Update on Thrombotic Thrombocytopenic Purpura
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thrombotic Thrombocytopenic Purpura and Systemic Lupus Erythematosus: Successful Management of a Rare Presentation
Indian J Crit Care Med July-September 2008 Vol 12 Issue 3 Case Report Thrombotic thrombocytopenic purpura and systemic lupus erythematosus: Successful management of a rare presentation Pratish George, Jasmine Das, Basant Pawar1, Naveen Kakkar2 Thrombotic thrombocytopenic purpura (TTP) and systemic lupus erythematosus (SLE) very rarely present simultaneously and pose a diagnostic and therapeutic dilemma to the critical care team. Prompt diagnosis and management with plasma exchange and immunosuppression is life-saving. A patient critically ill with TTP and SLE, successfully managed in the acute period of illness with plasma exchange, steroids and Abstract mycophenolate mofetil is described. Key words: Plasma exchange, systemic lupus erythematosus, thrombotic thrombocytopenic purpura Introduction Case Report Systemic lupus erythematosis (SLE) is diagnosed by A 30-year-old lady was admitted with fever and the presence of four or more of the following criteria, jaundice. A week earlier she had undergone an serially or simultaneously: malar rash, discoid rash, uncomplicated medical termination of pregnancy at photosensitivity, oral ulcers, non erosive arthritis, serositis, another hospital, at 13 weeks of gestation. She had an renal abnormalities including proteinuria or active urinary uneventful pregnancy with twins two years earlier and sediments, neuropsychiatric features, hematological the twins were diagnosed to have thalassemia major. abnormalities including hemolytic anemia, leucopenia, She was subsequently diagnosed to have thalassemia lymphopenia and thrombocytopenia, immunological minor and her husband had thalassemia minor trait. No markers like anti-ds DNA or anti-Smith antibody and high earlier history of spontaneous Þ rst trimester abortions Antinuclear antibody titres. Thrombotic thrombocytopenic was present. purpura (TTP) in patients with SLE is extremely rare. -

Dermatologic Manifestations and Complications of COVID-19
American Journal of Emergency Medicine 38 (2020) 1715–1721 Contents lists available at ScienceDirect American Journal of Emergency Medicine journal homepage: www.elsevier.com/locate/ajem Dermatologic manifestations and complications of COVID-19 Michael Gottlieb, MD a,⁎,BritLong,MDb a Department of Emergency Medicine, Rush University Medical Center, United States of America b Department of Emergency Medicine, Brooke Army Medical Center, United States of America article info abstract Article history: The novel coronavirus disease of 2019 (COVID-19) is associated with significant morbidity and mortality. While Received 9 May 2020 much of the focus has been on the cardiac and pulmonary complications, there are several important dermato- Accepted 3 June 2020 logic components that clinicians must be aware of. Available online xxxx Objective: This brief report summarizes the dermatologic manifestations and complications associated with COVID-19 with an emphasis on Emergency Medicine clinicians. Keywords: COVID-19 Discussion: Dermatologic manifestations of COVID-19 are increasingly recognized within the literature. The pri- fi SARS-CoV-2 mary etiologies include vasculitis versus direct viral involvement. There are several types of skin ndings de- Coronavirus scribed in association with COVID-19. These include maculopapular rashes, urticaria, vesicles, petechiae, Dermatology purpura, chilblains, livedo racemosa, and distal limb ischemia. While most of these dermatologic findings are Skin self-resolving, they can help increase one's suspicion for COVID-19. Emergency medicine Conclusion: It is important to be aware of the dermatologic manifestations and complications of COVID-19. Knowledge of the components is important to help identify potential COVID-19 patients and properly treat complications. © 2020 Elsevier Inc. -

A Rare Syndrome with Alemtuzumab, Review of Monitoring Protocol
Open Access Case Report DOI: 10.7759/cureus.5715 Idiopathic Thrombocytopenic Purpura: A Rare Syndrome with Alemtuzumab, Review of Monitoring Protocol Deepika Sarvepalli 1 , Mamoon Ur Rashid 2 , Waqas Ullah 3 , Yousaf Zafar 4 , Muzammil Khan 5 1. Internal Medicine, Guntur Medical College, Guntur, IND 2. Internal Medicine, AdventHealth, Orlando, USA 3. Internal Medicine, Abington Hospital - Jefferson Health, Abington, USA 4. Internal Medicine, University of Missouri - Kansas City School of Medicine, Kansas City, USA 5. Internal Medicine, Khyber Teaching Hospital, Peshawar, PAK Corresponding author: Deepika Sarvepalli, [email protected] Abstract Alemtuzumab, a humanized monoclonal antibody that targets surface molecule CD52, causes rapid and complete depletion of circulating T- and B-lymphocytes through antibody-dependent cell-mediated and complement-mediated cytotoxicity. Alemtuzumab has demonstrated superior efficacy compared to subcutaneous interferon beta-1a (SC IFNB-1a) in patients with multiple sclerosis (MS). Alemtuzumab treatment causes a rare and distinct form of secondary immune thrombocytopenic purpura (ITP), characterized by delayed onset, responsiveness to conventional therapies, and prolonged remission following treatment. In phase two and three clinical trials, the incidence of ITP was higher with alemtuzumab treatment compared to the patients receiving SC IFNB-1a. Here we report a case of ITP occurring two years after the first treatment with alemtuzumab. The patient recovered completely after a timely diagnosis -

Urticarial Vasculitis Associated with Essential Thrombocythaemia
Acta Derm Venereol 2014; 94: 244–245 SHORT COMMUNICATION Urticarial Vasculitis Associated with Essential Thrombocythaemia Annabel D. Scott, Nicholas Francis, Helen Yarranton and Sarita Singh Dermatology Registrar, Department of Dermatology, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, United Kingdom. E-mail: [email protected] Accepted Apr 3, 2013; Epub ahead of print Aug 27, 2013 Urticarial vasculitis is a form of leucocytoclastic vas- prednisolone 30 mg once daily, which controlled her culitis whereby the skin lesions resemble urticaria. It is symptoms. associated with systemic lupus erythematosus, Sjögren’s A biopsy was taken from an uticarial lesion on the syndrome, hepatitis B and C viruses (1). Rarely it is asso- arm. Histology showed numerous perivascular neutro- ciated with an underlying haematological disorders and, phils and eosinophils with margination of neutrophils to the best of our knowledge, has never been reported in in the lumen of vessels and some leucocytoclasis with association with essential thrombocythaemia. We present red cell extravasation in keeping with an urticarial a case report of urticarial vasculitis associated with es- vasculitis (Fig. 2). sential thrombocythaemia. Blood tests revealed an erythrocyte sedimentation rate of 47 mm/h (normal range 1–12), a platelet count of 1,098 × 109/l (normal range 135–400) and an eosi- CASE REPORT nophilia of 1.0 × 109/l (normal range 0–0.2). Comple- A 32-year-old woman presented with a several month ment levels, thyroid function, serum iron, haemoglobin, history of recurrent urticaria without angioedema, 4 C-reactive protein, anti-nuclear antibody, anti-nuclear months post-partum. -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

Immune-Pathophysiology and -Therapy of Childhood Purpura
Egypt J Pediatr Allergy Immunol 2009;7(1):3-13. Review article Immune-pathophysiology and -therapy of childhood purpura Safinaz A Elhabashy Professor of Pediatrics, Ain Shams University, Cairo Childhood purpura - Overview vasculitic disorders present with palpable Purpura (from the Latin, purpura, meaning purpura2. Purpura may be secondary to "purple") is the appearance of red or purple thrombocytopenia, platelet dysfunction, discolorations on the skin that do not blanch on coagulation factor deficiency or vascular defect as applying pressure. They are caused by bleeding shown in table 1. underneath the skin. Purpura measure 0.3-1cm, A thorough history (Table 2) and a careful while petechiae measure less than 3mm and physical examination (Table 3) are critical first ecchymoses greater than 1cm1. The integrity of steps in the evaluation of children with purpura3. the vascular system depends on three interacting When the history and physical examination elements: platelets, plasma coagulation factors suggest the presence of a bleeding disorder, and blood vessels. All three elements are required laboratory screening studies may include a for proper hemostasis, but the pattern of bleeding complete blood count, peripheral blood smear, depends to some extent on the specific defect. In prothrombin time (PT) and activated partial general, platelet disorders manifest petechiae, thromboplastin time (aPTT). With few exceptions, mucosal bleeding (wet purpura) or, rarely, central these studies should identify most hemostatic nervous system bleeding; -

Bruise, Contusion & Ecchymosis Conventions
Bruise, Contusion and Ecchymosis MedDRA Proactivity Proposal Implementation MedDRA Version 16.0 I. MSSO Recognized Definitions of Concepts and Terms The MSSO has designated Dorland’s Illustrated Medical Dictionary as the standard reference for medical definitions. The following definitions are cited from Dorland’s 27th edition: Bruise – A superficial injury produced by impact without laceration; a contusion Contusion – A bruise; an injury of a part without a break in the skin Ecchymosis – A small hemorrhagic spot, larger than a petechia, in the skin or mucous membrane forming a nonelevated, rounded or irregular, blue or purplish patch. Hematoma – A localized collection of blood, usually clotted, in an organ, space, or tissue, due to a break in the wall of a blood vessel. Hemorrhage – The escape of blood from the vessels; bleeding. Petechia – A pinpoint, non-raised, perfectly round, purplish red spot caused by intradermal or submucous hemorrhage. Additional comments regarding the definitions: Bruise and contusion are synonymous, and are often used in a colloquial context. Bruise and contusion are each considered a result of injury. Bruise and contusion have been used to describe minor hemorrhage within tissue, where traumatized blood vessels leak blood into the interstitial space. Commonly, capillaries and sometimes venules are injured within skin, subcutaneous tissue, muscle, or bone. In addition to trauma, the terms bruise, ecchymosis, and to a lesser extent, contusion, have also been used as clinical signs of disorders of platelet function, coagulopathies, venous congestion, allergic reactions, etc. Hemorrhage may be used to describe blood escaping from vessels and retained in the interstitial space, and perhaps more commonly, to describe the escape of blood from vessels, and flowing freely external to the tissues. -
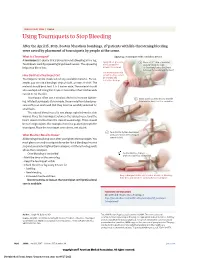
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -
ER Guide to Bleeding Disorders
Bleeding disorders ER guide to bleeding disorders 1 Table of contents 4 General Guidelines 4–5 national Hemophilia Foundation guidelines 5–10 Treatment options 10 HemopHilia a Name:__________________________________________________________________________________________________ 10–11 national Hemophilia Foundation guidelines Address:________________________________________________________________________________________________ 12 dosage chart Phone:__________________________________________________________________________________________________ 14–15 Treatment products 16 HemopHilia B In case of emergency, contact: ______________________________________________________________________________ 16 national Hemophilia Foundation guidelines Relation to patient:________________________________________________________________________________________ 17 dosage chart 18 Treatment products 19 HemopHilia a or B with inHiBiTors Diagnosis: Hemophilia A: Mild Moderate Severe 20 national Hemophilia Foundation guidelines Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 21 Treatment products Hemophilia B: Mild Moderate Severe 22–23 Von willeBrand disease Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 23–24 national Hemophilia Foundation guidelines von Willebrand disease: Type 1 Type 2 Type 3 Platelet type 25 Treatment products 27 Bibliography Preferred product:_________________________________________________________________________________________ Dose for life-threatening -

VAXZEVRIA/COVID-19 Vaccine Astrazeneca: Risk of Thrombosis in Combination with Thrombocytopenia – Updated Information
AstraZeneca Block B Liffey Valley Office Campus Dublin 22 D22 X0Y3 astrazeneca.com 2nd June 2021 VAXZEVRIA/COVID-19 Vaccine AstraZeneca: Risk of thrombosis in combination with thrombocytopenia – Updated information Dear Healthcare Professional, Please refer to previous Direct Healthcare Professional Communications (DHPCs) of 24th March and 13th April, 2021. AstraZeneca AB in agreement with the European Medicines Agency and the Health Products Regulatory Authority (HPRA) would like to inform you of the following: Summary Vaxzevria is contraindicated in individuals who have experienced Thrombosis with Thrombocytopenia Syndrome (TTS) following previous vaccination with Vaxzevria. TTS requires specialised clinical management. Healthcare professionals should consult applicable guidance and/or consult specialists (e.g., haematologists, specialists in coagulation) to diagnose and treat this condition. Individuals diagnosed with thrombocytopenia within 3 weeks after vaccination with Vaxzevria should be actively investigated for signs of thrombosis. Similarly, individuals who present with thrombosis within 3 weeks of vaccination should be evaluated for thrombocytopenia. The Vaxzevria Summary of Product Characteristics (SmPC) has been updated accordingly with this information. Background on the safety concern Vaxzevria is indicated for active immunisation to prevent COVID-19 caused by SARS-CoV-2, in individuals 18 years of age and older. A combination of thrombosis and thrombocytopenia, in some cases accompanied by bleeding, has been observed very rarely following vaccination with Vaxzevria. This includes severe cases presenting as venous thrombosis, including in unusual sites, such as cerebral venous sinus thrombosis and splanchnic vein thrombosis, as well as arterial thrombosis, concomitant with AstraZeneca Pharmaceuticals (Ireland) DAC T: +353 1 609 7100 F: +353 1 679 6650 Registered Office: 6th Floor, South Bank House, Barrow Street, Dublin 4, D04 TR29, Ireland Registered in Ireland No. -

Appendix Search Strategy Treatment of Hemophilia.Pdf
Appendix Search strategies Hemophilia – general aspects PubMed (NLM) September 2009 Von Willebrand disease (TiAb) AND Controlled clinical trial (PT) NOT Purpura, Thrombocytopenic (Me) Angiohemophilia (TiAb) Meta analysis (PT) Blood coagulation disorders (Me) Randomized controlled trial (PT) Hemophilia (TiAb) Systematic (SB) Haemophilia (TiAb) Bleeding disorder (TiAb) Random* (Ti) Bleeding disorders (TiAb) OR Control* (Ti) NOT Medline (SB) ("controlled clinical trial"[Publication Type] OR "meta analysis"[Publication Type] OR "randomized controlled trial"[Publication Type] OR systematic[sb] OR ((random*[Title] OR control*[Title]) NOT Medline[sb])) AND ("von Willebrand Disease"[title/abstract] OR "angiohemophilia"[title/Abstract] OR "Blood Coagulation Disorders"[Mesh terms] OR "hemophilia"[title/abstract] OR "haemophilia"[title/abstract] OR "bleeding disorder"[title/abstract] OR "bleeding disorders"[Title/abstract]) NOT "Purpura, Thrombocytopenic"[MeSH Terms] 211 Hemophilia – general aspects Embase.com (Elsevier) September 2009 Blood clotting factor deficiency (Exp,MJR) AND Clinical trial (Exp) NOT Thrombocytopenic purpura (Exp) Von Willebrand disease (Ti) Intervention study (De) Angiohemophilia (Ti) Longitudinal study (De) Angiohaemophilia (Ti) Prospective study (De) Hemophilia (Ti) Meta analysis (De) Haemophilia (Ti) Systematic review (De) Bleeding disorder (Ti) Random* (Ti) Bleeding disorders (Ti) Control* (Ti) ('blood clotting factor deficiency'/exp/mjOR 'von willebrand disease':ti OR 'angiohemophilia':ti OR 'angiohaemophilia':ti OR 'hemophilia':ti