk. 46 • In order to pick up a ticket at the Fotorama ticket booth, a prior reservation Films For ADults must be made. 16 VimApp - light up Viborg! • It is only possible to pick up a reserved ticket on the actual day the movie is 46 JApAnese Films screened. 18 solAr Walk • A reserved ticket must be picked up 20 minutes before the movie starts at 50 speciAl progrAmmes the latest. If not picked up 20 minutes before the start of the movie, your 20 immersion gAme expo ticket order will be annulled. Therefore, we recommended that you arrive at 51 JApAnese short Films the movie theater in good time. 22 expAnDeD AnimAtion • There is a reservation fee of 5 kr. per order. 52 JApAnese short Film progrAmmes • If you do not wish to pay a reservation fee, report to the ticket booth 1 24 mAngA Artist bAttle hour before your desired movie starts and receive tickets (IF there are any 56 internAtionAl Films text authors available.) VAF sum up: exhibitions in Jane Lyngbye Hvid Jensen • If you wish to see a movie that is fully booked, please contact the Fotorama 25 57 Katrine P. -

Rikki-Tikki-Tavi by Rudyard Kipling (From the Jungle Book)
Rikki-tikki-tavi by Rudyard Kipling (from The Jungle Book) At the hole where he went in Red-Eye called to Wrinkle-Skin. Hear what little Red-Eye saith: "Nag, come up and dance with death!" Eye to eye and head to head, (Keep the measure, Nag.) This shall end when one is dead; (At thy pleasure, Nag.) Turn for turn and twist for twist-- ( Run and hide thee, Nag.) Hah! The hooded Death has missed! (Woe betide thee, Nag!) This is the story of the great war that Rikki- him. Perhaps he isn't really dead." tikki-tavi fought single-handed, through the They took him into the house, and a big man bath-rooms of the big bungalow in Segowlee picked him up between his finger and thumb cantonment. Darzee, the Tailorbird, helped him, and said he was not dead but half choked. So and Chuchundra, the musk-rat, who never they wrapped him in cotton wool, and warmed comes out into the middle of the floor, but him over a little fire, and he opened his eyes and always creeps round by the wall, gave him sneezed. advice, but Rikki-tikki did the real fighting. "Now," said the big man (he was an Englishman He was a mongoose, rather like a little cat in his who had just moved into the bungalow), "don't fur and his tail, but quite like a weasel in his frighten him, and we'll see what he'll do." head and his habits. His eyes and the end of his restless nose were pink. -

Richard Epcar Voice Over Resume
RICHARD EPCAR VOICE OVER RESUME ADR DIRECTOR / ORIGINAL ANIMATION DIRECTOR / GAME DIRECTOR ADR WRITER / ENGLISH ADAPTER INTERNATIONAL DUBBING SUPERVISOR 818 426-3415 VOICE OVER REPRESENTATION: (323) 939-0251 VOICE ACTING RESUME GAME VOICE ACTING ARKHAM ORIGINS SEVERAL CHARACTERS WB INJUSTICE: GODS AMONG US THE JOKER WB INFINITE CRISIS THE JOKER WB MORTAL KOMBAT X RAIDEN WARNER BROS. FINAL FANTASY XIV 2.4-2.5 ILBERD ACE COMBAT ASSAULT HORIZON LEGACY STARGATE SG-1: UNLEASHED GEN. GEORGE HAMMOND MGM SAINTS ROW 4 LEAD VOICE (CYRUS TEMPLE) VOICEWORKS PRODS MARVEL HEROS SEVERAL VOICES MARVEL THE BUREAU: XCOM DECLASSIFIED LEAD VOICE TAKE 2 PRODS. BLADE STORM NIGHTMARE NARRATOR ULTIMATE NINJA STORM 3 LEAD VOICE NARUTO VG LEAD VOICE STUDIPOLIS CALL OF DUTY- BLACK OPS II SEVERAL VOICES EA RESIDENT EVIL 6 MO-CAPPED THE PRESIDENT ACTIVISION SKYRIM- THE ELDER SCROLLS V LEAD VOICES BETHESDA (BEST GAME OF THE YEAR 2011-Spike Video Awards) KINGDOM HEARTS: DREAM DROP DISTANCE LEAD VOICE SQUARE ENIX / DISNEY FINAL FANTASY XIV LEAD VOICE (GAIUS VAN BAELSAR) SQUARE ENIX MAD MAX SEVERAL VOICES DEAD OR ALIVE 5 LEAD VOICE VINDICTUS LEAD VOICE TIL MORNING’S LIGHT LEAD VOICE WAY FORWARD POWER RANGERS MEGAFORCE LEAD VOICES BANG ZOOM FINAL FANTASY XIII.3 LEAD VOICE GUILTY GEARS X-RD LEAD VOICE SQUARE ENIX YOGA Wii LEAD VOICE GORMITI LEAD VOICE EARTH DEFENSE FORCE LEAD VOICE 1 ATELIER AYESHA LEAD VOICE BANG ZOOM X-COM: ENEMY UNKNOWN LEAD VOICE TAKE 2 PRODS. OVERSTRIKE LEAD VOICE INSOMNIAC GAMES DEMON’S SCORE LEAD VOICES CALL OF DUTY BLACK OPS LEAD VOICES EA TRANSFORMERS -

Talking Like a Shōnen Hero: Masculinity in Post-Bubble Era
Talking like a Shōnen Hero: Masculinity in Post-Bubble Era Japan through the Lens of Boku and Ore Hannah E. Dahlberg-Dodd The Ohio State University Abstract Comics (manga) and their animated counterparts (anime) are ubiquitous in Japanese popular culture, but rarely is the language used within them the subject of linguistic inquiry. This study aims to address part of this gap by analyzing nearly 40 years’ worth of shōnen anime, which is targeted predominately at adolescent boys. In the early- and mid-20th century, male protagonists saw a shift in first-person pronoun usage. Pre-war, protagonists used boku, but beginning with the post-war Economic Miracle, shōnen protagonists used ore, a change that reflected a shift in hegemonic masculinity to the salaryman model. This study illustrates that a similar change can be seen in the late-20th century. With the economic downturn, salaryman masculinity began to be questioned, though did not completely lose its hegemonic status. This is reflected in shōnen works as a reintroduction of boku as a first- person pronoun option for protagonists beginning in the late 90s. Key words sociolinguistics, media studies, masculinity, yakuwarigo October 2018 Buckeye East Asian Linguistics © The Author 31 1. Introduction Comics (manga) and their animated counterparts (anime) have had an immense impact on Japanese popular culture. As it appears on television, anime, in addition to frequently airing television shows, can also be utilized to sell anything as mundane as convenient store goods to electronics, and characters rendered in an anime-inspired style have been used to sell school uniforms (Toku 2007:19). -

Otakon 2021 Schedule Grid Auto-Generated 2021-08-08 01:26:33
Live and Video Programming Friday Morning/Afternoon (Otakon 2021 schedule grid auto-generated 2021-08-08 01:26:33) Friday Room 9:00 AM 9:15 AM 9:30 AM 9:45 AM 10:00 AM 10:15 AM 10:30 AM 10:45 AM 11:00 AM 11:15 AM 11:30 AM 11:45 AM Friday Main Lvl3 A/B Main Vid 1 Rm 147A A Dog's Courage (2018) (S.Korea) [D][K] InuYasha: Swords of a Honorable Vid 1 Vid 2 Rm 145B Hero Mask 1-4 (2018)(Japan) [S] Jubei-chan: The Ninja Girl 1-4 ( Vid 2 Vid 3 Rm 146B Legendary Armor Samurai Troopers 1-4 (1988)(Japan) [S] S.Cry.ed 1-4 (2001)(Japan) [S] Vid 3 Vid 4 Rm 156 OTAKU no Video (1991)(Japan) [S][MT] Astroganger 1-4 (1972)(Japan) [S Vid 4 AMV Rm 144 Hot Gal (and Guy) Summer The Best Openings You Didn't See The Art AMV ClubOta Rm 206 ClubOta Panel 1 Rm 202 History of the Yandere [F] Evolution of Action Shonen [F] Americanization Panel 1 Panel 2 Rm 207 Thirty Years Ago: Anime in 1991 Swansongs and Bullets [F] VTuber Clipping: Panel 2 Panel 3 Rm 150 Bleach 20th Anniversary [F] Giant Robots: The 90s [F] Aural Anime: Mus Panel 3 Panel 4 Rm 151A Underground Idol Groups [F] Final Fantasy XIV Discussion [F] FukaFuka: Kemono Panel 4 Panel 5 Rm 151B The Beginning of Boys Love Film Smash Presents: Gourmet Cin Cosplaying Broke Panel 5 Panel 6 Rm 152A Japanese Fashion on a Budget Japanese Indie Music Otaku Parenting: Panel 6 Panel 7 Rm 146C From Alefgard to Zwaardsrust: Th Anime Food, How Panel 7 Wkshp 1 Rm 143 Origami 101 Translat Wkshp 1 Wkshp 2 Rm 140 Cosplay 201: Armor Patterning Wkshp 2 Wkshp 3 Rm 146A Realistic Martial Arts/Fighting Zumba Class - Anime Style Wkshp -

Sentai Filmworks
Sentai Filmworks - DVD Release Checklist: # - C A complete list of all 325 anime title releases and their 617 volumes and editions, with catalog numbers when available. 11 Eyes Azumanga Daioh: The Animation - Complete Collection (SF-EE100) - Complete Collection (Sentai Selects) (SFS-AZD100) A Little Snow Fairy Sugar Bakuon!! - Collection 1 (SF-LSF100) - Complete Collection (SF-BKN100) - Collection 2 (SF-LSF200) - Complete Collection (Sentai Selects) (SFS-LSF110) Battle Girls: Time Paradox - Complete Collection (SF-SGO100) A-Channel: The Animation - Complete Collection (SF-AC100) Beautiful Bones: Sakurako's Investigation - Complete Collection (SF-BBS100) Ajin: Demi-Human - Complete Collection (SF-AJN100) Beyond the Boundary - Limited Edition (BD/DVD Combo) (SFC-AJN100) - Complete Collection (SF-BTB100) - Season 2: Complete Collection (SF-AJN200) - Complete Collection: Limited Edition (BR/DVD Combo) (SFC-BTB100) - Season 2: Limited Edition (BD/DVD Combo) (SFC-AJN200) - I'll Be Here (BD/DVD Combo) (SFC-BTB001) Akame ga Kill! Black Bullet - Collection 1 (SF-AGK101) - Complete Collection (SF-BKB100) - Collection 1: Limited Edition (BD/DVD Combo) (SFC-AGK101) - Collection 2 (SF-AGK102) Blade & Soul - Collection 2: Limited Edition (BD/DVD Combo) (SFC-AGK102) - Complete Collection (SF-BAS100) Akane Iro ni Somaru Saka Blade Dance of the Elementalers - Complete Collection (SF-AIS100) - Complete Collection (SF-BDE100) AKB0048 Blue Drop - Season One: Complete Collection (SF-AKB100) - The Complete Series (2009, subbed) - Next Stage: Complete Collection -
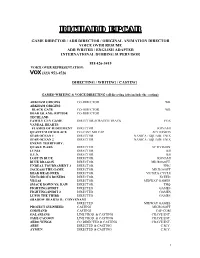
Please Click HERE to Download My Voice Directing
RICHARD EPCAR GAME DIRECTOR / ADR DIRECTOR / ORIGINAL ANIMATION DIRECTOR VOICE OVER RESUME ADR WRITER / ENGLISH ADAPTER INTERNATIONAL DUBBING SUPERVISOR 818 426-3415 VOICE OVER REPRESENTATION: (323) 951-4526 DIRECTING / WRITING / CASTING GAMES–WRITING & VOICE DIRECTING (all directing jobs include the casting) ARKHAM ORIGINS CO-DIRECTOR WB ARKHAM ORIGINS: BLACK GATE CO-DIRECTOR WB DEAD ISLAND: RIPTIDE CO-DIRECTOR TECHLAND FAMILY GUY GAME DIRECTOR-SCRATCH TRACK FOX VANDAL HEARTS: FLAMES OF JUDGEMENT DIRECTOR KONAMI QUANTUM OF SOLACE CO-CAST MO CAP ACTIVISION STAR OCEAN 1 DIRECTOR NANICA / SQUARE ENIX STAR OCEAN 2 DIRECTOR NANICA / SQUARE ENIX ENEMY TERRITORY: QUAKE WARS DIRECTER ACTIVISION LUNIA DIRECTOR IJJI S.U.N. DIRECTOR IJJI LOST IN BLUE DIRECTOR KONAMI BLUE DRAGON DIRECTOR MICROSOFT UNREAL TOURNAMENT 3 DIRECTOR EPIC JACKASS THE GAME DIRECTOR MICROSOFT DEAD HEAD FRED DIRECTOR VICIOUS CYCLE VICTORIOUS BOXERS DIRECTOR XCEED VEGAS DIRECTOR MIDWAY GAMES SMACK DOWN VS. RAW DIRECTOR THQ FIGHTING SPIRIT DIRECTED GAMES FIGHTING SPIRIT 2 DIRECTED GAMES LUPIN THE THIRD DIRECTED GAMES SHADOW HEARTS II: CONVENANT DIRECTED MIDWAY GAMES PROJECT SYLPHEED CASTING MICROSOFT GODHAND CASTING CAP-COM GALARIANS LINE PROD. & CASTING CRAVE ENT. JADE CACOON LINE PROD. & CASTING CRAVE ENT. AERO WINGS CO-DIRECTED & CASTING CRAVE ENT. ABBY DIRECTED & CASTING C.M.Y. AYMUN DIRECTED & CASTING C.M.Y. 1 ANIMATED CARTOONS – FEATURES AND TELEVISION-WRITING & DIRECTING KICK-HEART CAST/WROTE & DIRECTED PROD I-G ALMOST HEROES ADR DIRECTOR DIGIART JUNGLE SHUFFLE ADR DIRECTOR SPACE DOGS 3-D CAST/WROTE & DIRECTED EPIC BLUE ELEPHANT CAST/CO-DIRECTED WEINSTEIN CO. GHOST IN THE SHELL 2- INNOCENCE WROTE & DIRECTED-FEATURE MANGA U.K. -

View Full Catalog of Encoded Compatible Content
D-BOX HOME ENTERTAINEMENT IMMERSIVE EXPERIENCES (Hold the Ctrl keyboard key and press the F (Ctrl+F) to search for a specific movie) HaptiCode Release Date RECENTLY ADDED (Year-Month-Day) Star Wars: The Bad Batch - 1st Season EP11 2021-07-09 Black Widow 2021-07-09 Lupin 1st Season EP 6,7 2021-07-07 Loki 1st Season EP 4 2021-07-06 Ace Venture - When Nature Calls 2021-07-06 Ace Ventura - Pet Detective 2021-07-06 Star Wars: The Bad Batch - 1st Season EP10 2021-07-02 Lupin 1st Season EP 4,5 2021-06-30 Loki 1st Season EP 3 2021-06-29 Star Wars: The Bad Batch - 1st Season EP9 2021-06-25 Always 2021-06-23 Lupin 1st Season EP 2,3 2021-06-23 Loki 1st Season EP 2 2021-06-22 Jack Ryan - 2nd Season EP 7,8 2021-06-22 Star Wars: The Bad Batch - 1st Season EP8 2021-06-18 Astérix - The Mansion of the Gods 2021-06-17 Lupin 1st Season EP 1 2021-06-16 Wandavision 1st Season EP 9 2021-06-16 Loki 1st Season EP 1 2021-06-15 Jack Ryan - 2nd Season EP 5,6 2021-06-15 Star Wars: The Bad Batch - 1st Season EP7 2021-06-11 In the Heights 2021-06-11 Wandavision 1st Season EP 7,8 2021-06-09 Jack Ryan - 2nd Season EP 3,4 2021-06-08 Star Wars: The Bad Batch - 1st Season EP6 2021-04-06 Conjuring : The Devil Made Me Do It 2021-06-04 Wandavision 1st Season EP 5,6 2021-06-02 Jack Ryan - 2nd Season EP 1,2 2021-06-01 Star Wars: The Bad Batch - 1st Season EP5 2021-05-28 Cruella 2021-05-28 Star Wars: The Clone Wars S07 EP 9,10,11,12 2021-05-27 Wandavision 1st Season EP 3,4 2021-05-26 Get Him to the Greek 2021-05-25 Jack Ryan 1st Season EP 7,8 2021-05-25 Star Wars: The Bad Batch -

CELEBRATING FORTY YEARS of FILMS WORTH TALKING ABOUT This Projector Goes up to 4K
6 JUL 18 2 AUG 18 1 | 6 JUL 18 - 2 AUG 18 88 LOTHIAN ROAD | FILMHOUSECinema.COM CELEBRATING FORTY YEARS OF FILMS WORTH TALKING ABOUT This projector goes up to 4K... There’s a few mentions in this document of the term “4K”, and before you dive in I‘d like to just take a moment to explain what it actually means. I don’t want to insult anyone on the one hand by mansplaining it (a crime of which, of course, I have never been accused) or on the other by just telling you to “Google It”, so hopefully what I’m about to say lands somewhere in between. “4K”, when used in connection with a digital cinema projector, refers to the number of pixels, horizontally, in the full frame image (more accurately, it would be called 4096 pixels!). Early digital cinema projectors were all 2K (2048 pixels!), as was the case for the ones we have just replaced. The 2K projector in Cinema One has been replaced by a 4K one, which places us at the vanguard of modern cinema exhibition, in terms of the resolution of the image that hits our screen, when the film is provided in that format. 4K will likely become the norm over time, but for now it’s still relatively rare. But... many recently restored classic films have been restored in 4K, and what I’m trying to tell you in an increasingly roundabout way is we’re planning to show off our new kit by showing a great number of them across July and August! (See page 24-26 for July’s selection, though I’ll throw in 2001: A Space Odyssey as a taster!) It’s very exciting, and highly unlikely you will ever have seen these amazing films look so darned good. -

Newsletter 05/09 DIGITAL EDITION Nr
ISSN 1610-2606 ISSN 1610-2606 newsletter 05/09 DIGITAL EDITION Nr. 247 - März 2009 Michael J. Fox Christopher Lloyd LASER HOTLINE - Inh. Dipl.-Ing. (FH) Wolfram Hannemann, MBKS - Talstr. 3 - 70825 K o r n t a l Fon: 0711-832188 - Fax: 0711-8380518 - E-Mail: [email protected] - Web: www.laserhotline.de Newsletter 05/09 (Nr. 247) März 2009 Die FANTASY FILMFEST NIGHTS 2009 Ein kurzes Resumee von Wolfram Hannemann DEADGIRL (1:2.35, DVD, DS) HORSEMEN (1:1.85, DD 5.1) USA 2008 / ENGLISCHE OV USA 2009 / ENGLISCHE OV REGIE Marcel Sarmiento / Gadi Harel REGIE Jonas Åkerlund DARSTELLER DARSTELLER Noah Segan / Shiloh Dennis Quaid / Ziyi Zhang / Patrick Fugit / Fernandez / Candice Accola / Eric Podnar / Lou Taylor Pucci / Clifton Collins Jr. / Eric Jenny Spain / Andrew DiPalma / Nolan Balfour / Peter Stormare DREHBUCH Da- Gerard Funk / Michael Bowen DREH- vid Callaham PRODUZENTEN Michael BUCH Trent Haaga PRODUZENTEN Bay / Andrew Form / Brad Fuller VERLEIH Marcel Sarmiento / Gadi Harel VERLEIH Concorde Filmverleih Ascot Elite Home Entertainment Wenn einem schon in den ersten Minuten Da finden zwei Schüler in einem verlasse- des Films das Bauchgefühl sagt, dass man nen Krankenhaus im allerletzten Winkel im den Mörder bereits kennt, dann sollte man Kellergeschoss eine nackte Frau, die auf sich auf dieses Bauchgefühl verlassen. einen Tisch gefesselt ist. Und offensicht- Nachteil ist dann natürlich, dass der dann lich ist die Dame nicht von dieser Welt: folgende Film extrem langweilig wirkt. weder Pistolenkugeln noch Messerstiche HORSEMEN ist ein solches Beispiel. Da können ihr etwas anhaben. Die Jungs be- soll ein stark gealterter Dennis Quaid als schließen, die Dame als ihr persönliche Ermittler eine Serie von grausamen Morden Sexsklavin zu benutzen.. -

You've Seen the Movie, Now Play The
“YOU’VE SEEN THE MOVIE, NOW PLAY THE VIDEO GAME”: RECODING THE CINEMATIC IN DIGITAL MEDIA AND VIRTUAL CULTURE Stefan Hall A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY May 2011 Committee: Ronald Shields, Advisor Margaret M. Yacobucci Graduate Faculty Representative Donald Callen Lisa Alexander © 2011 Stefan Hall All Rights Reserved iii ABSTRACT Ronald Shields, Advisor Although seen as an emergent area of study, the history of video games shows that the medium has had a longevity that speaks to its status as a major cultural force, not only within American society but also globally. Much of video game production has been influenced by cinema, and perhaps nowhere is this seen more directly than in the topic of games based on movies. Functioning as franchise expansion, spaces for play, and story development, film-to-game translations have been a significant component of video game titles since the early days of the medium. As the technological possibilities of hardware development continued in both the film and video game industries, issues of media convergence and divergence between film and video games have grown in importance. This dissertation looks at the ways that this connection was established and has changed by looking at the relationship between film and video games in terms of economics, aesthetics, and narrative. Beginning in the 1970s, or roughly at the time of the second generation of home gaming consoles, and continuing to the release of the most recent consoles in 2005, it traces major areas of intersection between films and video games by identifying key titles and companies to consider both how and why the prevalence of video games has happened and continues to grow in power.