Medical Review(S) Review of Request for Priority Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin Lisa Pasierb
Duquesne University Duquesne Scholarship Collection Electronic Theses and Dissertations Fall 2005 The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin Lisa Pasierb Follow this and additional works at: https://dsc.duq.edu/etd Recommended Citation Pasierb, L. (2005). The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin (Doctoral dissertation, Duquesne University). Retrieved from https://dsc.duq.edu/etd/1021 This Immediate Access is brought to you for free and open access by Duquesne Scholarship Collection. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Duquesne Scholarship Collection. For more information, please contact [email protected]. The Role of Histidine-Rich Proteins in the Biomineralization of Hemozoin A Dissertation presented to the Bayer School of Natural and Environmental Sciences of Duquesne University As partial fulfillment of the requirements for the degree of Doctor of Philosophy By Lisa Pasierb August 26, 2005 Dr. David Seybert, thesis director Dr. David W. Wright, advisor In memory of Anna Pasierb April 24, 1924 – May 31, 2005 ii Acknowledgements First and foremost, I would like to express my sincerest gratitude to my advisor, Dr. David W. Wright. His exuberating energy and conviction attracted me to his research group, while his unwavering faith in me taught me more than he could ever know. Secondly, of course, I would like to extend my appreciation to Glenn Spreitzer and James Ziegler, the other two original members of the Wright group, whom initially tried to exert male dominance, but eventually became very faithful friends and colleagues. Finally, to all the other members of the Wright group over the years, thanks for all of your help, suggestions, and camaraderie. -

WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 498/04 (2006.01) A61K 31/5365 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 519/00 (2006.01) A61P 25/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, (21) Number: International Application DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/IB20 17/050844 HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KH, KN, (22) International Filing Date: KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, 15 February 2017 (15.02.2017) MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, (25) Filing Language: English RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, (26) Publication Language: English TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 62/298,657 23 February 2016 (23.02.2016) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: PFIZER INC. [US/US]; 235 East 42nd Street, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, New York, New York 10017 (US). -

Eurartesim, INN-Piperaquine & INN-Artenimol
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Eurartesim 160 mg/20 mg film-coated tablets. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 160 mg piperaquine tetraphosphate (as the tetrahydrate; PQP) and 20 mg artenimol. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). White oblong biconvex film-coated tablet (dimension 11.5x5.5mm / thickness 4.4mm) with a break-line and marked on one side with the letters “S” and “T”. The tablet can be divided into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Eurartesim is indicated for the treatment of uncomplicated Plasmodium falciparum malaria in adults, adolescents, children and infants 6 months and over and weighing 5 kg or more. Consideration should be given to official guidance on the appropriate use of antimalarial medicinal products, including information on the prevalence of resistance to artenimol/piperaquine in the geographical region where the infection was acquired (see section 4.4). 4.2 Posology and method of administration Posology Eurartesim should be administered over three consecutive days for a total of three doses taken at the same time each day. 2 Dosing should be based on body weight as shown in the table below. Body weight Daily dose (mg) Tablet strength and number of tablets per dose (kg) PQP Artenimol 5 to <7 80 10 ½ x 160 mg / 20 mg tablet 7 to <13 160 20 1 x 160 mg / 20 mg tablet 13 to <24 320 40 1 x 320 mg / 40 mg tablet 24 to <36 640 80 2 x 320 mg / 40 mg tablets 36 to <75 960 120 3 x 320 mg / 40 mg tablets > 75* 1,280 160 4 x 320 mg / 40 mg tablets * see section 5.1 If a patient vomits within 30 minutes of taking Eurartesim, the whole dose should be re-administered; if a patient vomits within 30-60 minutes, half the dose should be re-administered. -

Pharmacological and Cardiovascular Perspectives on the Treatment of COVID-19 with Chloroquine Derivatives
www.nature.com/aps REVIEW ARTICLE Pharmacological and cardiovascular perspectives on the treatment of COVID-19 with chloroquine derivatives Xiao-lei Zhang1, Zhuo-ming Li1, Jian-tao Ye1, Jing Lu1, Lingyu Linda Ye2, Chun-xiang Zhang3, Pei-qing Liu1 and Dayue D Duan2 The novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) causes coronavirus disease 2019 (COVID-19) and an ongoing severe pandemic. Curative drugs specific for COVID-19 are currently lacking. Chloroquine phosphate and its derivative hydroxychloroquine, which have been used in the treatment and prevention of malaria and autoimmune diseases for decades, were found to inhibit SARS-CoV-2 infection with high potency in vitro and have shown clinical and virologic benefits in COVID-19 patients. Therefore, chloroquine phosphate was first used in the treatment of COVID-19 in China. Later, under a limited emergency- use authorization from the FDA, hydroxychloroquine in combination with azithromycin was used to treat COVID-19 patients in the USA, although the mechanisms of the anti-COVID-19 effects remain unclear. Preliminary outcomes from clinical trials in several countries have generated controversial results. The desperation to control the pandemic overrode the concerns regarding the serious adverse effects of chloroquine derivatives and combination drugs, including lethal arrhythmias and cardiomyopathy. The risks of these treatments have become more complex as a result of findings that COVID-19 is actually a multisystem disease. While respiratory symptoms are the major clinical manifestations, cardiovascular abnormalities, including arrhythmias, myocarditis, heart failure, and ischemic stroke, have been reported in a significant number of COVID-19 patients. Patients with preexisting cardiovascular conditions (hypertension, arrhythmias, etc.) are at increased risk of severe COVID-19 and death. -

Dalbavancin • Oritavancin • Tedizolid • Ceftolozane/Tazobactam • Ceftazidime/Avibactam • Fecal Transplant
What’s New in Infectious Diseases? Bruce L. Gilliam, M.D. Institute of Human Virology University of Maryland School of Medicine Baltimore, MD Topics New Antibacterial Therapeutics Emerging Pathogens HIV Hepatitis C Disclosures Research Studies Pfizer – Staph aureus Vaccine Trial TaiMed Biologics - Ibaluzimab Advisory Board Viiv Healthcare New Antibacterial Therapeutics • Dalbavancin • Oritavancin • Tedizolid • Ceftolozane/tazobactam • Ceftazidime/avibactam • Fecal Transplant Incidence of Staph aureus hospitalizations in U.S.A., 2001–2009 BMC Infect Dis 2014, 14:296 Dalbavancin (Dalvance) • Derived from Teicoplanin • ½ life – Effective: 8.5 days – Terminal: 346 hrs (14 days) • Bactericidal • Similar spectrum to Vancomycin, active against: – Staphylococci • MSSA, MRSA, CoNS – Streptococci • resistant pneumococci • anaerobic strep – Enterococci • VRE with van B, C but not A – Corynebacterium Dalbavancin Once Weekly Non- Inferior to Vanco/Linezolid N Engl J Med 2014;370:2169-79. Single-Dose (1.5 g) Non-Inferior to Weekly Dalbavancin for Treatment of Acute Bacterial Skin and Skin Structure Infection 100 90 80 70 60 50 Single Dose 40 Once Weekly 30 20 10 0 Overall Clinical Success Rate Success Rate Success Rate Response Day 14 Day 28 Day 14 MRSA Clin Infect Dis. 2015 Nov 26. pii: civ982. [Epub ahead of print] VA Experience with Dalbavancin • Background – Levels in bone > MIC for 14 days • 8 patients treated for osteomyelitis with IV Dalbavancin – Former IV drug users not eligible for home IV or unwilling to do home IV • Treated for up to 8 weeks • No adverse events • All with resolution of osteomyelitis • Cost savings vs. placement in facility Oritavancin (Orbactiv) • Derived from Vancomycin • ½ life – Terminal 245-393 hrs (10-16 days) • Bactericidal • Similar spectrum to Vancomycin, active against: – Staphylococci • MSSA, MRSA, CoNS – Streptococci • resistant pneumococci • anaerobic strep – Enterococci • VRE with van A, B, C – Corynebacterium Single Dose Oritavancin vs. -

Jos Journal 2
POST-OPERATIVE AUDIT OF G6PD-DEFICIENT MALE CHILDREN WITH OBSTRUCTIVE ADENOTONSILLAR ENLARGEMENT AT UNIVERSITY COLLEGE HOSPITAL, IBADAN, NIGERIA. John EN1, Totyen EL1, Jacob N2, Nwaorgu OGB1 1 .Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria 2. Department of paediatrics, University College Hospital, Ibadan, Nigeria All correspondences and request for reprint to Dr John EN, Department of ENT/Head and Neck Surgery, University College Hospital, Ibadan, Nigeria Email: [email protected] Telephone: +2348036240109 Abstract Background: G6PD deficiency ranks among the commonest hereditary enzyme deficiency worldwide and notable as a predisposing condition to haemolyticcrises. The fear of possible untoward effects is often expressed by parents of G6PD deficient male children scheduled for surgery after obtaining an informed and understood consent. The parental perception of obstructive adenotonsillar enlargement in this condition was also appraised. Methods: A retrospective chart review of all G6PD deficient male children between ages 1 to 7years who had adenotonsillectomy over a 3year period at University college Hospital, Ibadan, Nigeria. Results: The patients comprised of 22 G6PD deficient male children diagnosed shortly after birth upon development of neonatal jaundice. Fifteen(68.2%) and 6(27.3%) of the patients subsequently developed episodes of drug- induced haemolysis and non-haemolytic drug reactions prior to undergoing adenotonsillectomy by the otolaryngologists. None of the patients was observed to develop haemolytic crises up to 2weeks post-adenotonsillectomy. From the parental perception and responses in the follow-up period,all 22(100%) patient had resolution of noisy breathing, 20(91%) had improvement of snoring and apnoeic spells. Only 15 (68%) were reported to stop mouth-breathing. -

Plasmodium Falciparum Clinical Isolates: in Vitro Genotypic and Phenotypic Characterization Nonlawat Boonyalai1* , Brian A
Boonyalai et al. Malar J (2020) 19:269 https://doi.org/10.1186/s12936-020-03339-w Malaria Journal RESEARCH Open Access Piperaquine resistant Cambodian Plasmodium falciparum clinical isolates: in vitro genotypic and phenotypic characterization Nonlawat Boonyalai1* , Brian A. Vesely1, Chatchadaporn Thamnurak1, Chantida Praditpol1, Watcharintorn Fagnark1, Kirakarn Kirativanich1, Piyaporn Saingam1, Chaiyaporn Chaisatit1, Paphavee Lertsethtakarn1, Panita Gosi1, Worachet Kuntawunginn1, Pattaraporn Vanachayangkul1, Michele D. Spring1, Mark M. Fukuda1, Chanthap Lon1, Philip L. Smith2, Norman C. Waters1, David L. Saunders3 and Mariusz Wojnarski1 Abstract Background: High rates of dihydroartemisinin–piperaquine (DHA–PPQ) treatment failures have been documented for uncomplicated Plasmodium falciparum in Cambodia. The genetic markers plasmepsin 2 (pfpm2), exonuclease (pfexo) and chloroquine resistance transporter (pfcrt) genes are associated with PPQ resistance and are used for moni- toring the prevalence of drug resistance and guiding malaria drug treatment policy. Methods: To examine the relative contribution of each marker to PPQ resistance, in vitro culture and the PPQ survival assay were performed on seventeen P. falciparum isolates from northern Cambodia, and the presence of E415G-Exo and pfcrt mutations (T93S, H97Y, F145I, I218F, M343L, C350R, and G353V) as well as pfpm2 copy number polymor- phisms were determined. Parasites were then cloned by limiting dilution and the cloned parasites were tested for drug susceptibility. Isobolographic analysis of several drug combinations for standard clones and newly cloned P. falciparum Cambodian isolates was also determined. Results: The characterization of culture-adapted isolates revealed that the presence of novel pfcrt mutations (T93S, H97Y, F145I, and I218F) with E415G-Exo mutation can confer PPQ-resistance, in the absence of pfpm2 amplifcation. -

Artemisinin Resistance: Current Status and Scenarios for Containment
REVIEWS Artemisinin resistance: current status and scenarios for containment Arjen M. Dondorp*‡, Shunmay Yeung*§, Lisa White*‡, Chea Nguon§, Nicholas P.J. Day*‡, Duong Socheat§|| and Lorenz von Seidlein*¶ Abstract | Artemisinin combination therapies are the first-line treatments for uncomplicated Plasmodium falciparum malaria in most malaria-endemic countries. Recently, partial artemisinin-resistant P. falciparum malaria has emerged on the Cambodia–Thailand border. Exposure of the parasite population to artemisinin monotherapies in subtherapeutic doses for over 30 years, and the availability of substandard artemisinins, have probably been the main driving force in the selection of the resistant phenotype in the region. A multifaceted containment programme has recently been launched, including early diagnosis and appropriate treatment, decreasing drug pressure, optimising vector control, targeting the mobile population, strengthening management and surveillance systems, and operational research. Mathematical modelling can be a useful tool to evaluate possible strategies for containment. Parenteral In nearly all countries in which malaria is endemic, antimalarial properties (artemisinin) was identified, and Administered by injection. artemisinin combination therapies (ACT) are now the several more potent derivatives were synthesized, includ- recommended first-line therapy for uncomplicated ing artesunate, artemether and dihydroartemisinin11 Plasmodium falciparum malaria, a policy endorsed by (FIG. 1). Artemisinin derivatives have an excellent safety the WHO1. This change in policy followed a period profile in the treatment of malaria, a rapid onset of action of increasing failure rates with chloroquine and later and are active against the broadest range of stages in the sulphadoxine–pyrimethamine treatment, which arose life cycle of Plasmodium spp. compared with other anti- from the development of resistant P. -

Annex 4: Drug Dosages for Children (Formulary)
Medicines Dosage Form Dose according to body weight (calculate if weight is below or over) 3-6 kg 6-10 kg 10-15 kg 15-20 kg 20-29 kg albendazole 200 mg (half tablet) 12-24 months chewable tablet, 400mg 400 mg (one tablet) over 24 months amodiaquine 10 mg base/kg/3 days (total dose 30 mg base/kg) tablet, 200mg - - 1 1 1 amoxicillin 15 mg/kg/dose for 7 days tablet/capsule 250 mg ¼ ½ ¾ 1 1½ oral suspension, 125mg/5ml 2.5 ml 5 ml 7.5 ml 10 ml - non-severe pneumonia: 25 mg/kg 2 times per day for 3 days tablet/capsule 250 mg ½ 1 1½ 2 2½ oral suspension, 125mg/5ml 5 ml 10 ml 15 ml - - ampicillin IM 50 mg/kg/6 hours Vial of 500 mg mixed with 2.1 ml 1 ml 2 ml 3 ml 5 ml 6 ml sterile water to give 500 mg/2.5 ml artemether IM 3.2 mg/kg once on day 1 injection, 40mg/ml in 1ml ampoule then injection, 80mg/ml in 1ml ampoule see Chapter 5, management of the child with malaria IM 1.6 mg/kg daily until oral therapy is possible, total therapy one week artemether + fixed dose treatment (20+120 mg) twice daily for 3 days tablet 10+120 mg see Chapter 5, management of the child with malaria lumefantrine artesunate severe malaria: IV or IM 2.4 mg/kg over 3 minutes at 0, 12 and 24 vial of 60 mg in 0.6 ml with 3.4 ml hours on day 1. -

Cytochrome P450 Oxidative Metabolism: Contributions to the Pharmacokinetics, Safety, and Efficacy of Xenobiotics
1521-009X/44/8/1229–1245$25.00 http://dx.doi.org/10.1124/dmd.116.071753 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:1229–1245, August 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Special Section on Emerging Novel Enzyme Pathways in Drug Metabolism—Commentary Cytochrome P450 and Non–Cytochrome P450 Oxidative Metabolism: Contributions to the Pharmacokinetics, Safety, and Efficacy of Xenobiotics Robert S. Foti and Deepak K. Dalvie Pharmacokinetics and Drug Metabolism, Amgen, Cambridge, Massachusetts (R.S.F.); and Pharmacokinetics, Dynamics, and Metabolism, Pfizer, La Jolla, California (D.K.D.) Downloaded from Received May 24, 2016; accepted June 10, 2016 ABSTRACT The drug-metabolizing enzymes that contribute to the metabolism this end, this Special Section on Emerging Novel Enzyme Pathways or bioactivation of a drug play a crucial role in defining the in Drug Metabolism will highlight a number of advancements that dmd.aspetjournals.org absorption, distribution, metabolism, and excretion properties of have recently been reported. The included articles support the that drug. Although the overall effect of the cytochrome P450 (P450) important role of non-P450 enzymes in the clearance pathways of family of drug-metabolizing enzymes in this capacity cannot be U.S. Food and Drug Administration–approved drugs over the past understated, advancements in the field of non-P450–mediated me- 10 years. Specific examples will detail recent reports of aldehyde tabolism have garnered increasing attention in recent years. This is oxidase, flavin-containing monooxygenase, and other non-P450 perhaps a direct result of our ability to systematically avoid P450 pathways that contribute to the metabolic, pharmacokinetic, or liabilities by introducing chemical moieties that are not susceptible pharmacodynamic properties of xenobiotic compounds. -
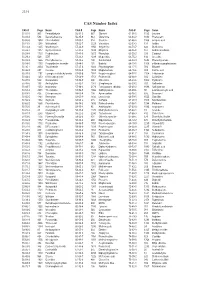
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Downloaded and Saved in PDB Format
bioRxiv preprint doi: https://doi.org/10.1101/833145; this version posted November 6, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Full title: Efficacy of Lumefantrine against piperaquine resistant Plasmodium berghei parasites is 2 selectively restored by probenecid, verapamil, and cyproheptadine through ferredoxin NADP+- 3 reductase and cysteine desulfurase 4 5 Short title: Mechanisms of Lumefantrine resistance and reversal in Plasmodium berghei ANKA 6 7 Authors: Fagdéba David Bara1,2,3, Loise Ndung’u1, Noah Machuki Onchieku1, Beatrice Irungu2, 8 Simplice Damintoti Karou3, Francis Kimani4, Damaris Matoke-Muhia4, Peter Mwitari2, Gabriel 9 Magoma1,5, Alexis Nzila6, Daniel Kiboi5* 10 11 Affiliations: 1Department of Molecular Biology and Biotechnology, Pan African University 12 Institute for Basic Sciences, Technology and Innovation (PAUSTI), Nairobi, Kenya. 2Centre for 13 Traditional Medicine and Drug Research, Kenya Medical Research Institute, Nairobi, Kenya. 14 3School of Food and Biology Technology, Universite du Lome, Lome, Togo. 4Centre for 15 Biotechnology Research and Development, Kenya Medical Research Institute, Nairobi, Kenya. 16 5Department of Biochemistry, Jomo Kenyatta University of Agriculture and Technology 17 (JKUAT), Nairobi, Kenya. 6Department of Life Sciences, King Fahd University of Petroleum and 18 Minerals, Dharam, Saudi Arabia. 19 20 Corresponding author: [email protected] ; [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/833145; this version posted November 6, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity.