Corticosteroid-Binding Globulin (Cbg): Deficiencies and the Role
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Identification of an Alpha-1 Antitrypsin Variant with Enhanced Specificity For
www.nature.com/scientificreports OPEN Identifcation of an alpha‑1 antitrypsin variant with enhanced specifcity for factor XIa by phage display, bacterial expression, and combinatorial mutagenesis Varsha Bhakta1, Mostafa Hamada2, Amy Nouanesengsy2, Jessica Lapierre2, Darian L. Perruzza2 & William P. Shefeld1,2* Coagulation Factor XIa (FXIa) is an emerging target for antithrombotic agent development. The M358R variant of the serpin alpha‑1 antitrypsin (AAT) inhibits both FXIa and other proteases. Our aim was to enhance the specifcity of AAT M358R for FXIa. We randomized two AAT M358R phage display libraries at reactive centre loop positions P13‑P8 and P7‑P3 and biopanned them with FXIa. A bacterial expression library randomized at P2′‑P3′ was also probed. Resulting novel variants were expressed as recombinant proteins in E. coli and their kinetics of FXIa inhibition determined. The most potent FXIa‑inhibitory motifs were: P13‑P8, HASTGQ; P7‑P3, CLEVE; and P2‑P3′, PRSTE (respectively, novel residues bolded). Selectivity for FXIa over thrombin was increased up to 34‑fold versus AAT M358R for these single motif variants. Combining CLEVE and PRSTE motifs in AAT‑RC increased FXIa selectivity for thrombin, factors XIIa, Xa, activated protein C, and kallikrein by 279‑, 143‑, 63‑, 58‑, and 36‑fold, respectively, versus AAT M358R. AAT‑RC lengthened human plasma clotting times less than AAT M358R. AAT‑RC rapidly and selectively inhibits FXIa and is worthy of testing in vivo. AAT specifcity can be focused on one target protease by selection in phage and bacterial systems coupled with combinatorial mutagenesis. Trombosis, the blockage of intact blood vessels by occlusive clots, continues to impose a heavy clinical burden, and is responsible for one quarter of deaths world-wide1. -

COMMENTARY Possible New Mechanism of Cortisol Action In
211 COMMENTARY Possible new mechanism of cortisol action in female reproductive organs: physiological implications of the free hormone hypothesis C Yding Andersen Laboratory of Reproductive Biology, Section 5712, University Hospital of Copenhagen, DK-2100 Copenhagen, Denmark (Requests for offprints should be addressed to C Yding Andersen; Email: [email protected]) Abstract The so-called free hormone hypothesis predicts that the cortisol to cortisone, while 11-HSD type 1 reverses this biological activity of a given steroid correlates with the free reaction. As a result, a high concentration of cortisol protein-unbound concentration rather than with the total available for biological action is present in the preovulatory concentration (i.e. free plus protein-bound). Cortisol is a follicle just prior to ovulation and it has been suggested that glucocorticoid with many diverse functions and the free cortisol may function to reduce the inflammatory-like hormone hypothesis seems to apply well to the observed reactions occurring in connection with ovulation. effects of cortisol. The ovaries express glucocorticoid This paper suggests (1) that the function of the oviduct receptors and are affected by cortisol, but lack the neces- is also affected by the high levels of free cortisol released in sary enzymes for cortisol synthesis. Ovarian follicles modu- preovulatory follicular fluid at ovulation and (2) that late the biological activity of cortisol by (1) follicular formation and function of the corpus luteum benefits from production of especially progesterone and 17-hydroxy- a high local concentration of free cortisol, whereas the progesterone which, within the follicle, reach levels that surrounding developing follicles may experience negative displace cortisol from its binding proteins, in particular, effects. -

Polygenic Risk Score of SERPINA6/SERPINA1 Associates with Diurnal and Stress-Induced HPA Axis Activity in Children
Edinburgh Research Explorer Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and stress-induced HPA axis activity in children Citation for published version: Utge, S, Räikkönen, K, Kajantie, E, Lipsanen, J, Andersson, S, Strandberg, T, Reynolds, R, Eriksson, JG & Lahti, J 2018, 'Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and stress-induced HPA axis activity in children', Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2018.04.009 Digital Object Identifier (DOI): 10.1016/j.psyneuen.2018.04.009 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Psychoneuroendocrinology General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 29. Sep. 2021 Psychoneuroendocrinology 93 (2018) 1–7 Contents lists available at ScienceDirect Psychoneuroendocrinology journal homepage: www.elsevier.com/locate/psyneuen Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and T stress-induced HPA axis activity in children Siddheshwar Utgea,b, Katri Räikkönena, Eero Kajantiec,d,e, Jari Lipsanena, Sture Anderssond, ⁎ Timo Strandbergf,g, Rebecca M. -

Human Plasma and Recombinant Hemopexins: Heme Binding Revisited
International Journal of Molecular Sciences Article Human Plasma and Recombinant Hemopexins: Heme Binding Revisited Elena Karnaukhova 1,*, Catherine Owczarek 2, Peter Schmidt 2, Dominik J. Schaer 3 and Paul W. Buehler 4,5,* 1 Center for Biologics Evaluation and Research, Food and Drug Administration, Silver Spring, MD 20993, USA 2 CSL Limited, Bio21 Institute, Parkville, Victoria 3010, Australia; [email protected] (C.O.); [email protected] (P.S.) 3 Division of Internal Medicine, University Hospital of Zurich, 8091 Zurich, Switzerland; [email protected] 4 Department of Pathology, The University of Maryland School of Medicine, Baltimore, MD 21201, USA 5 The Center for Blood Oxygen Transport and Hemostasis, Department of Pediatrics, The University of Maryland School of Medicine, Baltimore, MD 21201, USA * Correspondence: [email protected] (E.K.); [email protected] (P.W.B.) Abstract: Plasma hemopexin (HPX) is the key antioxidant protein of the endogenous clearance pathway that limits the deleterious effects of heme released from hemoglobin and myoglobin (the term “heme” is used in this article to denote both the ferrous and ferric forms). During intra-vascular hemolysis, heme partitioning to protein and lipid increases as the plasma concentration of HPX declines. Therefore, the development of HPX as a replacement therapy during high heme stress could be a relevant intervention for hemolytic disorders. A logical approach to enhance HPX yield involves recombinant production strategies from human cell lines. The present study focuses on a biophysical assessment of heme binding to recombinant human HPX (rhHPX) produced in the Expi293FTM (HEK293) cell system. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Mrna Vaccine Era—Mechanisms, Drug Platform and Clinical Prospection
International Journal of Molecular Sciences Review mRNA Vaccine Era—Mechanisms, Drug Platform and Clinical Prospection 1, 1, 2 1,3, Shuqin Xu y, Kunpeng Yang y, Rose Li and Lu Zhang * 1 State Key Laboratory of Genetic Engineering, Institute of Genetics, School of Life Science, Fudan University, Shanghai 200438, China; [email protected] (S.X.); [email protected] (K.Y.) 2 M.B.B.S., School of Basic Medical Sciences, Peking University Health Science Center, Beijing 100191, China; [email protected] 3 Shanghai Engineering Research Center of Industrial Microorganisms, Shanghai 200438, China * Correspondence: [email protected]; Tel.: +86-13524278762 These authors contributed equally to this work. y Received: 30 July 2020; Accepted: 30 August 2020; Published: 9 September 2020 Abstract: Messenger ribonucleic acid (mRNA)-based drugs, notably mRNA vaccines, have been widely proven as a promising treatment strategy in immune therapeutics. The extraordinary advantages associated with mRNA vaccines, including their high efficacy, a relatively low severity of side effects, and low attainment costs, have enabled them to become prevalent in pre-clinical and clinical trials against various infectious diseases and cancers. Recent technological advancements have alleviated some issues that hinder mRNA vaccine development, such as low efficiency that exist in both gene translation and in vivo deliveries. mRNA immunogenicity can also be greatly adjusted as a result of upgraded technologies. In this review, we have summarized details regarding the optimization of mRNA vaccines, and the underlying biological mechanisms of this form of vaccines. Applications of mRNA vaccines in some infectious diseases and cancers are introduced. It also includes our prospections for mRNA vaccine applications in diseases caused by bacterial pathogens, such as tuberculosis. -

Part I Biopharmaceuticals
1 Part I Biopharmaceuticals Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 3 1 Analogs and Antagonists of Male Sex Hormones Robert W. Brueggemeier The Ohio State University, Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, Columbus, Ohio 43210, USA 1Introduction6 2 Historical 6 3 Endogenous Male Sex Hormones 7 3.1 Occurrence and Physiological Roles 7 3.2 Biosynthesis 8 3.3 Absorption and Distribution 12 3.4 Metabolism 13 3.4.1 Reductive Metabolism 14 3.4.2 Oxidative Metabolism 17 3.5 Mechanism of Action 19 4 Synthetic Androgens 24 4.1 Current Drugs on the Market 24 4.2 Therapeutic Uses and Bioassays 25 4.3 Structure–Activity Relationships for Steroidal Androgens 26 4.3.1 Early Modifications 26 4.3.2 Methylated Derivatives 26 4.3.3 Ester Derivatives 27 4.3.4 Halo Derivatives 27 4.3.5 Other Androgen Derivatives 28 4.3.6 Summary of Structure–Activity Relationships of Steroidal Androgens 28 4.4 Nonsteroidal Androgens, Selective Androgen Receptor Modulators (SARMs) 30 4.5 Absorption, Distribution, and Metabolism 31 4.6 Toxicities 32 Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 4 Analogs and Antagonists of Male Sex Hormones 5 Anabolic Agents 32 5.1 Current Drugs on the Market 32 5.2 Therapeutic Uses and Bioassays -

The Serpintine Solution
& Experim l e ca n i t in a l l C C f a Journal of Clinical & Experimental o r d l i a o n l o r g u Lucas et al., J Clin Exp Cardiolog 2017, 8:1 y o J Cardiology ISSN: 2155-9880 DOI: 10.4172/2155-9880.1000e150 Editorial Open Access The Serpintine Solution Alexandra Lucas, MD, FRCP(C)1,2,*, Sriram Ambadapadi, PhD1, Brian Mahon, PhD3, Kasinath Viswanathan, PhD4, Hao Chen, MD, PhD5, Liying Liu, MD6, Erbin Dai, MD6, Ganesh Munuswami-Ramanujam, PhD7, Jacek M. Kwiecien, DVM, MSc, PhD8, Jordan R Yaron, PhD1, Purushottam Shivaji Narute, BVSc & AH, MVSc, PhD1,9, Robert McKenna, PhD10, Shahar Keinan, PhD11, Westley Reeves, MD, PhD12, Mark Brantly, MD, PhD13, Carl Pepine, MD, FACC14 and Grant McFadden, PhD1 1Center for Personalized Diagnostics, Biodesign Institute, Arizona State University, Tempe AZ, USA 2Saint Josephs Hospital, Dignity Health Phoenix, Phoenix, AZ, USA 3NIH/ NIDDK, Bethesda MD, USA 4Zydus Research Centre, Ahmedabad, India 5Department of tumor surgery, The Second Hospital of Lanzhou University, Lanzhou, Gansu, P.R.China 6Beth Israel Deaconess Medical Center, Harvard, Boston, MA, USA 7Interdisciplinary Institute of Indian system of Medicine (IIISM), SRM University, Chennai, Tamil Nadu, India 8MacMaster University, Hamilton, ON, Canada 9Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda MD, USA 10Department of Molecular Genetics and Microbiology, University of Florida, Gainesville, FL, USA 11Cloud Pharmaceuticals, Durham, North Carolina, USA 12Division of Rheumatology, University of Florida, -

Adaptive Evolution and Divergence of SERPINB3: a Young Duplicate in Great Apes
Adaptive Evolution and Divergence of SERPINB3: A Young Duplicate in Great Apes Sı´lvia Gomes1*, Patrı´cia I. Marques1,2, Rune Matthiesen3, Susana Seixas1* 1 Institute of Molecular Pathology and Immunology of the University of Porto (IPATIMUP), Porto, Portugal, 2 Institute of Biomedical Sciences Abel Salazar (ICBAS), University of Porto, Porto, Portugal, 3 National Health Institute Doutor Ricardo Jorge (INSA), Lisboa, Portugal Abstract A series of duplication events led to an expansion of clade B Serine Protease Inhibitors (SERPIN), currently displaying a large repertoire of functions in vertebrates. Accordingly, the recent duplicates SERPINB3 and B4 located in human 18q21.3 SERPIN cluster control the activity of different cysteine and serine proteases, respectively. Here, we aim to assess SERPINB3 and B4 coevolution with their target proteases in order to understand the evolutionary forces shaping the accelerated divergence of these duplicates. Phylogenetic analysis of primate sequences placed the duplication event in a Hominoidae ancestor (,30 Mya) and the emergence of SERPINB3 in Homininae (,9 Mya). We detected evidence of strong positive selection throughout SERPINB4/B3 primate tree and target proteases, cathepsin L2 (CTSL2) and G (CTSG) and chymase (CMA1). Specifically, in the Homininae clade a perfect match was observed between the adaptive evolution of SERPINB3 and cathepsin S (CTSS) and most of sites under positive selection were located at the inhibitor/protease interface. Altogether our results seem to favour a coevolution hypothesis for SERPINB3, CTSS and CTSL2 and for SERPINB4 and CTSG and CMA1.A scenario of an accelerated evolution driven by host-pathogen interactions is also possible since SERPINB3/B4 are potent inhibitors of exogenous proteases, released by infectious agents. -
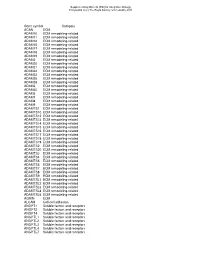
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Nano-Lactoferrin in Diagnostic, Imaging and Targeted Delivery for Cancer and Infectious Diseases Jagat R
cer Scien an ce C & f o T Kanwar et al., J Cancer Sci Ther 2012, 4.3 l h a e n r a Journal of 1000107 r p u DOI: 10.4172/1948-5956. y o J ISSN: 1948-5956 Cancer Science & Therapy Review Article Open Access Nano-Lactoferrin in Diagnostic, Imaging and Targeted Delivery for Cancer and Infectious Diseases Jagat R. Kanwar1*, Rasika M. Samarasinghe1, Rakesh Sehgal2 and Rupinder K. Kanwar1 1Nanomedicine-Laboratory of Immunology and Molecular Biomedical Research (LIMBR), Centre for Biotechnology and Interdisciplinary Biosciences (BioDeakin), Institute for Technology & Research Innovation (ITRI), Deakin University, Geelong, Technology Precinct (GTP), Pigdons Road, Waurn Ponds, Geelong, Victoria 3217, Australia 2Professor, Department of Parasitology, Postgraduate Institute of Medical Education & Research, Chandigarh, India-160012 Abstract Lactoferrin (Lf) is a natural occurring iron binding protein present in many mammalian excretions and involved in various physiological processes. Lf is used in the transport of iron along with other molecules and ions from the digestive system. However its the modulatory functions exhibited by Lf in connection to immune response, disease regression and diagnosis that has made this protein an attractive therapeutic against chronic diseases. Further, the exciting potentials of employing nanotechnology in advancing drug delivery systems, active disease targeting and prognosis have also shown some encouraging outcomes. This review focuses on the role of Lf in diagnosing infection, cancer, neurological and inflammatory diseases and the recent nanotechnology based strategies. Keywords: Lactoferrin; Nanodelivery; Cancer; Inflammation; fluids, mucosal secretions, pancreatic fluids and in neutrophils cells [8]. Infection; Oral administration Structurally, Lf weighs approximately 80kDa and the polypeptide folds into two globular lobes. -

Regulation of Lymphocyte Proliferation by Uterine Serpin: Interleukin-2 Mrna Production, CD25 Expression and Responsiveness to Interleukin-2 (44465) 2 1 MORGAN R
Regulation of Lymphocyte Proliferation by Uterine Serpin: Interleukin-2 mRNA Production, CD25 Expression and Responsiveness to Interleukin-2 (44465) 2 1 MORGAN R. PELTIER,WEN-JUN LIU, AND PETER J. HANSEN Department of Dairy and Poultry Sciences, University of Florida, Gainesville, Florida 32611–0920 Abstract. During pregnancy, the endometrium of the ewe secretes large amounts of a progesterone-induced protein of the serpin superfamily of serine proteinase inhibitors called ovine uterine serpin (OvUS). This protein inhibits lymphocyte proliferation in response to concanavalin A (ConA), phytohemagglutinin (PHA), or mixed lymphocyte reaction. The purpose of these experiments was to characterize the mechanism by which OvUS inhibits lymphocyte proliferation. Ovine US caused dose-dependent in- hibition of lymphocyte proliferation induced by phorbol myristol acetate (PMA), an activator of protein kinase C. The PHA-induced increase in CD25 expression was inhibited in peripheral blood mononuclear leukocytes (PBML) by OvUS. However, no effect of OvUS on Con A-induced expression of CD25 was observed. Further analysis using two-color flow cytometry revealed that OvUS inhibited ConA-induced expres- sion of CD25 in ␥␦-TCR− cells but not ␥␦-TCR+ cells. Stimulation of PBML for 14 hr with ConA resulted in an increase in steady state amounts of interleukin-2 (IL-2) mRNA that was not inhibited by OvUS. Ovine US was also inhibitory to lymphocyte proliferation induced by human IL-2. Results suggest that OvUS acts to inhibit lymphocyte prolif- eration by blocking the upregulation of the IL-2 receptor and inhibiting IL-2–mediated events. Lack of an effect of OvUS on ConA-stimulated CD25 expression in ␥␦-TCR+ cells may reflect a different mechanism of activation of these cells or insensitivity to inhibition by OvUS.