Annual Public Health Statistics 2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
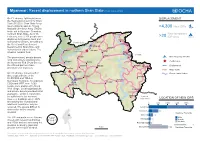
4,300 New Idps >20
Myanmar: Recent displacement in northern Shan State (as of 16 Feb 2016) On 7 February, fighting between DISPLACEMENT the Restoration Council for Shan State (RCSS) / Shan State Army South (SSA-S) and the Ta’ang >4,300 New IDPs National Liberation Army (TNLA) broke out in Kyaukme Township, northern Shan State. As of 16 Monekoe New temporary February, over 3,300 people were >20 IDP sites displaced to Kyaukme town and Konkyan surrounding villages, according to Kachin State Namhkan the Relief and Resettlement Laukkaing Mong Wee Department in Shan State and Tarmoenye humanitarian organizations. The Northern Mabein Lawt Naw Kutkai situation remains fluid. Shan State Hopang Hseni Kunlong CHINA The government, private donors, Manton Pan Lon New tempoary IDP sites local civil society organizations, Mongmit Conflict area the Myanmar Red Cross Society, Namtu the UN and partners have Namhsan Lashio Mongmao Pangwaun Displacement provided relief materials. Tawt San Major roads Mongngawt On 9 February, armed conflict Monglon Rivers / water bodies also erupted between the Hsipaw Namphan RCSS/SSA and TNLA in Kyaukme Tangyan Namhkam Township. According to Mongyai CSOs and WFP, over 1,000 Nawnghkio people were displaced to Mong Wee village. Local organisations Pangsang and private donors provided initial assistance, which is reported to be sufficient for the moment. Matman Eastern However, buildings where IDPs Shan State LOCATION OF NEW IDPS are staying are crowded and 0 500 1000 1500 2000 additional assistance may be required. The area is difficult to Kyaukme 2,400 access due to the security Kho Mone 520 situation. Kyaukme Township Mine Tin 220 The UN and partners are liaising Male closely with relevant authorities Monglon 110 Female No data and CSOs and are assessing the Pain Nal Kon 90 situation to identify gaps and provide further aid if needed. -

Shan State - Myanmar
Myanmar Information Management Unit SHAN STATE - MYANMAR Mohnyin 96°40'E Sinbo 97°30'E 98°20'E 99°10'E 100°0'E 100°50'E 24°45'N 24°45'N Bhutan Dawthponeyan India China Bangladesh Myo Hla Banmauk KACHIN Vietnam Bamaw Laos Airport Bhamo Momauk Indaw Shwegu Lwegel Katha Mansi Thailand Maw Monekoe Hteik Pang Hseng (Kyu Koke) Konkyan Cambodia 24°0'N Muse 24°0'N Muse Manhlyoe (Manhero) Konkyan Namhkan Tigyaing Namhkan Kutkai Laukkaing Laukkaing Mabein Tarmoenye Takaung Kutkai Chinshwehaw CHINA Mabein Kunlong Namtit Hopang Manton Kunlong Hseni Manton Hseni Hopang Pan Lon 23°15'N 23°15'N Mongmit Namtu Lashio Namtu Mongmit Pangwaun Namhsan Lashio Airport Namhsan Mongmao Mongmao Lashio Thabeikkyin Mogoke Pangwaun Monglon Mongngawt Tangyan Man Kan Kyaukme Namphan Hsipaw Singu Kyaukme Narphan Mongyai Tangyan 22°30'N 22°30'N Mongyai Pangsang Wetlet Nawnghkio Wein Nawnghkio Madaya Hsipaw Pangsang Mongpauk Mandalay CityPyinoolwin Matman Mandalay Anisakan Mongyang Chanmyathazi Ai Airport Kyethi Monghsu Sagaing Kyethi Matman Mongyang Myitnge Tada-U SHAN Monghsu Mongkhet 21°45'N MANDALAY Mongkaing Mongsan 21°45'N Sintgaing Mongkhet Mongla (Hmonesan) Mandalay Mongnawng Intaw international A Kyaukse Mongkaung Mongla Lawksawk Myittha Mongyawng Mongping Tontar Mongyu Kar Li Kunhing Kengtung Laihka Ywangan Lawksawk Kentung Laihka Kunhing Airport Mongyawng Ywangan Mongping Wundwin Kho Lam Pindaya Hopong Pinlon 21°0'N Pindaya 21°0'N Loilen Monghpyak Loilen Nansang Meiktila Taunggyi Monghpyak Thazi Kenglat Nansang Nansang Airport Heho Taunggyi Airport Ayetharyar -

Early Childhood Care and Development- END of PROGRAMME EVALUATION !
early childhood care and Development- END OF PROGRAMME EVALUATION ! Table of Contents Acronyms and Abbreviations!..................................................................................................................................................!5! Tables and figures!.....................................................................................................................................................................!6! 1.! EXECUTIVE SUMMARY – CONCLUSIONS AND RECOMMENDATIONS!.........................!7! 2. INTRODUCTION – ORGANIZATIONAL AND PROGRAMMATIC RELEVANCE!............!14! 3. METHODOLOGY!......................................................................................................................................!15! 3.1 ! INTRODUCTION!.....................................................................................................................................................!15! 3.2 ! DATA TOOLS AND DESIGN PROCESS!...............................................................................................................!16! 3.3 ! SAMPLE AND SAMPLE SELECTION!....................................................................................................................!17! 3.4 ! FIELD RESEARCH AND DATA COLLECTION!...................................................................................................!18! 3.5 ! LIMITATIONS!..........................................................................................................................................................!18! -
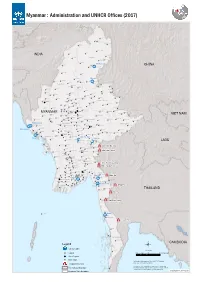
Myanmar : Administration and UNHCR Offices (2017)
Myanmar : Administration and UNHCR Offices (2017) Nawngmun Puta-O Machanbaw Khaunglanhpu Nanyun Sumprabum Lahe Tanai INDIA Tsawlaw Hkamti Kachin Chipwi Injangyang Hpakan Myitkyina Lay Shi Myitkyina CHINA Mogaung Waingmaw Homalin Mohnyin Banmauk Bhamo Paungbyin Bhamo Tamu Indaw Shwegu Momauk Pinlebu Katha Sagaing Mansi Muse Wuntho Konkyan Kawlin Tigyaing Namhkan Tonzang Mawlaik Laukkaing Mabein Kutkai Hopang Tedim Kyunhla Hseni Manton Kunlong Kale Kalewa Kanbalu Mongmit Namtu Taze Mogoke Namhsan Lashio Mongmao Falam Mingin Thabeikkyin Ye-U Khin-U Shan (North) ThantlangHakha Tabayin Hsipaw Namphan ShweboSingu Kyaukme Tangyan Kani Budalin Mongyai Wetlet Nawnghkio Ayadaw Gangaw Madaya Pangsang Chin Yinmabin Monywa Pyinoolwin Salingyi Matman Pale MyinmuNgazunSagaing Kyethi Monghsu Chaung-U Mongyang MYANMAR Myaung Tada-U Mongkhet Tilin Yesagyo Matupi Myaing Sintgaing Kyaukse Mongkaung VIET NAM Mongla Pauk MyingyanNatogyi Myittha Mindat Pakokku Mongping Paletwa Taungtha Shan (South) Laihka Kunhing Kengtung Kanpetlet Nyaung-U Saw Ywangan Lawksawk Mongyawng MahlaingWundwin Buthidaung Mandalay Seikphyu Pindaya Loilen Shan (East) Buthidaung Kyauktaw Chauk Kyaukpadaung MeiktilaThazi Taunggyi Hopong Nansang Monghpyak Maungdaw Kalaw Nyaungshwe Mrauk-U Salin Pyawbwe Maungdaw Mongnai Monghsat Sidoktaya Yamethin Tachileik Minbya Pwintbyu Magway Langkho Mongpan Mongton Natmauk Mawkmai Sittwe Magway Myothit Tatkon Pinlaung Hsihseng Ngape Minbu Taungdwingyi Rakhine Minhla Nay Pyi Taw Sittwe Ann Loikaw Sinbaungwe Pyinma!^na Nay Pyi Taw City Loikaw LAOS Lewe -

Mandalay, Pathein and Mawlamyine - Mandalay, Pathein and Mawlamyine
Urban Development Plan Development Urban The Republic of the Union of Myanmar Ministry of Construction for Regional Cities The Republic of the Union of Myanmar Urban Development Plan for Regional Cities - Mawlamyine and Pathein Mandalay, - Mandalay, Pathein and Mawlamyine - - - REPORT FINAL Data Collection Survey on Urban Development Planning for Regional Cities FINAL REPORT <SUMMARY> August 2016 SUMMARY JICA Study Team: Nippon Koei Co., Ltd. Nine Steps Corporation International Development Center of Japan Inc. 2016 August JICA 1R JR 16-048 Location業務対象地域 Map Pannandin 凡例Legend / Legend � Nawngmun 州都The Capital / Regional City Capitalof Region/State Puta-O Pansaung Machanbaw � その他都市Other City and / O therTown Town Khaunglanhpu Nanyun Don Hee 道路Road / Road � Shin Bway Yang � 海岸線Coast Line / Coast Line Sumprabum Tanai Lahe タウンシップ境Township Bou nd/ Townshipary Boundary Tsawlaw Hkamti ディストリクト境District Boundary / District Boundary INDIA Htan Par Kway � Kachinhin Chipwi Injangyang 管区境Region/S / Statetate/Regi Boundaryon Boundary Hpakan Pang War Kamaing � 国境International / International Boundary Boundary Lay Shi � Myitkyina Sadung Kan Paik Ti � � Mogaung WaingmawミッチMyitkyina� ーナ Mo Paing Lut � Hopin � Homalin Mohnyin Sinbo � Shwe Pyi Aye � Dawthponeyan � CHINA Myothit � Myo Hla Banmauk � BANGLADESH Paungbyin Bhamo Tamu Indaw Shwegu Katha Momauk Lwegel � Pinlebu Monekoe Maw Hteik Mansi � � Muse�Pang Hseng (Kyu Koke) Cikha Wuntho �Manhlyoe (Manhero) � Namhkan Konkyan Kawlin Khampat Tigyaing � Laukkaing Mawlaik Tonzang Tarmoenye Takaung � Mabein -

Dry Zone and South East Region - Myanmar
Myanmar Information Management Unit Dry Zone and South East Region - Myanmar !( !( !( !( Manhlyoe Muse (Manhero) !( !( Cikha Wuntho !( !( Namhkan Konkyan !( !( Khampat Kawlin !( !( Tigyaing !( Laukkaing !( Mawlaik Tonzang !( !( Tarmoenye !( BHUTAN Takaung !( Mabein Chinshwehaw Namtit Kutkai !( !( !( Kachin !( Hopang INDIA Kunlong!( State Tedim !( Rihkhawdar !( !( Kyunhla Hseni !( !( CHINA Manton Pan Lon !( !( Sagaing Kale Kalewa Kanbalu Region !( !( !( Mongmit !( Namtu Ü Taze !( Kanbalu Pangwaun INDIA !( Namhsan Mongmao Chin Shan Taze Lashio !( !( State State Falam !( Mogoke !( Mandalay !( Mingin Thabeikkyin !( Region !( !( Ye-U Rakhine Magway Monglon State Ye-U Khin-U !( Mongngawt Region !( !( Khin-U !( CHINA LAOS Thantlang Tabayin Man Kan Kayah !( Hakha !( !( State Tabayin Kyauk Hsipaw Namphan Bago .! Myaung !( Shwebo !( !( Region SAGAING Shwebo Singu !( !( Kyaukme REGION !( Tangyan !( THAILAND Ayeyarwady Yangon Kayin Kani Mongyai State !( Budalin !( Region Region !( Budalin Wetlet Ayadaw !( Nawnghkio !( Wein Ayadaw !( !( Wetlet Mon State Madaya Gangaw !( Pangsang !( !( Monywa Yinmabin Tanintharyi !( Monywa Rezua !( Yinmabin Mandalay Region !( Sagaing City Pyinoolwin Mongpauk Salingyi Myinmu !( !( Pale !( Chaung-U .! Matman Pale !( Myinmu Kyethi !( !( Monghsu Chaung-U !( Ngazun Sagaing !( Salingyi !( !( BANGLADESH Myaung ! Myitnge Mongyang . !( !( !( !( Tada-U Ngazun CHIN Monghsu Mongkhet Myaung Sintgaing !( STATE Tilin Tada-U !( Mongkaing Kyethi Mongsan Mongla !( (Hmonesan) Mongnawng !( Myaing Yesagyo Intaw !( !( Matupi Kyaukse Kyaukse -

The 2015 General Election in Myanmar: What Now for Ethnic Politics?
MYANMAR POLICY BRIEFING | 17 | December 2015 The 2015 General Election in Myanmar: What Now for Ethnic Politics? KEY POINTS • The victory of the National League for Democracy (NLD) in the 2015 elections was a resounding mandate for democratic change after decades of military-dominated government. • The scale of the victory in ethnic nationality communities across the country highlighted the hopes of all Myanmar’s peoples for the NLD to help achieve a new era of peace and democracy. Both domestic and international expectations are now high, and the incoming government will enjoy initial goodwill. • Formidable challenges remain in key aspects of social and political life. These include transition from military-backed government, political reform and the agreement of a nationwide ceasefire that includes all groups and regions of the country. • Despite the NLD’s success, concerns remain among different nationalities that, unless the NLD pioneers a political breakthrough, conflict and the marginalisation of minority peoples will continue. The perception is widespread that the present structures of national politics and Myanmar’s “first-past-the-post” electoral system do not guarantee the equitable representation of all nationality groups. • In the coming months, the successful transition to a new era of democratic governance and the agreement of an inclusive nationwide ceasefire could provide the best opportunity for ethnic peace and deep-rooted reform in many decades. It is vital that the different sides work cooperatively together rather than seek self- advantage. ideas into movement Introduction After over half a century of military-dominated government, the peoples of Myanmar are Despite huge challenges, election day in Myanmar entering uncharted waters. -

Humanitarian Impact of Landmines in Burma/Myanmar
Humanitarian Impact of Landmines in Burma/Myanmar report prepared by Geneva Call with technical assistance from DCA Mine Action 2011 COVER PHOTO - FREE BURMA RANGERS INSIDE PHOTOS - DCA Humanitarian Impact of Landmines in Burma/Myanmar 2011 TABLE of CONTENTS • Executive Summary 3 • List of Acronyms 4 • Names of Burma/Myanmar States and Divisions 5 • Acknowledgements 6 1. Introduction and Methodology 7 2. Background and Context 9 History of Landmine Use 9 Affected Areas 9 Affected Communities 12 Affected People 14 3. Mine Action in Burma 16 Victim Assistance 19 Mine Risk Education 21 Advocacy against Landmines 22 Mine Clearance 24 4. Potential Mine Action Providers 26 UN Mine Action Agencies, INGOs, National Authorities 26 NSAs and NSA-linked CBOs, National and Local NGOs, National Faith-Based Organizations, Civil Society Organizations, Media in Buma/Myanmar 27 5. Conclusion 28 6. Recommendations 29 7. Appendices 32 2 EXECUTIVE SUMMARY Humanitarian Impact of Landmines in Burma/Myanmar While the existing data available on landmine victims China are also mined, and mine accidents have indicate that Burma/Myanmar1 faces one of the most occurred there. An estimated five million people severe landmine problems in the world today, little is live in townships that contain mine-contaminated known about the actual extent of the problem, the areas, and are in need of Mine Risk Education (MRE) impact on affected populations, communities’ mine to reduce risky behaviour, and victim assistance for action needs and how different actors can become those already injured. more involved in mine action. With estimates of mine victim numbers still unclear The Government of Burma/Myanmar has prohibited due to a lack of reliable data, the report finds that almost all forms of mine action with the exception of a significant proportion of the children affected in a limited amount of prosthetic assistance to people landmine accidents in NSA areas are child soldiers. -

Countdown to the Myanmar Elections Prepared for the Conflict Prevention and Peace Forum by Richard Horsey 1 25 August 2010
Countdown to the Myanmar Elections Prepared for the Conflict Prevention and Peace Forum by Richard Horsey 1 25 August 2010 I. The election timetable On 13 August, the Myanmar Election Commission finally announced the timetable for the country’s first elections in two decades; two days earlier, it had designated the constituencies. 2 The key dates are as follows: 11 August Constituencies designated by Election Commission 16 – 30 August Registration period for candidates (party and independent) 3 September Deadline for candidates to withdraw 6 – 10 September Applications scrutinized by Election Commission 7 November Election Day The announcement gave parties little more than two weeks’ notice of the candidate registration deadline – although most parties had already been considering for some time the question of which constituencies they would contest, and identifying possible candidates. The limited time remaining, and the considerable costs associated with contesting a seat (a non-refundable US$500 fee per candidate), mean that a number of parties have to scale-back their ambitions. With 498 seats up for grabs at the national level, and a further 665 in regional legislatures, only highly-organized and well-funded parties can hope to contest a majority of seats. Although parties have already started their canvassing activities, the campaign period proper – when confirmed candidates can formally seek support from the electorate in their constituency – will last only two months. By way of comparison, the timetable for the 1990 elections was announced more than six months in advance, on 7 November 1989. 3 Then too, however, little 1 Richard Horsey is an independent political analyst and a former ILO liaison officer in Myanmar; he is fluent in the Burmese language. -

Malteser Activities in Shan Special Region
Myanmar Information Management Unit Malteser Activities in Shan Special Region !( !( 97°20'E !( 98°0'E 98°40'E 99°20'E 100°0'E Mansi Maw !( Pang Hseng Monekoe !( Hteik (Kyu Koke) ns !( !( CHINA MANSI Manhlyoe Muse !( (Manhero) Shan State (North) !( MUSE KONKYAN Ü Namhkan !( Konkyan !( Mandalay Shan State (East) 23°45'N 23°45'N NAMHKAN Laukkaing Shan State (South) !( LAUKKAING LAOS Tarmoenye !( KUTKAI THAILAND Kayah Nam!( Tit !( Kutkai !( Hopang Kunlong !( !( CHINA KUNLONG MANTON Hseni !( Pan Lon HSENI !( HOPANG Nar Wee 23°10'N Gaung Gi 23°10'N (Na Wi) !( Hsawng Hpa Namtu !( + + (Saun Pha) NAMTU !( Pangwaun !( Hkun Mar Yawng (Hkwin Ma) Mong Maw !( Lashio ns!( Lin !( !( Man Tun !( MONGMAO Long PANGWAUN Htan !( LASHIO Aik Chan Lin Haw !( (Ai' Chun) !( Ka Lawng nsAik Chan Hpar !( Man Kan !( Yin Pang !( Hsipaw !( Namphan!z!( TANGYAN NAMPHAN 22°35'N 22°35'N Man Man Hseng Tangyan !( C"¢!( Nam Hkam Wu Nawng !( Hkit !( Mongyai !( !z Nar PANGSANG MONGYAI Kawng !z!( Wein!= HSIPAW Nam Phat !( !( Pang Yang C!("¢ Ho Tawng Ton Hpa ( Ho Tao) !( !z Mong Mongpauk!z!( Hpen !( ¢ 22°0'N C" Mong Hpen 22°0'N Matman !( !¹ Nam Mong Tai MONGYANG Kyethi !( Nam Hpai !( Monghsu !( MATMAN Mongyang KYETHI Mong Kar !( !( MONGHSU Mongkhet !( MONGKAUNG Mongsan MONGKHET (Hmonesan) Mongla !( Mongnawng !( !( Mongkaung !( MONGLA 21°25'N 21°25'N Mongping !( Tontar !( Mongyu !( Kunhing Kar Li !( !( Kengtung LAIHKA !(®v Laihka !( MONGYAWNG KUNHING KENGTUNG MONGPING Mongyawng !( Kho Lam !( Pinlon !( LOILEN MONGHPYAK Loilen !( Nansang !( Monghpyak !( NANSANG Kenglat !( 20°50'N -

Burma (Myanmar) 2020 Crime & Safety Report
Burma (Myanmar) 2020 Crime & Safety Report This is an annual report produced in conjunction with the Regional Security Office at the U.S. Embassy in Rangoon (Yangon). OSAC encourages travelers to use this report to gain baseline knowledge of security conditions in Burma (Myanmar). For more in-depth information, review OSAC’s Burma country page for original OSAC reporting, consular messages, and contact information, some of which may be available only to private-sector representatives with an OSAC password. Travel Advisory The current U.S. Department of State Travel Advisory at the date of this report’s publication assesses Burma at Level 2, indicating travelers should exercise increased caution due to areas of civil unrest and armed conflict. Do not travel to: • Buthidaung, Kyauktaw, Maungdaw, Minbya, Mrauk- U, Ponnagyun, and Rathedaung townships in Rakhine State due to civil unrest and armed conflict. • Paletwa township in Chin State due to civil unrest and armed conflict • Hpakan, Momauk, Sumprabum, Tanai, and Waingmaw townships in Kachin State due to civil unrest and armed conflict. • Hpapun township in Kayin State due to civil unrest. • Hseni, Hsipaw, Konkyan, Kutkai, Kyaukme, Laukkaing, Matman, Mongmao, Muse, Namphan, Namtu, Pangsang, and Pangwaun townships in Shan State due to civil unrest and armed conflict. Reconsider travel to: • Ann, and Myebon townships in Rakhine State due to civil unrest and armed conflict. • Matupi township in Chin State due to civil unrest. • Bhamo, Mansi, and Mogaung townships in Kachin State due to civil unrest. • Hopang, Lashio, Mongkaung, Namhsan, Nanhkan townships in Shan State due to civil unrest. • Lashio township in Shan State due to civil unrest. -

Shan State REDD+ Action Plan, Myanmar
FOREST Action Pl D+ an 2 ED 01 R 8, te M ta y S a n n m a h a r S S Prepared by Forest Research Institute (FRI) Myanmar Report preparation team FRI Thaung Naing Oo, Director Inkyin Khaine, Assistant Director Nay Aung, Range Officer ICIMOD Nabin Bhattarai, Forest Land Restoration and REDD+ Research Associate Bhaskar Singh Karky, Programme Coordinator, REDD+ Initiative GIZ Kai Windhorst, CTA Copyright © 2019 Forest Department, Ministry of Natural Resources and Environmental Conservation, Myanmar This work is licensed under a Creative Commons Attribution Non-Commercial, No Derivatives 4.0 International License (https://creativecommons.org/licenses/by-nc-nd/4.0/). Published by Forest Research Institute (FRI), Forest Department, Ministry of Natural Resources and Environmental Conservation, Myanmar Production team Shanuj VC (Consultant editor) Samuel Thomas (Senior editor) Rachana Chettri (Editor) Dharma Ratna Maharjan (Graphic designer) Photos: Deependra Tandukar, Bandana Shakya, Yi Shaoliang Printed and bound in Nepal by Quality Printers Pvt. Ltd., Kathmandu, Nepal Citation: FRI (2019). Shan State REDD+ Action Plan, Myanmar. FRI: Myanmar. FOREST Shan State REDD+ Action Plan, Myanmar 2019 Prepared by Forest Research Institute (FRI), Myanmar Contents Message iv Acknowledgments v Acronyms and abbreviations vi Introduction 1 Myanmar’s national REDD+ strategy 1 Evolution of SRAP in Myanmar 2 Linking Myanmar’s NDCs and SRAP 2 Shan State 3 Contextual background 3 Geography 3 Administrative divisions 3 Land cover change assessment 4 Methodology and