INVOKAMET® Safely and Effectively
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metformin Plus Saxagliptin for Type 2 Diabetes
Treatment evaluation Metformin plus saxagliptin for type 2 diabetes André J. Scheen Division of Diabetes, Nutrition and Metabolic Disorders and Division of Clinical Pharmacology, Department of Medicine, CHU Sart Tilman, University of Liège, Liège, Belgium Running title : Saxagliptin plus metformin Word count : Abstract : 148 Main text : 2404 Tables : 4 Figures : 0 Address for correspondence : Pr André J. SCHEEN Department of Medicine CHU Sart Tilman (B35) B-4000 LIEGE 1 BELGIUM Phone : 32-4-3667238 FAX : 32-4-3667068 Page 1 Email : andre.scheen @ chu.ulg.ac.be SUMMARY Metformin is considered as the first-line drug therapy for the management of type 2 diabetes. Dipeptidyl peptidase-4 (DPP-4) inhibitors, by promoting insulin secretion and reducing glucagon secretion in a glucose-dependent manner, offer new opportunities for oral therapy after failure of metformin. Saxagliptin, a DPP-4 inhibitor, and metformin may be administered together, separately or in fixed-dose combination (FDC), either as saxagliptin added to metformin or as initial combination in drug-naive patients. Both compounds exert complementary pharmacodynamic actions leading to better improvement in blood glucose control (fasting plasma glucose, postprandial glucose, HbA1c) than either compound separately. Adding saxagliptin to metformin monthotherapy results in a consistent, sustained and safe reduction in HbA1c levels. Tolerance is excellent without hypoglycemia or weight gain. The combination saxaglitpin plus metformin may be used as first-line or second-line therapy in the management of type 2 diabetes, especially as a valuable alternative to the classical metformin-sulfonylurea combination. Key-words : DPP-4 inhibitor – Fixed-dose combination - Metformin – Saxagliptin - Type 2 diabetes mellitus Page 2 1. -

CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence On
cancers Review CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence on Cancer Biology Emi Kawakita 1 , Daisuke Koya 2,3 and Keizo Kanasaki 1,3,* 1 Internal Medicine 1, Shimane University Faculty of Medicine, 89-1 Enya-cho, Izumo 693-8501, Japan; [email protected] 2 Department of Diabetology & Endocrinology, Kanazawa Medical University, Uchinada 920-0293, Japan; [email protected] 3 Division of Anticipatory Molecular Food Science and Technology, Medical Research Institute, Kanazawa Medical University, Uchinada 920-0293, Japan * Correspondence: [email protected]; Tel.: +81-853-20-2183 Simple Summary: Dipeptidyl peptidase (DPP)-4 inhibitor is widely used for type 2 diabetes. Al- though DPP-4/CD26 has been recognized as both a suppressor and inducer in tumor biology due to its various functions, how DPP-4 inhibitor affects cancer progression in diabetic patients is still unknown. The aim of this review is to summarize one unfavorable aspect of DPP-4 inhibitor in cancer-bearing diabetic patients. Abstract: DPP-4/CD26, a membrane-bound glycoprotein, is ubiquitously expressed and has diverse biological functions. Because of its enzymatic action, such as the degradation of incretin hormones, DPP-4/CD26 is recognized as the significant therapeutic target for type 2 diabetes (T2DM); DPP- 4 inhibitors have been used as an anti-diabetic agent for a decade. The safety profile of DPP-4 inhibitors for a cardiovascular event in T2DM patients has been widely analyzed; however, a clear association between DPP-4 inhibitors and tumor biology is not yet established. Previous preclinical Citation: Kawakita, E.; Koya, D.; Kanasaki, K. -

Think Medicines!
Think Issue 13 August 2016 MHRA Drug Safety SGLT2 inhibitors: updated advice on the risk of diabetic Medicines!Updates can be found ketoacidosis (DKA) at the following link. The MHRA are advising health care professionals to test for raised ketones in patients with ketoacidosis symptoms, who are taking SGLT2 inhibitors even if New higher strength Humalog® plasma glucose levels are near-normal. SGLT2 inhibitors include: Canagliflozin, 200 units/ml KwikPen™ Dapagliflozin and Empagliflozin. Serious, life-threatening, and fatal cases of In order to minimize medication DKA have been reported in patients taking an SGLT2 inhibitor. In several cases, errors. blood glucose levels were only moderately elevated (e.g. <14mmol/L) Insulin lispro 200 units/ml representing an atypical presentation for DKA, which could delay diagnosis and solution for injection should treatment. ONLY be administered using the Advice for health Care Professionals: Humalog 200 units/ml pre-filled Inform patients of the signs of diabetic ketoacidosis (DKA) and advise them to pen (KwikPen). seek immediate medical advice if they develop any of these symptoms (e.g. When switching from one rapid weight loss, feeling sick or being sick, stomach pain, fast and deep Humalog strength to another, breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the dose does not need to be the mouth, or a different odour to urine or sweat). converted. Unnecessary dose Discuss the risk factors of DKA with patients. conversion may lead to under/ Discontinue treatment with the SGLT2 inhibitor immediately if DKA is over dosing and resultant hyper/ suspected or diagnosed. -

Komboglyze, INN-Saxagliptin, Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Komboglyze 2.5 mg/850 mg film-coated tablets Komboglyze 2.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Komboglyze 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 850 mg of metformin hydrochloride. Komboglyze 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 1,000 mg of metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Komboglyze 2.5 mg/850 mg film-coated tablets Light brown to brown, biconvex, round, film-coated tablets, with “2.5/850” printed on one side and “4246” printed on the other side, in blue ink. Komboglyze 2.5 mg/1,000 mg film-coated tablets Pale yellow to light yellow, biconvex, oval shaped, film-coated tablets, with “2.5/1000” printed on one side and “4247” printed on the other side, in blue ink. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Komboglyze is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: in patients inadequately controlled on their maximally tolerated dose of metformin alone in combination with other medicinal products for the treatment of diabetes, including insulin, in patients inadequately controlled with metformin and these medicinal products (see sections 4.4, 4.5 and 5.1 for available data on different combinations) in patients already being treated with the combination of saxagliptin and metformin as separate tablets. -

IHS PROVIDER September 2017
September 2017 Volume 42 Number 9 Indian Health Service National Pharmacy and Therapeutics Committee SGLT-2 inhibitors (Update) NPTC Formulary Brief August Meeting 2017 Background: The FDA has currently approved three SGLT-2 inhibitors, two of which have completed FDA-mandated cardiovascular outcomes trials. Last year, in the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG), empagliflozin not only reduced cardiovascular events, but also mortality.1 This year, the Canagliflozin Cardiovascular Assessment Study (CANVAS) demonstrated equivocal cardiovascular benefits, no mortality benefit, and significant harms in those receiving canagliflozin.2 The DECLARE-TIMI 58 cardiovascular study of dapagliflozin will be completed in April 2019 (ClinicalTrials.gov Identifier: NCT01730534). Uncertainty remains regarding the current data, long- term benefits and harms, and differentiation among SGLT-2 inhibitors. Following a review of SGLT2 inhibitors at the August 2017 NPTC meeting on their cardiovascular outcomes, net benefit and place in therapy, no modifications were made to the National Core Formulary (NCF). Discussion: EMPA-REG enrolled 7,020 patients with Type 2 diabetes mellitus (T2DM) and HgbA1c values between 7.0-10.0%. All patients had established cardiovascular disease (CVD) and were observed for a median duration of 3.1 years. Empagliflozin reduced the primary outcome of cardiovascular (CV) death, nonfatal myocardial infarction (MI), or nonfatal cardiovascular accident (CVA) by 6.5 events per 1000 patient-years (pt-yrs). Mortality decreased by 9.2 events per 1000 pt-yrs, primarily driven by a reduction in CV mortality of 7.8 events per 1000 pt-yrs. Heart failure hospitalization decreased by 5.1 events per 1000 pt-yrs. -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

AVANDIA (Rosiglitazone Maleate Tablets), for Oral Use Ischemic Cardiovascular (CV) Events Relative to Placebo, Not Confirmed in Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------- WARNINGS AND PRECAUTIONS ----------------------- These highlights do not include all the information needed to use • Fluid retention, which may exacerbate or lead to heart failure, may occur. AVANDIA safely and effectively. See full prescribing information for Combination use with insulin and use in congestive heart failure NYHA AVANDIA. Class I and II may increase risk of other cardiovascular effects. (5.1) • Meta-analysis of 52 mostly short-term trials suggested a potential risk of AVANDIA (rosiglitazone maleate tablets), for oral use ischemic cardiovascular (CV) events relative to placebo, not confirmed in Initial U.S. Approval: 1999 a long-term CV outcome trial versus metformin or sulfonylurea. (5.2) • Dose-related edema (5.3) and weight gain (5.4) may occur. WARNING: CONGESTIVE HEART FAILURE • Measure liver enzymes prior to initiation and periodically thereafter. Do See full prescribing information for complete boxed warning. not initiate therapy in patients with increased baseline liver enzyme levels ● Thiazolidinediones, including rosiglitazone, cause or exacerbate (ALT >2.5X upper limit of normal). Discontinue therapy if ALT levels congestive heart failure in some patients (5.1). After initiation of remain >3X the upper limit of normal or if jaundice is observed. (5.5) AVANDIA, and after dose increases, observe patients carefully for signs • Macular edema has been reported. (5.6) and symptoms of heart failure (including excessive, rapid weight gain; • Increased incidence of bone fracture was observed in long-term trials. dyspnea; and/or edema). If these signs and symptoms develop, the heart (5.7) failure should be managed according to current standards of care. -

Ertugliflozin 5Mg, 15Mg Film-Coated Tablet (Steglatro®) Merck Sharp & Dohme
1 www.scottishmedicines.org.uk SMC2102 ertugliflozin 5mg, 15mg film-coated tablet (Steglatro®) Merck Sharp & Dohme 7 December 2018 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHSScotland. The advice is summarised as follows: ADVICE: following a full submission ertugliflozin (Steglatro®) is accepted for restricted use within NHSScotland. Indication under review: in adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes. SMC restriction: ertugliflozin is accepted for use as monotherapy and as add-on therapy. When used as monotherapy it is restricted to patients who would otherwise receive a dipeptidyl peptidase-4 inhibitor and in whom a sulphonylurea or pioglitazone is not appropriate. Ertugliflozin was superior to placebo in lowering HbA1c in adults with type 2 diabetes mellitus in phase III studies in monotherapy, dual therapy and triple therapy settings. Chairman Scottish Medicines Consortium Published 14 January 2019 1 Indication In adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes.1 Dosing Information The recommended starting dose is 5mg orally once daily which can, if tolerated, be increased to 15mg once daily if additional glycaemic control is needed. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -
Taking Metformin for Gestational Diabetes This Information Sheet Will Help You Understand More About Taking Metformin for Gestational Diabetes
Taking metformin for gestational diabetes This information sheet will help you understand more about taking metformin for gestational diabetes. This information sheet is not a substitute for talking with your midwife, doctor, nurse or pharmacist. Gestational diabetes Risks for your baby: Gestational diabetes means you have too much • may grow larger than normal (this increases the glucose (a type of sugar) in your blood when you risk of injury during birth) are pregnant. Insulin controls the amount of • born too early (premature) glucose in your blood. Sometimes you don’t make • low blood glucose after birth enough insulin or it doesn’t work as well when you are pregnant. • may need treatment in hospital • jaundice (yellow skin) that needs treatment Gestational diabetes is common. Up to eight pregnant women in every 100 get gestational • breathing problems. diabetes. Taking metformin helps reduce these risks. It can be hard to tell if you have gestational You can see how many women and babies are diabetes. Some women find that they: affected and how treatment helps in the picture • lack energy on the next page. • feel thirsty a lot • go to the toilet a lot Metformin is safe to take for • get lots of infections. gestational diabetes Metformin has been tested in clinical studies and Some women have no symptoms. This is why all is safe to take for gestational diabetes. pregnant women are tested for diabetes so they Metformin helps keep both your weight gain and can get treatment. blood pressure down. Metformin The main side effect is stomach upsets such as Metformin is a medicine that has been used feeling sick and diarrhoea. -
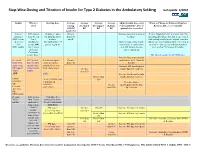
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option.