ETD Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Music of Ghana and Tanzania
MUSIC OF GHANA AND TANZANIA: A BRIEF COMPARISON AND DESCRIPTION OF VARIOUS AFRICAN MUSIC SCHOOLS Heather Bergseth A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of MASTERDecember OF 2011MUSIC Committee: David Harnish, Advisor Kara Attrep © 2011 Heather Bergseth All Rights Reserved iii ABSTRACT David Harnish, Advisor This thesis is based on my engagement and observations of various music schools in Ghana, West Africa, and Tanzania, East Africa. I spent the last three summers learning traditional dance- drumming in Ghana, West Africa. I focus primarily on two schools that I have significant recent experience with: the Dagbe Arts Centre in Kopeyia and the Dagara Music and Arts Center in Medie. While at Dagbe, I studied the music and dance of the Anlo-Ewe ethnic group, a people who live primarily in the Volta region of South-eastern Ghana, but who also inhabit neighboring countries as far as Togo and Benin. I took classes and lessons with the staff as well as with the director of Dagbe, Emmanuel Agbeli, a teacher and performer of Ewe dance-drumming. His father, Godwin Agbeli, founded the Dagbe Arts Centre in order to teach others, including foreigners, the musical styles, dances, and diverse artistic cultures of the Ewe people. The Dagara Music and Arts Center was founded by Bernard Woma, a master drummer and gyil (xylophone) player. The DMC or Dagara Music Center is situated in the town of Medie just outside of Accra. Mr. Woma hosts primarily international students at his compound, focusing on various musical styles, including his own culture, the Dagara, in addition music and dance of the Dagbamba, Ewe, and Ga ethnic groups. -

Faculty of Arts and Sciences Dean's Annual Report
Faculty of Arts and Sciences Dean’s Annual Report Fiscal Year 2011 Harvard University 1 Table of Contents Harvard College ........................................................................................................................... 9 Graduate School of Arts and Sciences (GSAS) ......................................................................... 23 Division of Arts and Humanities ................................................................................................ 29 Division of Science .................................................................................................................... 34 Division of Social Science ......................................................................................................... 38 School of Engineering and Applied Sciences (SEAS) ............................................................... 42 Faculty Trends ............................................................................................................................ 49 Harvard College Library ............................................................................................................ 54 Sustainability Report Card ......................................................................................................... 59 Financial Report ......................................................................................................................... 62 2 Harvard University Faculty of Arts and Sciences Office of the Dean University Hall Cambridge, Massachusetts -

Kenya.Pdf 43
Table of Contents PROFILE ..............................................................................................................6 Introduction .................................................................................................................................................. 6 Facts and Figures.......................................................................................................................................... 6 International Disputes: .............................................................................................................................. 11 Trafficking in Persons:............................................................................................................................... 11 Illicit Drugs: ................................................................................................................................................ 11 GEOGRAPHY.....................................................................................................12 Kenya’s Neighborhood............................................................................................................................... 12 Somalia ........................................................................................................................................................ 12 Ethiopia ....................................................................................................................................................... 12 Sudan.......................................................................................................................................................... -

Women in the Rural Society of South-West Wales, C.1780-1870
_________________________________________________________________________Swansea University E-Theses Women in the rural society of south-west Wales, c.1780-1870. Thomas, Wilma R How to cite: _________________________________________________________________________ Thomas, Wilma R (2003) Women in the rural society of south-west Wales, c.1780-1870.. thesis, Swansea University. http://cronfa.swan.ac.uk/Record/cronfa42585 Use policy: _________________________________________________________________________ This item is brought to you by Swansea University. Any person downloading material is agreeing to abide by the terms of the repository licence: copies of full text items may be used or reproduced in any format or medium, without prior permission for personal research or study, educational or non-commercial purposes only. The copyright for any work remains with the original author unless otherwise specified. The full-text must not be sold in any format or medium without the formal permission of the copyright holder. Permission for multiple reproductions should be obtained from the original author. Authors are personally responsible for adhering to copyright and publisher restrictions when uploading content to the repository. Please link to the metadata record in the Swansea University repository, Cronfa (link given in the citation reference above.) http://www.swansea.ac.uk/library/researchsupport/ris-support/ Women in the Rural Society of south-west Wales, c.1780-1870 Wilma R. Thomas Submitted to the University of Wales in fulfillment of the requirements for the Degree of Doctor of Philosophy of History University of Wales Swansea 2003 ProQuest Number: 10805343 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. -

Wildlife and Forest Biodiversity Conservation in Taita, Kenya Njogu, J.G
Community-based conservation in an entitlement perspective: wildlife and forest biodiversity conservation in Taita, Kenya Njogu, J.G. Citation Njogu, J. G. (2004). Community-based conservation in an entitlement perspective: wildlife and forest biodiversity conservation in Taita, Kenya. Leiden: African Studies Centre. Retrieved from https://hdl.handle.net/1887/12921 Version: Not Applicable (or Unknown) License: Leiden University Non-exclusive license Downloaded from: https://hdl.handle.net/1887/12921 Note: To cite this publication please use the final published version (if applicable). Community-based conservation in an entitlement perspective African Studies Centre Research Report 73 / 2004 Community-based conservation in an entitlement perspective Wildlife and forest biodiversity conservation in Taita, Kenya James Gichiah Njogu This PhD project was part of the research programme Resources, Environment and Development Research Associates (REDRA) of the Amsterdam Research Institute for Global Issues and Development Studies (AGIDS). It also formed part of Working Programme 1, Natural resource management: Knowledge transfer, social insecurity and cultural coping, of the Research School for Resource Studies for Development (CERES). The Netherlands Foundation for the Advancement of Tropical Research (WOTRO) jointly with the Amsterdam Research Institute for Global Issues and Development Studies (AGIDS) of the University of Amsterdam funded this research. The School of Environmental Studies of Moi University (Eldoret, Kenya) provided institutional support. Published by: African Studies Centre P.O. Box 9555 2300 RB Leiden Tel: + 31 - 71 - 527 33 72 Fax: + 31 - 71 - 527 33 44 E-mail: [email protected] Website:http://asc.leidenuniv.nl Printed by: PrintPartners Ipskamp B.V., Enschede ISBN 90.5448.057.2 © African Studies Centre, Leiden, 2004 Contents List of maps viii List of figures viii List of boxes viii List of tables ix List of plates x List of abbreviations x Acknowledgements xii PART 1: THE CONTEXT 1 1. -
Note to User
NOTE TO USER Page(s) not included in the original manuscript are unavailable from the author or university. The manuscript was microfilmed as received. This is reproduction is the best copy available THE NUTRIENT AND PHYTONUTRIENT COMPOSITION OF ONTARIO GROWBEANS AND =IR EFFECT ON AZOXYMETHANE INDUCED COLONTC PRENEOPLASIA IN RATS Heten Anita MiUie Samek A thesis submitted in confonnity with the requirements for the degree of Masters of Science Graduate Department of Nutritional Sciences University of Toronto Copyright by Helen Anita Millie Samek 200 1 Acquisitions and Acquisit'hs et Bibliogtaphic Services services bibliiraphiques The author has granted a non- L'auteur a accordé une licence non exclusive licence aliowhg the exclusive permettant a la National Library of Canada to BkIiothèque nationale du Canada de reproduce, loan, distriiute or sell reproduire, prêter, distribuer ou copies of this thesis in rnicroform, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/film, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auîeur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts fiom it Ni la thèse ni des extraits substantiels may be printed or othenivise de ceile-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son permission. autorisation. TEE NUTRIENT AND PaYTONUTRIENT COMPOSITION OF ONTARIO GROWN BEANS AND THEIR EFFECT ON AZOXYMETHANE INDUCED COLONIC PRENEOPLASIA IN RATS Master of Science, 200 1 Helen A. Samek Graduate Department of Nutritional Sciences University of Toronto Beans have long been recognized for their nutritionai quality. -

Service, Slavery ('Utumwa') and Swahili Social Reality
AAP 37 (1994}. 87-107 SERVICE, SLAVERY ('UTUMWA') AND SWAHILI SOCIAL REALITY CAROL M. EASTMAN Introduction A basic dichotomy between what is civilized (uungwana) and what is barbarian (ushenzi or 'foreign, strange') has existed for centuries on the East African Coast. The concept of utumwa 'slavery, service' may be seen to mediate the opposition between the civilized and the uncivilized over time In this paper, I invoke a sociolinguistic approach to complement the historical record in order to examine the use of the word utumwa itself as it has changed to reveal distinct class and gender connotations especially in northem Swahili communities. To explore utumwa is difficult. There is no consensus with regard to what the word and its derivatives mean that applies consistently, yet it is clear that there has been a meaning shift since the nineteenth century. This paper examines the construction and transformation of a non-Westem-molded form of service in Africa. Oral traditions and terminological variation will be brought to bear on an analysis of utumwa 'slavery, service' as an important concept of social change in East Africa and, in particular, on the northern Kenya coast What this term, its derivatives, and other terms associated with it have come to mean to Swahili speakers and culture bearers will be seen to mirror aspects of the history of Swahili-speaking people fi-om the 1Oth-11th century to the present Utumwa functioned in contrast to notions of civilization (uungwana) and, later, Arabness (uarabu or ustaarabu). The construction -
Retrospect Magazine Design Layout.Indd
2000 HELLO HELLO MMILLENNIUMILLENNIUM 1999 CCELEBRATIONSELEBRATIONS GOODBYE GOODBYE A lot of people approached the end of 1999 with trepi- dation. There were reports that aeroplanes would fall out of the sky at the stroke of midnight. All computers would crash, leading to world turmoil and people would wake up to a world EXAMPLE IMAGE NOT COPYRIGHT that they did not recognise. CLEARED By Sharon RM Stevens n acknowledgement of this huge mile- Istone in the World’s calendar, most countries and or cities decided to meet the momentous occasion in various ways. Some planned fixed structures to celebrate, while others met the New Year by changing Brighton millennium celebration, image from the Zap archive names of buildings, cities etc. Still, others EXAMPLE IMAGE planned firework displays beyond anything NOT COPYRIGHT anyone had ever CLEARED seen. In an attempt to capture events Tower el ff at the turn of the century, led by the BBC and WGBH-TV and several other EXAMPLE IMAGE companies, the NOT COPYRIGHT CLEARED 2000 Today pro- gramme was cre- Queen Elizabeth II and Prince Philip at the opening of the Millennium Dome Fireworks burst from the Ei ated. It was to be a way of encapsulating the worldwide New the New year. Samoa being the last. Year events over a 28hour period, starting However, it was later controversially from 31st of December 1999 to the 1st of reported that the first country to cele- January 2000. The TV coverage of New brate the dawning of 2000 was, in fact, Year celebrations would span across sev- the Chatham Islands, New Zealand. -

Esoto: Where Girls and Warriors Meet the Changing Space and Perceptions of Esoto Over Generations of the Maasai Women of Engare Sero Lisa Wilmore SIT Study Abroad
SIT Graduate Institute/SIT Study Abroad SIT Digital Collections Independent Study Project (ISP) Collection SIT Study Abroad Fall 2010 Esoto: Where Girls and Warriors Meet The Changing Space and Perceptions of Esoto Over Generations of the Maasai Women of Engare Sero Lisa Wilmore SIT Study Abroad Follow this and additional works at: https://digitalcollections.sit.edu/isp_collection Part of the African Languages and Societies Commons, Dance Commons, and the Social and Cultural Anthropology Commons Recommended Citation Wilmore, Lisa, "Esoto: Where Girls and Warriors Meet The hC anging Space and Perceptions of Esoto Over Generations of the Maasai Women of Engare Sero" (2010). Independent Study Project (ISP) Collection. 900. https://digitalcollections.sit.edu/isp_collection/900 This Unpublished Paper is brought to you for free and open access by the SIT Study Abroad at SIT Digital Collections. It has been accepted for inclusion in Independent Study Project (ISP) Collection by an authorized administrator of SIT Digital Collections. For more information, please contact [email protected]. Esoto: where girls and warriors meet The changing space and perceptions of esoto over generations of the Maasai women of Engare Sero by Lisa Wilmore SIT Tanzania: Political Ecology and Wildlife Conservation Fall 2010 Acknowledgements I must first express my thanks to the Engare Sero community who welcomed Team Natron into a place that we have all come to love after our three-week stay. Your generosity and friendship made our experience memorable. Thank you to all of the women for your graceful cooperation in the heat of a typical Engare Sero day. Your interest, sincerity, and laughter gave my project life from the first day. -

06 Session5.Pdf
The 1st World Humanities Forum Proceedings Session 5 Organizers’ Parallel Session A. UNESCO: Towards a New Humanism B. MEST/NRF: Renaissance of Humanities in Korea C. Busan Metropolitan City: Humanities for Locality The 1st World Humanities Forum Proceedings Organizers’ Parallel Session A. UNESCO: Towards a New Humanism 1. Age of Abundance / Alphonso Lingis (Pennsylvania State University) 2. Subjectivity and Solidarity – a Rebirth of Humanism / In Suk Cha (Seoul National University) 3. Reconstructing Humanism / John Crowley (UNESCO) 4. Transversality, Ecopiety, and the Future of Humanity / Hwa Yol Jung (Moravian College) Session 5 Session The Age of Abundance Alphonso Lingis Pennsylvania State University What immense and growing abundance of commodities we see about us, the result of extraordinary technological advances in industry driven by information and communications technologies! Manufacture has acquired new and advanced materials, and daily contrives new inventions and devises new products. Biotechnology is increasing food production with genetically altered plants and animals, and soon, meat not taken from butchered animals but grown from stem cells. Production is no longer bounded by the limitations of human labor; electrical and nuclear energy power the machines and robots shape materials and assemble cars, jet airplanes, computers, and soon everything. Nanotechnology is beginning to assemble molecules atom by atom, on the way to manufacture computer circuitry out of sand, gold out of lead, even living cells out of atoms. We see ourselves beginning an essentially new kind of human existence, acquiring a new nature— postevolutionary, transhuman. We are awed, fascinated, but also bewildered by the prospect with an abundance beyond all our needs and desires; how shall we deal with it? We are watching extraordinary advances in biotechnology, which promise not only to cure and prevent diseases and correct defects, but, with pharmaceuticals, gene therapy and nanotechnology, to endow our bodies and our minds with greater and also new capacities. -

Central American Immigrant Women's Perceptions of Adult Learning: a Qualitative Inquiry Ana Guisela Chupina Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 2004 Central American immigrant women's perceptions of adult learning: a qualitative inquiry Ana Guisela Chupina Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Adult and Continuing Education and Teaching Commons, Bilingual, Multilingual, and Multicultural Education Commons, Women's History Commons, and the Women's Studies Commons Recommended Citation Chupina, Ana Guisela, "Central American immigrant women's perceptions of adult learning: a qualitative inquiry " (2004). Retrospective Theses and Dissertations. 933. https://lib.dr.iastate.edu/rtd/933 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Central American immigrant women's perceptions of adult learning: A qualitative inquiry by Ana Guisela Chupina A dissertation submitted to the graduate faculty in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY Major: Education (Adult Education) Program of Study Committee: Nancy J. Evans, Major Professor Jackie M. Blount Deborah W. Kilgore Carlie C. Tartakov Michael B. Whiteford Iowa State University Ames, Iowa 2004 Copyright © Ana Guisela Chupina, 2004. All rights reserved. UMI Number: 3145633 Copyright 2004 by Chupina, Ana Guisela All rights reserved. INFORMATION TO USERS The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleed-through, substandard margins, and improper alignment can adversely affect reproduction. -
New Year Special! 3 O 7 @ 2 ) W 0 W 0 W 8
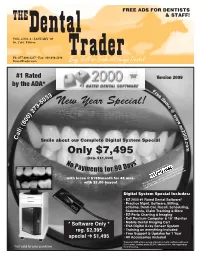
FREE ADS FOR DENTISTS THE & STAFF! VOL. 6 NO. Dental1 • JANUARY ‘09 So. Calif. Edition Ph: 877-888-4237 • Fax: 949-498-1198 DentalTrader.com TraderBuy, Sell or Trade all things Dental #1 Rated Version 2009 by the ADA* Fr ee 3 d 3 e 0 m -5 New Year Special! 3 o 7 @ 2 ) w 0 w 0 w 8 . ( e z : l 2 l 0 a 0 9 C . Smile about our Complete Digital System Special c o Only $7,495 m (reg. $11,000) No s* Paym 0 Day ents for 9 Lease provided by with lease @ $198/month for 48 mos. with $1.00 buyout “Financial Solutions for Growing Businesses” for other lease options: contact Erik Mohler @877-692-8156 or [email protected] Digital System Special Includes: • EZ 2000 #1 Rated Dental Software* • Practice Mgmt. Software, Billing, eClaims, Denti-Cal, Recall, Scheduling, Statements, Claim Tracking & More • EZ-Perio Charting & Imaging • Dell Pentium Computer & 19” Monitor • Mobile Dental Imaging Cart * Software Only * • EVA Digital X-ray Sensor System reg. $2,395 • Training on everything included • Free Support & Updates for 1 Year special ‘ $1,495 • All Accessories included *based on ADA online survey of practice mgmt. software with over 5,000 users, costing under $2,500; $99 lease doc. fee required up *not valid for prior purchase front if leasing. 2 SO. CALIFORNIA JANUARY 2009 Business Transactions WOOD & DELGADO Transition Consulting Attorneys At Law Practice Purchase Agreements Partnership Agreements Shareholder Agreements The Authority Associate Agreements Associate Buy-ins in Dental Law MSO's Lease Negotiations Loan Workouts Space Sharing/Group Solo Corporate Formations/Dissolutions Real Estate Acquisition/Sale Employee/Employment Handbooks Dental Board Defense Estate Planning Wills Trusts Power of Attorney Living Will Asset Protection Planning Offices in Irvine, San Francisco & Temecula Patrick J.