Annex 4: Drug Dosages for Children (Formulary)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin Lisa Pasierb
Duquesne University Duquesne Scholarship Collection Electronic Theses and Dissertations Fall 2005 The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin Lisa Pasierb Follow this and additional works at: https://dsc.duq.edu/etd Recommended Citation Pasierb, L. (2005). The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin (Doctoral dissertation, Duquesne University). Retrieved from https://dsc.duq.edu/etd/1021 This Immediate Access is brought to you for free and open access by Duquesne Scholarship Collection. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Duquesne Scholarship Collection. For more information, please contact [email protected]. The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin A Dissertation presented to the Bayer School of Natural and Environmental Sciences of Duquesne University As partial fulfillment of the requirements for the degree of Doctor of Philosophy By Lisa Pasierb August 26, 2005 Dr. David Seybert, thesis director Dr. David W. Wright, advisor In memory of Anna Pasierb April 24, 1924 – May 31, 2005 ii Acknowledgements First and foremost, I would like to express my sincerest gratitude to my advisor, Dr. David W. Wright. His exuberating energy and conviction attracted me to his research group, while his unwavering faith in me taught me more than he could ever know. Secondly, of course, I would like to extend my appreciation to Glenn Spreitzer and James Ziegler, the other two original members of the Wright group, whom initially tried to exert male dominance, but eventually became very faithful friends and colleagues. Finally, to all the other members of the Wright group over the years, thanks for all of your help, suggestions, and camaraderie. -

WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 498/04 (2006.01) A61K 31/5365 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 519/00 (2006.01) A61P 25/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, (21) Number: International Application DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/IB20 17/050844 HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KH, KN, (22) International Filing Date: KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, 15 February 2017 (15.02.2017) MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, (25) Filing Language: English RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, (26) Publication Language: English TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 62/298,657 23 February 2016 (23.02.2016) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: PFIZER INC. [US/US]; 235 East 42nd Street, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, New York, New York 10017 (US). -

Dalbavancin • Oritavancin • Tedizolid • Ceftolozane/Tazobactam • Ceftazidime/Avibactam • Fecal Transplant
What’s New in Infectious Diseases? Bruce L. Gilliam, M.D. Institute of Human Virology University of Maryland School of Medicine Baltimore, MD Topics New Antibacterial Therapeutics Emerging Pathogens HIV Hepatitis C Disclosures Research Studies Pfizer – Staph aureus Vaccine Trial TaiMed Biologics - Ibaluzimab Advisory Board Viiv Healthcare New Antibacterial Therapeutics • Dalbavancin • Oritavancin • Tedizolid • Ceftolozane/tazobactam • Ceftazidime/avibactam • Fecal Transplant Incidence of Staph aureus hospitalizations in U.S.A., 2001–2009 BMC Infect Dis 2014, 14:296 Dalbavancin (Dalvance) • Derived from Teicoplanin • ½ life – Effective: 8.5 days – Terminal: 346 hrs (14 days) • Bactericidal • Similar spectrum to Vancomycin, active against: – Staphylococci • MSSA, MRSA, CoNS – Streptococci • resistant pneumococci • anaerobic strep – Enterococci • VRE with van B, C but not A – Corynebacterium Dalbavancin Once Weekly Non- Inferior to Vanco/Linezolid N Engl J Med 2014;370:2169-79. Single-Dose (1.5 g) Non-Inferior to Weekly Dalbavancin for Treatment of Acute Bacterial Skin and Skin Structure Infection 100 90 80 70 60 50 Single Dose 40 Once Weekly 30 20 10 0 Overall Clinical Success Rate Success Rate Success Rate Response Day 14 Day 28 Day 14 MRSA Clin Infect Dis. 2015 Nov 26. pii: civ982. [Epub ahead of print] VA Experience with Dalbavancin • Background – Levels in bone > MIC for 14 days • 8 patients treated for osteomyelitis with IV Dalbavancin – Former IV drug users not eligible for home IV or unwilling to do home IV • Treated for up to 8 weeks • No adverse events • All with resolution of osteomyelitis • Cost savings vs. placement in facility Oritavancin (Orbactiv) • Derived from Vancomycin • ½ life – Terminal 245-393 hrs (10-16 days) • Bactericidal • Similar spectrum to Vancomycin, active against: – Staphylococci • MSSA, MRSA, CoNS – Streptococci • resistant pneumococci • anaerobic strep – Enterococci • VRE with van A, B, C – Corynebacterium Single Dose Oritavancin vs. -

Efficacy and Tolerability of Quinacrine Monotherapy and Albendazole Plus Chloroquine Combination Therapy in Nitroimidazole-Refractory Giardiasis: a Tropnet Study
Klinik für Infektiologie & Spitalhygiene Efficacy and tolerability of quinacrine monotherapy and albendazole plus chloroquine combination therapy in nitroimidazole-refractory giardiasis: a TropNet study Andreas Neumayr, Mirjam Schunk, Caroline Theunissen, Marjan Van Esbroeck, Matthieu Mechain, Manuel Jesús Soriano Pérez, Kristine Mørch, Peter Sothmann, Esther Künzli, Camilla Rothe, Emmanuel Bottieau Journal Club 01.03.21 Andreas Neumayr Background on giardia treatment: • 1st-line treatment: 5-nitroimidazoles: metronidazole (1957), tinidazole, ornidazole, secnidazole • cure rate of 5NIs in 1st-line treatment: ~90% • in the last decade, an increase of 5NI-refractory giardia cases has been observed in travel medicine clinics across Europe: Hospital for Tropical Diseases, London: 2008: 15% --> 2013: 40% 70% of 5NI-refractory cases imported from India • 2nd-line treatment: effectiveness of a 2nd round with a 5NI: ~17% alternative drugs: albendazole, mebendazole, nitazoxanide, quinacrine, furazolidone, chloroquine, paromomycin 2012 TropNet member survey: 53 centres use 39 different treatment regimens, consisting of 7 different drugs in mono- or combination-therapy in various dosages and durations JC 01.03.21 Nabarro LE et al. Clin Microbiol Infect. 2015;21:791-6. • by 2013, there were only 13 reports of 2nd-line therapy for giardiasis (8 case series, 5 individual case reports): n=110 Cure rates Albendazole 6/32 18.7% Paromomycin 5/17 29.4% Nitazoxanide 2/5 40.0% Albendazole + 5-NI 42/53 79.2% Quinacrine 19/21 90.5% Quinacrine + 5-NI 14/14 100% Quinacrine + Paromomycin 2/2 100% • 2013: TropNet "GiardiaREF" study kick-off: Study on efficacy and tolerability of two 2nd-line regimens in nitroimidazole-refractory giardiasis: Quinacrine JC 01.03.21 Meltzer E et al. -

Jos Journal 2
POST-OPERATIVE AUDIT OF G6PD-DEFICIENT MALE CHILDREN WITH OBSTRUCTIVE ADENOTONSILLAR ENLARGEMENT AT UNIVERSITY COLLEGE HOSPITAL, IBADAN, NIGERIA. John EN1, Totyen EL1, Jacob N2, Nwaorgu OGB1 1 .Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria 2. Department of paediatrics, University College Hospital, Ibadan, Nigeria All correspondences and request for reprint to Dr John EN, Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria Email: [email protected] Telephone: +2348036240109 Abstract Background: G6PD deficiency ranks among the commonest hereditary enzyme deficiency worldwide and notable as a predisposing condition to haemolyticcrises. The fear of possible untoward effects is often expressed by parents of G6PD deficient male children scheduled for surgery after obtaining an informed and understood consent. The parental perception of obstructive adenotonsillar enlargement in this condition was also appraised. Methods: A retrospective chart review of all G6PD deficient male children between ages 1 to 7years who had adenotonsillectomy over a 3year period at University college Hospital, Ibadan, Nigeria. Results: The patients comprised of 22 G6PD deficient male children diagnosed shortly after birth upon development of neonatal jaundice. Fifteen(68.2%) and 6(27.3%) of the patients subsequently developed episodes of drug- induced haemolysis and non-haemolytic drug reactions prior to undergoing adenotonsillectomy by the otolaryngologists. None of the patients was observed to develop haemolytic crises up to 2weeks post-adenotonsillectomy. From the parental perception and responses in the follow-up period,all 22(100%) patient had resolution of noisy breathing, 20(91%) had improvement of snoring and apnoeic spells. Only 15 (68%) were reported to stop mouth-breathing. -

Cytochrome P450 Oxidative Metabolism: Contributions to the Pharmacokinetics, Safety, and Efficacy of Xenobiotics
1521-009X/44/8/1229–1245$25.00 http://dx.doi.org/10.1124/dmd.116.071753 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:1229–1245, August 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Special Section on Emerging Novel Enzyme Pathways in Drug Metabolism—Commentary Cytochrome P450 and Non–Cytochrome P450 Oxidative Metabolism: Contributions to the Pharmacokinetics, Safety, and Efficacy of Xenobiotics Robert S. Foti and Deepak K. Dalvie Pharmacokinetics and Drug Metabolism, Amgen, Cambridge, Massachusetts (R.S.F.); and Pharmacokinetics, Dynamics, and Metabolism, Pfizer, La Jolla, California (D.K.D.) Downloaded from Received May 24, 2016; accepted June 10, 2016 ABSTRACT The drug-metabolizing enzymes that contribute to the metabolism this end, this Special Section on Emerging Novel Enzyme Pathways or bioactivation of a drug play a crucial role in defining the in Drug Metabolism will highlight a number of advancements that dmd.aspetjournals.org absorption, distribution, metabolism, and excretion properties of have recently been reported. The included articles support the that drug. Although the overall effect of the cytochrome P450 (P450) important role of non-P450 enzymes in the clearance pathways of family of drug-metabolizing enzymes in this capacity cannot be U.S. Food and Drug Administration–approved drugs over the past understated, advancements in the field of non-P450–mediated me- 10 years. Specific examples will detail recent reports of aldehyde tabolism have garnered increasing attention in recent years. This is oxidase, flavin-containing monooxygenase, and other non-P450 perhaps a direct result of our ability to systematically avoid P450 pathways that contribute to the metabolic, pharmacokinetic, or liabilities by introducing chemical moieties that are not susceptible pharmacodynamic properties of xenobiotic compounds. -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -
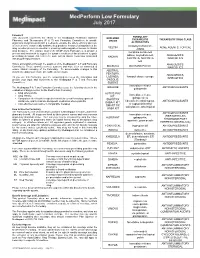
Medperform Low Formulary July 2017
MedPerform Low Formulary July 2017 Foreword FORMULARY This document represents the efforts of the MedImpact Healthcare Systems EXCLUDED THERAPEUTIC THERAPEUTIC DRUG CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide DRUGS physicians and pharmacists with a method to evaluate the safety, efficacy and cost- ALTERNATIVES effectiveness of commercially available drug products. A structured approach to the clindamycin/tretinoin, VELTIN ACNE AGENTS, TOPICAL drug selection process is essential in ensuring continuing patient access to rational ZIANA drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ER, ANALGESICS, prescribing decisions that reflect the most current clinical consensus associated KADIAN with drug therapy decisions. NUCYNTA, NUCYNTA NARCOTICS ER This is accomplished through the auspices of the MedImpact P & T and Formulary ANALGESICS, BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, ANALGESICS, LAZANDA, fentanyl citrate lozenge As you use this Formulary, you are encouraged to review the information and NARCOTICS provide your input and comments to the MedImpact P & T and Formulary ONSOLIS, Committees. SUBSYS immediate-release GRALISE ANTICONVULSANTS The MedImpact -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Efficacy and Safety of Methylene Blue in the Treatment of Malaria: a Systematic Review G
Lu et al. BMC Medicine (2018) 16:59 https://doi.org/10.1186/s12916-018-1045-3 RESEARCH ARTICLE Open Access Efficacy and safety of methylene blue in the treatment of malaria: a systematic review G. Lu1,2, M. Nagbanshi2, N. Goldau2, M. Mendes Jorge2, P. Meissner3, A. Jahn2, F. P. Mockenhaupt4 and O. Müller2* Abstract Background: Methylene blue (MB) was the first synthetic antimalarial to be discovered and was used during the late 19th and early 20th centuries against all types of malaria. MB has been shown to be effective in inhibiting Plasmodium falciparum in culture, in the mouse model and in rhesus monkeys. MB was also shown to have a potent ex vivo activity against drug-resistant isolates of P. falciparum and P. vivax. In preclinical studies, MB acted synergistically with artemisinin derivates and demonstrated a strong effect on gametocyte reduction in P. falciparum. MB has, thus, been considered a potentially useful partner drug for artemisinin-based combination therapy (ACT), particularly when elimination is the final goal. The aim of this study was to review the scientific literature published until early 2017 to summarise existing knowledge on the efficacy and safety of MB in the treatment of malaria. Methods: This systematic review followed PRISMA guidelines. Studies reporting on the efficacy and safety of MB were systematically searched for in relevant electronic databases according to a pre-designed search strategy. The search (without language restrictions) was limited to studies of humans published until February 2017. Results: Out of 474 studies retrieved, a total of 22 articles reporting on 21 studies were eligible for analysis. -

Application for Inclusion of Artesunate/Amodiaquine Fixed Dose Combination Tablets in the Who Model Lists of Essential Medicines
SANOFI-AVENTIS artesunate/amodiaquine Application for inclusion in the WHO Model Lists of essential medicines June 2009- updated Sept. 2010 APPLICATION FOR INCLUSION OF ARTESUNATE/AMODIAQUINE FIXED DOSE COMBINATION TABLETS IN THE WHO MODEL LISTS OF ESSENTIAL MEDICINES Artesunate / Amodiaquine, Fixed dose combination 1/57 25 mg/ 67.5 mg, 50 mg/ 135 mg and 100 mg/270 mg SANOFI-AVENTIS artesunate/amodiaquine Application for inclusion in the WHO Model Lists of essential medicines June 2009- updated Sept. 2010 TABLE OF CONTENT 1. Summary statement of the proposal for inclusion p.4 2. Name of the focal point in WHO submitting or supporting the p.9 Application 3. Name of the organisation(s) consulted and/or supporting the p.10 Application 4. International Non-proprietary Name (INN, generic name) of p.10 the medicine 5. Dosage form or strength proposed for inclusion p.10 5.1. Chemical characteristics p.10 5.2. The formulation proposed for inclusion p.11 5.3. Stability of the formulation p.14 6. International availability – sources, if possible manufacturers p.14 6.1. Sources and manufacturers p.14 6.2. History of the product p.15 6.3. International availability and production capacity p.16 7. Whether listing is requested as an individual medicine or as an p.17 example of a group 8. Information supporting the public health relevance p.18 (epidemiological information on disease burden, assessment of current use, target population) 9. Treatment details p.22 9.1. Method of administration p.22 9.2. Dosage p.22 9.3. Duration p.22 9.4. -

Methylene Blue for the Treatment of Health Conditions: a Scoping Review
Vol.64: e21200266, 2021 https://doi.org/10.1590/1678-4324-20212002660266 ISSN 1678-4324 Online Edition Review - Human and Animal Health Methylene Blue for the Treatment of Health Conditions: a Scoping Review Jessica Galvan1* Luciane Patrícia Andreani Cabral2 https://orcid.org/0000-0002-3261-8521 https://orcid.org/0000-0001-9424-7431 Mariana Xavier Borsoi1 Marcos Cezar Pomini3 https://orcid.org/0000-0003-4940-8149 https://orcid.org/0000-0001-8129-7165 Luciana Julek1 Fabiana Bucholdz Teixeira Alves2 https://orcid.org/0000-0001-6898-6839 https://orcid.org/0000-0001-9955-1811 Danielle Bordin2 https://orcid.org/0000-0001-7861-0384 1Campos Gerais Regional University Hospital (HURCG), State University of Ponta Grossa (UEPG), Department of Nursing and Health Public, Ponta Grossa, Paraná, Brazil; 2State University of Ponta Grossa (UEPG), Ponta Grossa, Paraná, Brazil. 3Piracicaba Dental School, University of Campinas (UNICAMP), Campinas, São Paulo, Brazil. Editor-in-Chief: Paulo Vitor Farago Associate Editor: Paulo Vitor Farago Received: 2020.05.03; Accepted: 2020.09.10. *Correspondence: [email protected]; Tel.: +55-44-99980-7290 (J.G.). HIGHLIGHTS This scoping review summarizes the findings of clinical trials using methylene blue (MB) for the treatment of various health conditions. This research method allowed mapping main findings, clarifying research topics, and identifying gaps in the literature. Abstract: studies evaluating effective drugs for health conditions are of crucial importance for public health. Methylene blue (MB) is an accessible synthetic drug that presents low toxicity and has been used in several health areas due to its effectiveness. Objective: this scoping review aims to provide a comprehensive overview of relevant research regarding the use of MB for the treatment of health conditions.