16118909.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Cellular Retinaldehyde-Binding Protein Has Secondary Thermal 9-Cis-Retinal Isomerase Activity
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/259313787 Human Cellular Retinaldehyde-Binding Protein Has Secondary Thermal 9-cis-Retinal Isomerase Activity Article in Journal of the American Chemical Society · January 2014 DOI: 10.1021/ja411366w · Source: PubMed CITATIONS READS 6 123 12 authors, including: Christin Bolze Rachel E. Helbling Vifor Pharma 13 PUBLICATIONS 21 CITATIONS 3 PUBLICATIONS 13 CITATIONS SEE PROFILE SEE PROFILE Arwen Pearson Guillaume Pompidor University of Hamburg European Molecular Biology Laboratory 78 PUBLICATIONS 1,083 CITATIONS 37 PUBLICATIONS 286 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Melanopsin View project AdPLA LRAT View project All content following this page was uploaded by Achim Stocker on 10 November 2017. The user has requested enhancement of the downloaded file. Article pubs.acs.org/JACS Human Cellular Retinaldehyde-Binding Protein Has Secondary Thermal 9-cis-Retinal Isomerase Activity † ‡ † § ∥ ⊥ ∇ Christin S. Bolze, , Rachel E. Helbling, Robin L. Owen, Arwen R. Pearson, Guillaume Pompidor, , ⊥ ⊥ ○ † # # Florian Dworkowski, Martin R. Fuchs, , Julien Furrer, Marcin Golczak, Krzysztof Palczewski, † † Michele Cascella,*, and Achim Stocker*, † ‡ Department of Chemistry and Biochemistry, and Graduate School for Cellular and Biomedical Sciences, University of Bern, Freiestrasse 3, 3012 Bern, Switzerland § Diamond Light Source, Harwell Science and Innovation Campus, -

Shedding New Light on the Generation of the Visual Chromophore PERSPECTIVE Krzysztof Palczewskia,B,C,1 and Philip D
PERSPECTIVE Shedding new light on the generation of the visual chromophore PERSPECTIVE Krzysztof Palczewskia,b,c,1 and Philip D. Kiserb,d Edited by Jeremy Nathans, Johns Hopkins University School of Medicine, Baltimore, MD, and approved July 9, 2020 (received for review May 16, 2020) The visual phototransduction cascade begins with a cis–trans photoisomerization of a retinylidene chro- mophore associated with the visual pigments of rod and cone photoreceptors. Visual opsins release their all-trans-retinal chromophore following photoactivation, which necessitates the existence of pathways that produce 11-cis-retinal for continued formation of visual pigments and sustained vision. Proteins in the retinal pigment epithelium (RPE), a cell layer adjacent to the photoreceptor outer segments, form the well- established “dark” regeneration pathway known as the classical visual cycle. This pathway is sufficient to maintain continuous rod function and support cone photoreceptors as well although its throughput has to be augmented by additional mechanism(s) to maintain pigment levels in the face of high rates of photon capture. Recent studies indicate that the classical visual cycle works together with light-dependent pro- cesses in both the RPE and neural retina to ensure adequate 11-cis-retinal production under natural illu- minances that can span ten orders of magnitude. Further elucidation of the interplay between these complementary systems is fundamental to understanding how cone-mediated vision is sustained in vivo. Here, we describe recent -

JMSCR Vol||08||Issue||02||Page 208-210||February 2020
JMSCR Vol||08||Issue||02||Page 208-210||February 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i2.40 Keratomalacia - A Case Report Authors Deepthi Pullepu1*, Deepthi Janga2, V Murali Krishna3 *Corresponding Author Deepthi Pullepu Department of Ophthalmology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Abstract Xerophthalmia refers to an ocular condition of destructive dryness of conjunctiva and cornea caused due to severe vitamin A deficiency. Usually affects infants, children and women of reproductive age group. It is estimated to affect about one-third of children under the age of five around the world. Keratomalacia means dry and cloudy cornea which melts and perforates, caused due to severe vitamin A deficiency. Here we describe a case of 21 year old female with neurofibromatosis type 1 presenting with keratomalacia. Keywords: Vitamin A deficiency, Xerophthalmia, Keratomalacia. Introduction blindness is a significant contributor Vitamin A is essential for the functioning of the In India, it is estimated that there are immune system, healthy growth and development approximately 6.8 million people who have vision of body and is usually acquired through diet. less than 6/60 in at least one eye due to corneal Globally, 190 million children under five years of diseases; of these, about a million have bilateral age are affected by vitamin A deficiency involvement. They suffer from an increased risk of visual Corneal blindness resulting due to this disease can impairment, illness and death from childhood be completely prevented by institution of effective infections such as measles and those causing preventive or prophylactic measures at the diarrhoea community level. -

Abstract: a 19 Year Old Male Was Diagnosed with Vitamin a Deficiency
Robert Adam Young Abstract: A 19 year old male was diagnosed with vitamin A deficiency (VAD). Clinical examination shows conjunctival changes with central and marginal corneal ulcers. Patient history and lab testing were used to confirm the diagnosis. I. Case History 19 year old Hispanic Male Presents with chief complaint of progressive blur at distance and near in both eyes, foreign body sensation, ocular pain, photophobia, and epiphora; signs/symptoms are worse in the morning upon wakening. Started 6 months to 1 year ago, and has progressively gotten worse. Patient reports that the right eye is worse than the left eye. Ocular history of Ocular Rosacea Medical history of Hypoaldosteronism, Pernicious Anemia, and Type 2 Polyglandular Autoimmune Syndrome Last eye examination was two weeks ago at a medical center Presenting topical/systemic medications - Tobramycin TID OU, Prednisolone Acetate QD OU (has used for two weeks); Fludrocortisone (used long-term per PCP) Other pertinent info includes reports that patient cannot gain weight, although he has a regular appetite. Patient presents looking very slim, malnourished, and undersized for his age. II. Pertinent findings Entering unaided acuities are 20/400 OD with no improvement with pinhole; 20/50 OS that improves to 20/25 with pinhole. Pupil testing shows (-)APD; Pupils are 6mm in dim light, and constrict to 4mm in bright light. Ocular motilities are full and smooth with no reports of diplopia or pain. Tonometry was performed with tonopen and revealed intraocular pressures of 12 mmHg OD and 11 mmHG OS. Slit lamp examination shows 2+ conjunctival injection with trace-mild bitot spots both nasal and temporal, OU. -

Current Health Issues in the Caribbean BLINDNESS in THE
Current Health Issues in the Caribbean BLINDNESS IN THE CARIBBEAN Alfred L. Anduze, M.D. St. Croix Vision Center St. Croix Hospital St. Croix U.S. Virgin Islands Caribbean Studies Association Merida, Mexico May 26, 1994 Abstract: Blindness in the Caribbean Background: The prevailing of blindness in the Caribbean region are reviewed in the context of world blindness statistics to identify differences and similarities that might exist. Method: A review of the status of blindness in the U.S. Virgin Islands, Barbados, Jamaica, Puerto Rico, Trinidad, and Mexico; individually with regard to causal etiology, epidemiology, treatment and possible future research. Results: Blindness in the Caribbean is the result of genetics, tropical environment and cultural habits of the inhabitants and consist of Age-related macular disease, Infectious diseases, Diabetes mellitus, Glaucoma, Congenital defects, Xerophthalmia, Trachoma, Trauma and Cataracts. Conclusion: There are almost 50 million people who are legally blind worldwide (i.e. with a vision of 20/200 or less) 2-3 million in the Caribbean region. The social and economic consequences are serious additional deterrents in developing countries. Outline: Causes of Blindness in the Caribbean I. Age-related macular disease a. Vascular insufficiency b. Senile macular degeneration II. Cataracts III. Glaucoma IV. Diabetes mellitus V. Infectious diseases a. Trachoma b. Onchocerciasis c. Leprosy d. Toxoplasmosis e. Toxocariasis f. AIDS VI. Trauma a. industrial/work-related b. sports c. home accidents VII. Nutritional a. Xerophthalmia/keratomalacia b. Iron-deficiency anemia c. Tobacco/Alcohol Retinopathy VIII. Congenital defects a. genetic syndromes b. strabismus Legal blindness is acceptably defined as vision 20/200 (6/60) or less. -

(10) Patent No.: US 8119385 B2
US008119385B2 (12) United States Patent (10) Patent No.: US 8,119,385 B2 Mathur et al. (45) Date of Patent: Feb. 21, 2012 (54) NUCLEICACIDS AND PROTEINS AND (52) U.S. Cl. ........................................ 435/212:530/350 METHODS FOR MAKING AND USING THEMI (58) Field of Classification Search ........................ None (75) Inventors: Eric J. Mathur, San Diego, CA (US); See application file for complete search history. Cathy Chang, San Diego, CA (US) (56) References Cited (73) Assignee: BP Corporation North America Inc., Houston, TX (US) OTHER PUBLICATIONS c Mount, Bioinformatics, Cold Spring Harbor Press, Cold Spring Har (*) Notice: Subject to any disclaimer, the term of this bor New York, 2001, pp. 382-393.* patent is extended or adjusted under 35 Spencer et al., “Whole-Genome Sequence Variation among Multiple U.S.C. 154(b) by 689 days. Isolates of Pseudomonas aeruginosa” J. Bacteriol. (2003) 185: 1316 1325. (21) Appl. No.: 11/817,403 Database Sequence GenBank Accession No. BZ569932 Dec. 17. 1-1. 2002. (22) PCT Fled: Mar. 3, 2006 Omiecinski et al., “Epoxide Hydrolase-Polymorphism and role in (86). PCT No.: PCT/US2OO6/OOT642 toxicology” Toxicol. Lett. (2000) 1.12: 365-370. S371 (c)(1), * cited by examiner (2), (4) Date: May 7, 2008 Primary Examiner — James Martinell (87) PCT Pub. No.: WO2006/096527 (74) Attorney, Agent, or Firm — Kalim S. Fuzail PCT Pub. Date: Sep. 14, 2006 (57) ABSTRACT (65) Prior Publication Data The invention provides polypeptides, including enzymes, structural proteins and binding proteins, polynucleotides US 201O/OO11456A1 Jan. 14, 2010 encoding these polypeptides, and methods of making and using these polynucleotides and polypeptides. -
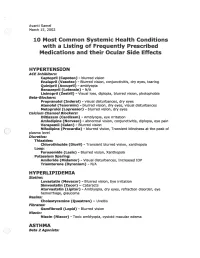
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

© Alan Macfarlane and Gerry Martin, 2002 1 MYOPIA: ITS
© Alan Macfarlane and Gerry Martin, 2002 MYOPIA: ITS COMPARATIVE INCIDENCE AND PROBABLE CAUSES What Rasmussen encountered in his many years of working with Chinese eye problem astonished him. He summarized his impressions thus. 'Three facts stand out clearly in both ancient and modern records of Chinese eyesight: one that they are a highly myopic nation; two that keratomalacia is the major cause of ocular disease; and three that presbyopia is earlier than in the West by about five years. They stand out against an historical background of neglect and abuse, malnutrition, and centuries of State indifference.' (p.48) Moving on to the statistics of myopia, he summarized the research of a quarter of a century by saying that 'only 20 per cent. of all lenses supplied by the ancients, and similar amount by the moderns (excluding high astigmatic) were for old-sight lenses. It is the other 80 per cent. that matters; the 65 per cent. for myopia and the 15 per cent. for glare and therapeutics.' (p.20) Elsewhere he gives slightly different statistics, which applied to those aged under forty years, showed that approximately 75 per cent. of the lenses were supplied for myopia. In a detailed table he presents the figures; in the 'Ancient Chinese Sight Records', 65% were for myopia; in the 'Modern Chinese Sight Records' myopia (simple) or with astigmatism combined accounted for 70% of the lenses.(p.48) The second figure of 70% was based on 120,000 case histories collected by Rasmussen and his colleagues over a period of 25 years. (p.49) The significance of the degree of myopia only comes out if we compare the Chinese figures with those for other nationalities. -

The Main Causes of Blindness and Low Vision in School for Blind
26ORIGINAL ARTICLE DOI 10.5935/0034-7280.20160006 The main causes of blindness and low vision in school for blind As principais causas de cegueira e baixa visão em escola para deficientes visuais Abelardo Couto Junior1, Lucas Azeredo Gonçalves de Oliveira2 ABSTRACT Objective: Identify and analyze the main causes of blindness and low vision in school for blind. Methods: One hundred sixty-five medical records of visually impaired students were reviewed in an institution specialized in teaching the blind, treated between august 2013 and may 2014. The variables analyzed were age, sex, visual acuity, primary and secondary diagnoses, treatment, optical prescription features and prognosis. Results: 165 students were evaluated, 91 students (55%) are legally blind and only 74 (45%) of the students are classified as low vision. The main causes of blindness were: retinopathy of prematurity (21%), optic nerve atrophy (18%), congenital glaucoma (16%), retinal dystrophy (11%) and cancer (8%). The causes of low vision were: congenital cataract (18%), congenital glaucoma (15%) and retinochoroidal scarring (12%). Conclusion: The main causes of blindness and low vision in the Benjamin Constant Institute are from preventable diseases. Keywords: Blindness; Low vision; Visual acuity; Child; Health school RESUMO Objetivo: Identificar e analisar as principais causas de cegueira e baixa visão em escola para deficientes visuais. Métodos: Foram revisados 165 prontuários de alunos portadores de deficiência visual em instituição especializada no ensino de cegos, atendidos no período de agosto de 2013 a maio de 2014. As variáveis analisadas foram: idade, gênero, acuidade visual, diagnóstico principal e secundário, tratamento, recursos ópticos prescritos e prognóstico. Resultados: Dos 165 alunos avaliados, 91 alunos (55%) são legalmente cegos e apenas 74 (45%) dos alunos são enquadrados como baixa visão. -

Ophthaproblem
Pratique clinique Clinical Pract ice Ophthaproblem Shaun Segal Sanjay Sharma, MD, MSC, MBA, FRCSC : Ophthalmic Photography : Ophthalmic Photography Photo credit Photo Dieu Hotel University, Laboratory of Queen’s Kingston, Ont. Hospital, 30-year-old woman had been admitted to hospital in infancy with diarrhea, steatorrhea, and failure to thrive. During late childhood, she developed atypi- Acal retinitis pigmentosa involving the retina and a progressive ataxic neuropathy. Investigations showed her serum lacked beta-lipoprotein and her red corpuscles had a spiky shape. Recent ophthalmic examination revealed substantial choroidal atrophy around the disk and a speckled peripheral fundus. Which vitamins should this patient be given as therapy for her disorder? 1. Vitamin A 2. Vitamin E 3. Vitamin C 4. Vitamin B Answer on page 1085 Mr Segal is a medical student at Queen’s University in Kingston, Ont. Dr Sharma is an Associate Professor of Ophthalmology and an Assistant Professor of Epidemiology at Queen’s University VOL 5: AUGUST • AOÛT 2005 d Canadian Family Physician • Le Médecin de famille canadien 1079 Pratique clinique Clinical Pract ice Answer to Ophthaproblem continued from page 1079 1. Vitamin A and 2. vitamin E Th is patient has abetalipoproteinemia (ABL), some- times called Bassen-Kornzweig syndrome,1 a dis- ease characterized by malabsorption of fat. The condition is treated with supplements of the two fat-soluble vitamins A and E. Abetalipoproteinemia manifests itself through signs of lipid malabsorp- tion, dense contracted red blood -

Prevalence and Causes of Low Vision and Blindness Worldwide
S Afr Optom 2005 64 (2) 44 − 54 Prevalence and causes of low vision and blindness worldwide AO Oduntan* Department of Optometry, University of Limpopo, Private Bag X1106, Sovenga, 0727 South Africa <[email protected]> Abstract Introduction A recent review of the causes and prevalence There are many low vision and blind people of low vision and blindness world wide is lack- worldwide, and there is a considerable amount of ing. Such review is important for highlighting data available on the prevalence of low vision and the causes and prevalence of visual impairment blindness in many parts of the world. The data, in the different parts of the world. Also, it is however, vary significantly from one continent to important in providing information on the types another. In 1995, the World Health Organization and magnitude of eye care programs needed in (WHO) Task Force on data on blindness estimated different parts of the world. In this article, the that there were 37.1 million blind people world- causes and prevalence of low vision and blind- wide, indicating a global prevalence of 0.7 percent1. ness in different parts of the world are reviewed According to that report, the prevalence values and the socio-economic and psychological range from 0.3% in the developed countries to implications are briefly discussed. The review 1.4% in Sub-Saharan African countries. The preva- is based on an extensive review of the litera- lence of visual impairment is expected to be higher ture using computer data bases combined with in the developing countries due to the low level of review of available national, regional and inter- health care services in many of the countries. -

PDF Hosted at the Radboud Repository of the Radboud University Nijmegen
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/30002 Please be advised that this information was generated on 2021-10-03 and may be subject to change. of Sharola Dharmaraj amaurosis analysis and congenital Clinical molecular Leber Clinical and molecular analysis of Leber congenital amaurosis Sharola Dharmaraj Clinical and molecular analysis of Leber congenital amaurosis Sharola Dharmaraj SSharolaharola BBW.inddW.indd 1 229-May-079-May-07 110:45:200:45:20 AAMM Clinical and molecular analysis of Leber congenital amaurosis PhD thesis Radboud University Nijmegen Medical Centre Sharola Dharmaraj ISBN: 978-90-9021-989-9 © 2007 S. Dharmaraj All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, by print or otherwise, without permission in writing from the author. Cover image: Fundus in LCA5-associated LCA (K.Klima) Print and layout by: Optima Grafi sche Communicatie, Rotterdam SSharolaharola BBW.inddW.indd 2 229-May-079-May-07 110:45:220:45:22 AAMM Clinical and molecular analysis of Leber congenital amaurosis Een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad van doctor aan de Radboud Universiteit Nijmegen op gezag van de rector magnifi cus prof. mr. S.C.J.J Kortmann, volgens besluit van het College van Decanen in het openbaar te verdedigen op maandag 2 juli 2007 om 13.30 uur precies door Sharola Dharmaraj geboren op 11 december 1961 te India SSharolaharola BBW.inddW.indd 3 229-May-079-May-07 110:45:220:45:22 AAMM Promotor: Prof.