Committee for Veterinary Medicinal Products
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy and Tolerability of Quinacrine Monotherapy and Albendazole Plus Chloroquine Combination Therapy in Nitroimidazole-Refractory Giardiasis: a Tropnet Study
Klinik für Infektiologie & Spitalhygiene Efficacy and tolerability of quinacrine monotherapy and albendazole plus chloroquine combination therapy in nitroimidazole-refractory giardiasis: a TropNet study Andreas Neumayr, Mirjam Schunk, Caroline Theunissen, Marjan Van Esbroeck, Matthieu Mechain, Manuel Jesús Soriano Pérez, Kristine Mørch, Peter Sothmann, Esther Künzli, Camilla Rothe, Emmanuel Bottieau Journal Club 01.03.21 Andreas Neumayr Background on giardia treatment: • 1st-line treatment: 5-nitroimidazoles: metronidazole (1957), tinidazole, ornidazole, secnidazole • cure rate of 5NIs in 1st-line treatment: ~90% • in the last decade, an increase of 5NI-refractory giardia cases has been observed in travel medicine clinics across Europe: Hospital for Tropical Diseases, London: 2008: 15% --> 2013: 40% 70% of 5NI-refractory cases imported from India • 2nd-line treatment: effectiveness of a 2nd round with a 5NI: ~17% alternative drugs: albendazole, mebendazole, nitazoxanide, quinacrine, furazolidone, chloroquine, paromomycin 2012 TropNet member survey: 53 centres use 39 different treatment regimens, consisting of 7 different drugs in mono- or combination-therapy in various dosages and durations JC 01.03.21 Nabarro LE et al. Clin Microbiol Infect. 2015;21:791-6. • by 2013, there were only 13 reports of 2nd-line therapy for giardiasis (8 case series, 5 individual case reports): n=110 Cure rates Albendazole 6/32 18.7% Paromomycin 5/17 29.4% Nitazoxanide 2/5 40.0% Albendazole + 5-NI 42/53 79.2% Quinacrine 19/21 90.5% Quinacrine + 5-NI 14/14 100% Quinacrine + Paromomycin 2/2 100% • 2013: TropNet "GiardiaREF" study kick-off: Study on efficacy and tolerability of two 2nd-line regimens in nitroimidazole-refractory giardiasis: Quinacrine JC 01.03.21 Meltzer E et al. -

Jos Journal 2
POST-OPERATIVE AUDIT OF G6PD-DEFICIENT MALE CHILDREN WITH OBSTRUCTIVE ADENOTONSILLAR ENLARGEMENT AT UNIVERSITY COLLEGE HOSPITAL, IBADAN, NIGERIA. John EN1, Totyen EL1, Jacob N2, Nwaorgu OGB1 1 .Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria 2. Department of paediatrics, University College Hospital, Ibadan, Nigeria All correspondences and request for reprint to Dr John EN, Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria Email: [email protected] Telephone: +2348036240109 Abstract Background: G6PD deficiency ranks among the commonest hereditary enzyme deficiency worldwide and notable as a predisposing condition to haemolyticcrises. The fear of possible untoward effects is often expressed by parents of G6PD deficient male children scheduled for surgery after obtaining an informed and understood consent. The parental perception of obstructive adenotonsillar enlargement in this condition was also appraised. Methods: A retrospective chart review of all G6PD deficient male children between ages 1 to 7years who had adenotonsillectomy over a 3year period at University college Hospital, Ibadan, Nigeria. Results: The patients comprised of 22 G6PD deficient male children diagnosed shortly after birth upon development of neonatal jaundice. Fifteen(68.2%) and 6(27.3%) of the patients subsequently developed episodes of drug- induced haemolysis and non-haemolytic drug reactions prior to undergoing adenotonsillectomy by the otolaryngologists. None of the patients was observed to develop haemolytic crises up to 2weeks post-adenotonsillectomy. From the parental perception and responses in the follow-up period,all 22(100%) patient had resolution of noisy breathing, 20(91%) had improvement of snoring and apnoeic spells. Only 15 (68%) were reported to stop mouth-breathing. -

Annex 4: Drug Dosages for Children (Formulary)
Medicines Dosage Form Dose according to body weight (calculate if weight is below or over) 3-6 kg 6-10 kg 10-15 kg 15-20 kg 20-29 kg albendazole 200 mg (half tablet) 12-24 months chewable tablet, 400mg 400 mg (one tablet) over 24 months amodiaquine 10 mg base/kg/3 days (total dose 30 mg base/kg) tablet, 200mg - - 1 1 1 amoxicillin 15 mg/kg/dose for 7 days tablet/capsule 250 mg ¼ ½ ¾ 1 1½ oral suspension, 125mg/5ml 2.5 ml 5 ml 7.5 ml 10 ml - non-severe pneumonia: 25 mg/kg 2 times per day for 3 days tablet/capsule 250 mg ½ 1 1½ 2 2½ oral suspension, 125mg/5ml 5 ml 10 ml 15 ml - - ampicillin IM 50 mg/kg/6 hours Vial of 500 mg mixed with 2.1 ml 1 ml 2 ml 3 ml 5 ml 6 ml sterile water to give 500 mg/2.5 ml artemether IM 3.2 mg/kg once on day 1 injection, 40mg/ml in 1ml ampoule then injection, 80mg/ml in 1ml ampoule see Chapter 5, management of the child with malaria IM 1.6 mg/kg daily until oral therapy is possible, total therapy one week artemether + fixed dose treatment (20+120 mg) twice daily for 3 days tablet 10+120 mg see Chapter 5, management of the child with malaria lumefantrine artesunate severe malaria: IV or IM 2.4 mg/kg over 3 minutes at 0, 12 and 24 vial of 60 mg in 0.6 ml with 3.4 ml hours on day 1. -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -
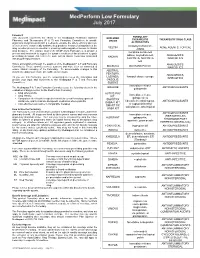
Medperform Low Formulary July 2017
MedPerform Low Formulary July 2017 Foreword FORMULARY This document represents the efforts of the MedImpact Healthcare Systems EXCLUDED THERAPEUTIC THERAPEUTIC DRUG CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide DRUGS physicians and pharmacists with a method to evaluate the safety, efficacy and cost- ALTERNATIVES effectiveness of commercially available drug products. A structured approach to the clindamycin/tretinoin, VELTIN ACNE AGENTS, TOPICAL drug selection process is essential in ensuring continuing patient access to rational ZIANA drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ER, ANALGESICS, prescribing decisions that reflect the most current clinical consensus associated KADIAN with drug therapy decisions. NUCYNTA, NUCYNTA NARCOTICS ER This is accomplished through the auspices of the MedImpact P & T and Formulary ANALGESICS, BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, ANALGESICS, LAZANDA, fentanyl citrate lozenge As you use this Formulary, you are encouraged to review the information and NARCOTICS provide your input and comments to the MedImpact P & T and Formulary ONSOLIS, Committees. SUBSYS immediate-release GRALISE ANTICONVULSANTS The MedImpact -

New Zealand Data Sheet
1 PARNATE tranylcypromine film-coated tablets 10 mg New Zealand Data Sheet 1 PARNATE® (10 MG FILM-COATED TABLETS) PARNATE 10 mg film-coated tablets. 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Parnate 10 mg film-coated tablets: each tablet contains tranylcypromine sulfate equivalent to 10 mg of tranylcypromine. Excipients with known effect: each tablet contains sucrose 6 mg. For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Parnate 10 mg film-coated tablets contain "geranium rose" coloured, biconvex, film-coated tablets. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Parnate is indicated for the treatment of symptoms of depressive illness especially where treatment with other types of anti-depressants has failed. It is not recommended for use in mild depressive states resulting from temporary situational difficulties. 4.2 Dose and method of administration Adults Begin with 20 mg a day given as 10 mg in the morning and 10 mg in the afternoon. If there is no satisfactory response after two weeks, add one more tablet at midday. Continue this dosage for at least a week. A dosage of 3 tablets a day should only be exceeded with caution. When a satisfactory response is established, dosage may be reduced to a maintenance level. Some patients will be maintained on 20 mg per day, some will need only 10 mg daily. If no improvement occurs, continued administration is unlikely to be beneficial. 1 2 PARNATE tranylcypromine film-coated tablets 10 mg When given together with a tranquilliser, the dosage of Parnate is not affected. When the medicine is given concurrently with electroconvulsive therapy, the recommended dosage is 10 mg twice a day during the series and 10 mg a day afterwards as maintenance therapy. -

Furazolidone Drug Information, Professional 7/8/18 19:50
Furazolidone Drug Information, Professional 7/8/18 19:50 Furazolidone (Oral-Local) VA CLASSIFICATION Primary: AM600 Secondary: AP109 Commonly used brand name(s): Furoxone; Furoxone Liquid. Note: For a listing of dosage forms and brand names by country availability, see Dosage Forms section(s). †Not commercially available in Canada. Category: Antibacterial (oral-local)— antiprotozoal— Note: Furazolidone is a broad-spectrum anti-infective that is effective against most gastrointestinal tract pathogens. {01} Indications Accepted Cholera (treatment)—Furazolidone is indicated as a secondary agent in the treatment of cholera caused by Vibrio cholerae (V. comma) . {01} {02} {03} {04} {05} {07} {09} {15} {18} {19} Diarrhea, bacterial (treatment)—Furazolidone is indicated as a secondary agent in the treatment of bacterial diarrhea caused by susceptible organisms. Furazolidone is active in vitro against Campylobacter jejuni, Enterobacter aerogenes, Escherichia coli, Proteus species, Salmonella species, Shigella species, and staphylococci. However, clinical studies on the effectiveness of furazolidone in some types of bacterial diarrhea have been inconclusive or conflicting. {01} {02} {25} {26} https://www.drugs.com/mmx/furazolidone.html Página 1 de 12 Furazolidone Drug Information, Professional 7/8/18 19:50 Giardiasis (treatment)—Furazolidone is indicated as a secondary agent in the treatment of giardiasis caused by Giardia lamblia . {01} {02} {03} {04} {05} {06} {07} {08} {09} {13} {14} {16} —Not all species or strains of a particular organism may be susceptible to furazolidone. Pharmacology/Pharmacokinetics Physicochemical characteristics: Molecular weight— 225.16 {10} Mechanism of action/Effect: Microbicidal. Furazolidone interferes with several bacterial enzyme systems. It neither significantly alters normal bowel flora nor results in fungal overgrowth. -

National Treatment Guidelines for Antimicrobial Use in Infectious Diseases
National Treatment Guidelines for Antimicrobial Use in Infectious Diseases Version 1.0 (2016) NATIONAL CENTRE FOR DISEASE CONTROL Directorate General of Health Services Ministry of Health & Family Welfare Government of India CONTENTS Chapter 1 .................................................................................................................................................................................................................. 7 Introduction ........................................................................................................................................................................................................ 7 Chapter 2. ................................................................................................................................................................................................................. 9 Syndromic Approach For Empirical Therapy Of Common Infections.......................................................................................................... 9 A. Gastrointestinal & Intra-Abdominal Infections ......................................................................................................................................... 10 B. Central Nervous System Infections ........................................................................................................................................................... 13 C. Cardiovascular Infections ......................................................................................................................................................................... -

Parasitic Infections (1 of 14)
Parasitic Infections (1 of 14) 1 Patient presents w/ signs & symptoms suggestive of GI parasitic infection 2 DIAGNOSIS No ALTERNATIVE Is a GI parasitic infection DIAGNOSIS confi rmed? Yes Protozoal or helminthic infection? Protozoal Infection Helminthic Infection A Rehydration & nutrition B Prevention PHARMACOLOGICAL PHARMACOLOGICAL THERAPY FOR THERAPY FOR PROTOZOAL HELMINTHIC INFECTIONS INFECTIONS ©See page 3 MIMSSee page 3 B1 © MIMS 2019 Parasitic Infections (2 of 14) 1 SIGNS & SYMPTOMS OF GI PARASITIC INFECTIONS GI Symptoms • Abdominal pain, diarrhea, dysentery, fl atulence, malabsorption, symptoms of biliary obstruction Nonspecifi c Symptoms • Fever, malaise, fatigue, anorexia, sweating, wt loss, edema & pruritus • Some patients may be asymptomatic PARASITIC INFECTIONS PARASITIC 2 DIAGNOSIS Clinical History • Attempt to elicit a history of possible exposure, especially for helminthic infections, eg eating undercooked meat, source of drinking water, swimming in fresh water where certain parasites may be endemic • Knowledge of the geographic distribution of parasites is helpful in the diagnosis of patients Host Susceptibility Factors in GI Parasitic Infections • Nutritional status • Intercurrent disease • Pregnancy • Immunosuppressive drugs • Presence of a malignancy Physical Exam Findings • Pallor • Hepatomegaly • Ascites • Ileus • Rectal prolapse Lab Tests Microscopic Exam of Stools • Fundamental to the diagnosis of all GI infections - A minimum of 3 stool specimens, examined by trained personnel using a concentration & a permanent stain -

Pdf/Medeff/Bulletin/Carn-Bcei V22n2-Eng.Pdf
NEWSLETTER The Official Journal of the Anesthesia Patient Safety Foundation www.apsf.org Volume 30, No.1, 1-16 Circulation 118,032 June 2015 What is Your MH IQ ? by Charles B, Watson, MD, FCCM, and Barbara W. Brandom, MD Question Your Understanding remain unreported, they do provide a profile of metabolic monitors are important in the immedi- 14 of MH: events that take place, and there is no evidence to ate postoperative period as well. suggest a decrease in MH-related death or compli- The anesthesia community has the best under- cations. The most recent review of MH Registry 3. MH is very rare—there is one standing of Malignant Hyperthermia [MH] data shows an increased, rather than decreased, causative genetic mutation because it is a genetically determined illness that is number of deaths reported.3 most often recognized during or immediately after associated with MH anesthesia with the potent inhalational agents In addition, there has been skepticism that suc- susceptibility. and/or administration of succinylcholine. More- cinylcholine, alone, causes MH crisis in susceptible 4,5 FALSE—Depending on the population over, a specific antidote for the MH crisis has been individuals. Older data from the MH registry and newer data from the Canadian MH experience in reviewed, MH crisis has been reported with an available since the late 1970s, dantrolene sodium. incidence ranging from 1:8,000 to 1:30,000 anes- recent years clearly show that MH crisis can be Now dantrolene and other necessary elements thetics. Quarterly reviews of calls to the MH Hot- induced by succinylcholine administration, needed for emergency treatment of an MH epi- line [800-MH-HYPER] made when a caller alone.4,6-8 Succinylcholine induced muscle contrac- sode are immediately available to anesthesia staff suspects MH show that around 30% are MH crisis at most hospital and outpatient anesthetizing ture of patients and swine shown susceptible to MH while most represent other acute processes. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Pharmacogenomic Associations Tables
Pharmacogenomic Associations Tables Disclaimer: This is educational material intended for health care professionals. This list is not comprehensive for all of the drugs in the pharmacopeia but focuses on commonly used drugs with high levels of evidence that the CYPs (CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4 and CYP3A5 only) and other select genes are relevant to a given drug’s metabolism. If a drug is not listed, there is not enough evidence for inclusion at this time. Other CYPs and other genes not described here may also be relevant but are out of scope for this document. This educational material is not intended to supersede the care provider’s experience and knowledge of her or his patient to establish a diagnosis or a treatment plan. All medications require careful clinical monitoring regardless of the information presented here. Table of Contents Table 1: Substrates of Cytochrome P450 (CYP) Enzymes Table 2: Inhibitors of Cytochrome P450 (CYP) Enzymes Table 3: Inducers of Cytochrome P450 (CYP) Enzymes Table 4: Alternate drugs NOT metabolized by CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4 or CYP3A5 enzymes Table 5: Glucose-6-Phosphate Dehydrogenase (G6PD) Associated Drugs and Compounds Table 6: Additional Pharmacogenomic Genes & Associated Drugs Table 1: Substrates of Cytochrome P450 (CYP) Enzymes Allergy Labetalol CYP2C19 Immunosuppressives Loratadine CYP3A4 Lidocaine CYP1A2 CYP2D6 Cyclosporine CYP3A4/5 Analgesic/Anesthesiology CYP3A4/5 Sirolimus CYP3A4/5 Losartan CYP2C9 CYP3A4/5 Codeine CYP2D6 activates Tacrolimus CYP3A4/5 Lovastatin