Different Body Parts' Fat Mass and Corrected QT Interval on The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lamadrid Android
ANDROID FGSDFG FDDFGDF ANTITRUST Android antitrust investigation DOMINANT POSITION mokmdokamsdfkmasodmkfosakdmfosdkmf okmsadf IT MARKET ANDROID FGSDFG FDDFGDF ANTITRUST Android antitrust investigation DOMINANT POSITION mokmdokamsdfkmasodmkfosakdmfosdkmf okmsadf IT MARKET ANDROID FGSDFG FDDFGDF ANTITRUST Android antitrust investigation DOMINANT POSITION mokmdokamsdfkmasodmkfosakdmfosdkmf okmsadf IT MARKET ANDROID THOUGHTS IN BRIEF: FGSDFG FDDFGDF(i) A quick overview of the facts (ii) Business considerations and ANTITRUSTbackground DOMINANT(iii)The POSITION Law : (I) Dominance mokmdokamsdfkmasodmkfosakdmfosdkmf(iv)The Law: (II) Predatory okmsadf allegations IT MARKET(v) The Law: (III) Bundling allegations ANDROID FGSDFG THE FACTS FDDFGDF ANTITRUST DOMINANT POSITION mokmdokamsdfkmasodmkfosakdmfosdkmf okmsadf IT MARKET • AndroidANDROID is an open source OS licensed on a royalty-free basis. Licensees remain free to do whatever they wish with the code (e.g. downloading,FGSDFG distributing or modifying –forking- it). • OEMs remain free to use Android with or without Google Apps (e.g. NokiaFDDFGDF X). • WhenANTITRUST OEMs wish to offer certain Google apps on top of Android they can enter into a MADA which requires them to (i) preload a minimum set ofDOMINANT apps (GMS); POSITION (ii) place Search widget and GooglePlay icons in a certain way; and (iii) use Google Search as default engine for the searchmokmdokamsdfkmasodmkfosakdmfosdkmf intent. okmsadf • OEMs (and users) remain at all times free to pre-install at any time any nonIT MARKET-Google app (including a non-Google App Store) = no Google walled garden (room for intra-ecosystem competition) ANDROID A MATTER OF DIFFERENT FGSDFG FDDFGDFBUSINESS MODELS ANTITRUST DOMINANT POSITION mokmdokamsdfkmasodmkfosakdmfosdkmf okmsadf IT MARKET EssentiallyANDROID 3 different business models for mobile operating systems (OSs): i. Apple’s vertically integrated model - Monetization via sales of devices. -

Meego Smartphones and Operating System Find a New Life in Jolla Ltd
Jolla Ltd. Press Release July 7, 2012 Helsinki, Finland FOR IMMEDIATE RELEASE MeeGo Smartphones and Operating System Find a New Life in Jolla Ltd. Jolla Ltd. is an independent Finland based smartphone product company which continues the excellent work that Nokia started with MeeGo. The Jolla team is formed by directors and core professionals from Nokia's MeeGo N9 organisation, together with some of the best minds working on MeeGo in the communities. Jussi Hurmola, CEO Jolla Ltd.: "Nokia created something wonderful - the world's best smartphone product. It deserves to be continued, and we will do that together with all the bright and gifted people contributing to the MeeGo success story." Jolla Ltd. will design, develop and sell new MeeGo based smartphones. Together with international private investors and partners, a new smartphone using this MeeGo based OS will be revealed later this year. Jolla Ltd. has been developing a new smartphone product and the OS since the end of 2011. The OS has evolved from MeeGo OS using Mer Core and Qt with Jolla technology including its own brand new UI. The Jolla team consists of a substantial number of MeeGo's core engineers and directors, and is aggressively hiring the top MeeGo and Linux talent to contribute to the next generation smartphone production. Company is headquartered in Helsinki, Finland and has an R&D office in Tampere, Finland. Sincerely, Jolla Ltd. Dr. Antti Saarnio - Chairman & Finance Mr. Jussi Hurmola - CEO Mr. Sami Pienimäki - VP, Sales & Business Development Mr. Stefano Mosconi - CIO Mr. Marc Dillon - COO Further inquiries: [email protected] Jolla Ltd. -
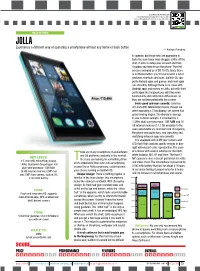
Overall Features Performance Price
Scan this code for more info. To download a barcode app, SMS <f2k> to 56677 from a mobile phone with Internet access and camera. SMARTPHONE JOLLA Experience a different way of operating a smartphone without any home or back button — Ashok Pandey to operate, but those who are upgrading to taste the new flavor may struggle a little. At the start, it asks to setup your account and then, it guides you how to use the phone. The first screen reminded us of BB 10 OS. Since there is no Home button, you’ll have to learn a lot of gestures, shortcuts and cues. Sailfish OS sup- ports Android apps and games, and most apps run smoothly. Although there is no issue with Android apps and games on Jolla, but with third party apps like facebook you will find some functionality and notification differences, as Price: `15,490 they are not integrated with the system. Feels good and runs smooth: Jolla has 4.5-inch qHD (960x450p) display, though we were expecting a 720p display, yet screen has good viewing angles. The display is average to use in direct sunlight. It is backed by a 1.4GHz dual-core processor, 1GB RAM and 16 GB internal memory (13.7 GB available to the user) expandable via microSD card. Navigating the phone was quite easy, and launching and switching between apps was smooth. It is equipped with 8 MP rear camera with LED flash that captures quality images in day- light with decent color reproduction. The cam- here are many smartphone manufacturers era comes with several settings for the flash, and OS platforms available in the market. -

Mer: Core OS Mobile & Devices
Mer: Core OS mobile & devices Qt Developer Days - Silicon Valley 2012 Carl Symons Introduction Plasma Active chooses Mer Not just another Linux distribution Focus - device providers Where's Mer? SDKs - apps & platform Get Mer Resources Carl Symons Large company Mktg/BusDev Start-ups } Slightly geeky Grassroots LinuxFest organizer KDE News editor/promo KDE Plasma Active Mer upstream and downstream First LinuxCon September 2009 Portland Moblin is a hot topic Moblin 2.1 for phones introduced MeeGo Announced February 201 0 Moblin & Maemo merger Support for Intel Atom Desktop Summit August 11 , 2011 Berlin; Free Desktop meeting Developer orientation; ExoPCs MeeGo AppStore A real Linux OS LinuxCon - Vancouver August 1 8, 2011 Intel AppUp Developer orientation; ExoPCs MeeGo AppStore show real Linux OS; possibilities Intel AppUp Elements September 28, 2011 National developer conference Tizen announced (led by Intel and Samsung) MeeGo and Qt abandoned HTML5/CSS3 Maemo Reconstructed October 3, 2011 Mer announced The spirit of MeeGo lives on Plasma Active chooses Mer October 5, 2011 No viable alternative Lightweight Mer talent and community Performant Boot time - more than a minute to about 1 5 seconds on Atom tablet Not just another Linux MeeGo - large company dominated; closed governance Mer - Core OS only Packages Focus - Device Providers Complete world class platform for building commercial products Modern, clean Linux Easy to try; easy to port Systems, structures, processes, code to serve device providers Where's Mer? X86, ARM, MIPS NemoMobile -

Download Android Os for Phone Open Source Mobile OS Alternatives to Android
download android os for phone Open Source Mobile OS Alternatives To Android. It’s no exaggeration to say that open source operating systems rule the world of mobile devices. Android is still an open-source project, after all. But, due to the bundle of proprietary software that comes along with Android on consumer devices, many people don’t consider it an open source operating system. So, what are the alternatives to Android? iOS? Maybe, but I am primarily interested in open-source alternatives to Android. I am going to list not one, not two, but several alternatives, Linux-based mobile OSes . Top Open Source alternatives to Android (and iOS) Let’s see what open source mobile operating systems are available. Just to mention, the list is not in any hierarchical or chronological order . 1. Plasma Mobile. A few years back, KDE announced its open source mobile OS, Plasma Mobile. Plasma Mobile is the mobile version of the desktop Plasma user interface, and aims to provide convergence for KDE users. It is being actively developed, and you can even find PinePhone running on Manjaro ARM while using KDE Plasma Mobile UI if you want to get your hands on a smartphone. 2. postmarketOS. PostmarketOS (pmOS for short) is a touch-optimized, pre-configured Alpine Linux with its own packages, which can be installed on smartphones. The idea is to enable a 10-year life cycle for smartphones. You probably already know that, after a few years, Android and iOS stop providing updates for older smartphones. At the same time, you can run Linux on older computers easily. -

Call Your Netbsd
Call your NetBSD BSDCan 2013 Ottawa, Canada Pierre Pronchery ([email protected]) May 17th 2013 Let's get this over with ● Pierre Pronchery ● French, based in Berlin, Germany ● Freelance IT-Security Consultant ● OSDev hobbyist ● NetBSD developer since May 2012 (khorben@) Agenda 1.Why am I doing this? 2.Target hardware: Nokia N900 3.A bit of ARM architecture 4.NetBSD on ARM 5.Challenges of the port 6.Current status 7.DeforaOS embedded desktop 8.Future plans 1. A long chain of events ● $friend0 gives me Linux CD ● Computer not happy with Linux ● Get FreeBSD CD shipped ● Stick with Linux for a while ● Play with OpenBSD on Soekris hardware ● $friend1 gets Zaurus PDA ● Switch desktop and laptop to NetBSD ● I buy a Zaurus PDA ● I try OpenBSD on Zaurus PDA 1. Chain of events, continued ● $gf gets invited to $barcamp ● I play with my Zaurus during her presentation ● $barcamp_attender sees me doing this ● Begin to work on the DeforaOS desktop ● Get some of it to run on the Zaurus ● Attend CCC Camp near Berlin during my bday ● $gf offers me an Openmoko Neo1973 ● Adapt the DeforaOS desktop to Openmoko 1. Chain of events, unchained ● $barcamp_attender was at the CCC Camp, too ● We begin to sell the Openmoko Freerunner ● Create a Linux distribution to support it ● Openmoko is EOL'd and we split ways ● $friend2 gives me sparc64 boxes ● Get more involved with NetBSD ● Nokia gives me a N900 during a developer event ● $barcamp_attender points me to a contest ● Contest is about creating an OSS tablet 1. Chain of events (out of breath) ● Run DeforaOS on NetBSD on the WeTab tablet ● Co-win the contest this way ● $friend3 boots NetBSD on Nokia N900 ● Give a talk about the WeTab tablet ● Promise to work on the Nokia N900 next thing ● Apply to BSDCan 2013 ● Taste maple syrup for the first time in Canada ● Here I am in front of you Pictures: Sharp Zaurus Pictures: Openmoko Freerunner Pictures: WeTab Pictures: DeforaOS 2. -
Therapeutic Effects of a Taurine-Magnesium Coordination Compound on Experimental Models of Type 2 Short QT Syndrome
Acta Pharmacologica Sinica (2018) 39: 382–392 © 2018 CPS and SIMM All rights reserved 1671-4083/18 www.nature.com/aps Article Therapeutic effects of a taurine-magnesium coordination compound on experimental models of type 2 short QT syndrome Meng-yao AN1, Kai SUN1, Yan LI1, Ying-ying PAN1, Yong-qiang YIN1, Yi KANG1, Tao SUN2, Hong WU1, Wei-zhen GAO1, Jian-shi LOU1, * 1Department of Pharmacology, College of Basic Medical Sciences, Tianjin Medical University, Tianjin 300070, China; 2State Key Laboratory of Medicinal Chemical Biology, Nankai University, Tianjin 300071, China Abstract Short QT syndrome (SQTS) is a genetic arrhythmogenic disease that can cause malignant arrhythmia and sudden cardiac death. The current therapies for SQTS have application restrictions. We previously found that Mg· (NH2CH2CH2SO3)2· H2O, a taurine-magnesium coordination compound (TMCC) exerted anti-arrhythmic effects with low toxicity. In this study we established 3 different models to assess the potential anti-arrhythmic effects of TMCC on type 2 short QT syndrome (SQT2). In Langendorff guinea pig-perfused hearts, perfusion of pinacidil (20 μmol/L) significantly shortened the QT interval and QTpeak and increased rTp-Te (P<0.05 vs control). Subsequently, perfusion of TMCC (1–4 mmol/L) dose-dependently increased the QT interval and QTpeak (P<0.01 vs pinacidil). TMCC perfusion also reversed the rTp-Te value to the normal range. In guinea pig ventricular myocytes, perfusion of trapidil (1 mmol/L) significantly shortened the action potential duration at 50% (APD50) and 90% repolarization (APD90), which was significantly reversed by TMCC (0.01–1 mmol/L, P<0.05 vs trapidil). -

Palm OS Cobalt 6.1 in February 2004 6.1 in February Cobalt Palm OS Release: Last 11.2 Ios Release: Latest
…… Lecture 11 Market Overview of Mobile Operating Systems and Security Aspects Mobile Business I (WS 2017/18) Prof. Dr. Kai Rannenberg . Deutsche Telekom Chair of Mobile Business & Multilateral Security . Johann Wolfgang Goethe University Frankfurt a. M. Overview …… . The market for mobile devices and mobile OS . Mobile OS unavailable to other device manufacturers . Overview . Palm OS . Apple iOS (Unix-based) . Manufacturer-independent mobile OS . Overview . Symbian platform (by Symbian Foundation) . Embedded Linux . Android (by Open Handset Alliance) . Microsoft Windows CE, Pocket PC, Pocket PC Phone Edition, Mobile . Microsoft Windows Phone 10 . Firefox OS . Attacks and Attacks and security features of selected . mobile OS 2 100% 20% 40% 60% 80% 0% Q1 '09 Q2 '09 Q3 '09 Q1 '10 Android Q2 '10 Q3 '10 Q4 '10 u Q1 '11 sers by operating sers by operating iOS Q2 '11 Worldwide smartphone Worldwide smartphone Q3 '11 Q4 '11 Microsoft Q1 '12 Q2 '12 Q3 '12 OS Q4 '12 RIM Q1 '13 Q2 '13 Q3 '13 Bada Q4' 13** Q1 '14 Q2 '14 s ystem ystem (2009 Q3 '14 Symbian Q4 '14 Q1 '15 [ Q2 '15 Statista2017a] Q3 '15 s ales ales to end Others Q4 '15 Q1 '16 Q2 '16 Q3 '16 - 2017) Q4 '16 Q1 '17 Q2 '17 3 . …… Worldwide smartphone sales to end …… users by operating system (Q2 2013) Android 79,0% Others 0,2% Symbian 0,3% Bada 0,4% BlackBerry OS 2,7% Windows 3,3% iOS 14,2% [Gartner2013] . Android iOS Windows BlackBerry OS Bada Symbian Others 4 Worldwide smartphone sales to end …… users by operating system (Q2 2014) Android 84,7% Others 0,6% BlackBerry OS 0,5% Windows 2,5% iOS 11,7% . -

Sailfish OS How to Contribute? Who Am I?
Sailfish OS How to contribute? Who am I? ● Marko “Sage” Saukko – Chief Engineer at Jolla and responsible of Hardware Adaptation team, ODM discussions, factory process, hardware adaptation architecture, ... – Worked for Jolla since March 2012 – Before Jolla worked with MeeGo project 2009- 2012. Part of team responsible of keeping the ARM port of MeeGo functional (Nokia N900 :)) Jolla & Sailfish OS ● Jolla Ltd. is Finnish technology company developing Sailfish OS ● In 2011 MeeGo was discontinued and the passionate team behind part of MeeGo wanted to continue that effort. Sailfish OS ● https://sailfishos.org/ ● Still very young operating system (~5 years) ● Mobile operating system based on Linux ● Lots of familiar open source components – rpm, systemd, dbus, wayland, pulseaudio, bluez, connman, ofono, … – Using wayland instead of X11 compared to many desktop Linux operating systems Some Sailfish OS milestones ● 2012 Announed Sailfish OS UI/SDK ● 2013 Jolla Phone with Sailfish OS 1.0 Beta ● 2014 Sailfish OS 1.0 and Hardware Adaptation Development Kit ● 2015 Sailfish OS 2.0 and Jolla Tablet ● 2016 Sailfish OS with Multi-SIM support ● 2016 Sailfish Community Device Program Where can I find Sailfish OS? ● Products using Sailfish OS – Jolla 1 – Jolla Tablet – Intex Aqua Fish – Jolla C – Turing Phone ● 40+ Community ports Sailfish OS some key things ● UI written in Qt and QML ● Mostly C/C++ in the middleware ● Android support, you can run android apps without any modifications ● Compatible with hardware running Android ● Multitasking, application covers can have functionality when apps are minimized ● Gestures based operations, less buttons to press ● Easier one handed use, e.g., pull menu Gestures ● https://sailfishos.org/wiki/User_Interface_Development ● Tap, Double tap, Edge swipe, pull menu, sub page, long-press, .. -

Jolla Releases Sailfish 3, the Third Generation of Its Independent Mobile Operating System
*For release on November 8, 2018, 3.00am EET* Jolla releases Sailfish 3, the third generation of its independent mobile operating system Helsinki, Finland, November 8, 2018 - - Jolla, the Finnish mobile company today announced the availability of Sailfish 3, the third generation of its independent mobile operating system. Sailfish 3 offers a packetized solution for various corporate environments, and a smooth and secure mobile OS for all mobile enthusiasts looking for an alternative. Sailfish X, the downloadable Sailfish OS supports now several new Sony Xperia devices, and it can be tried out free or charge. Sailfish OS, with roots in Nokia and MeeGo, has now matured to its third generation. Sailfish 3 is a secure and efficient, open source based mobile platform designed mainly for a multitude of corporate solutions. It has a deeper level of security including features, such as Mobile Device Management (MDM), fully integrated VPN solutions, enterprise WiFi, data encryption, and better and faster performance. With Sailfish 3, Jolla is also perfectly equipped to cater to all needs of different governmental and corporate clients. Sami Pienimäki, Jolla’s CEO comments: “Sailfish has come a long way, and now we are proud to start the rollout of Sailfish 3, the next chapter for the independent European mobile OS. With Sailfish 3 we are better equipped than ever to help our governmental and corporate customers to custom build secure and comprehensive mobile solutions. Sailfish OS is currently being deployed as a platform for independent regional mobile solutions in Russia, Latin America, and China, and we are constantly looking to expand to new regions. -

Sulautettu Linux Ajoneuvo-PC:N Ohjelmistoalustana
HEIKKI SARKANEN SULAUTETTU LINUX AJONEUVO-PC:N OHJELMISTOA- LUSTANA Diplomityö Tarkastaja: Prof. Kari Systä Tarkastaja ja aihe hyväksytty Teknisten tieteiden tiedekunnan tiede- kuntaneuvoston kokouksessa 14.01.2015 i TIIVISTELMÄ HEIKKI SARKANEN: Sulautettu Linux ajoneuvo-PC:n ohjelmistoalustana Tampereen teknillinen yliopisto Diplomityö, 59 sivua, 14 liitesivua Toukokuu 2016 Automaatiotekniikan koulutusohjelma Pääaine: Ohjelmistotuotanto Tarkastaja: Prof. Kari Systä Avainsanat: Linux, Qt, Yocto, U-boot, X11 Työn tavoitteena oli toteuttaa Linux-pohjainen ohjelmistoalusta mittaussovelluksel- le, joka sijoitetaan tablettia muistuttavaan, seitsemäntuumaisella kosketusnäytöllä ohjattavaan ajoneuvo-PC:hen. Työn lähtökohtana oli laitteistovalmistajan toimit- tama Freescalen i.MX6-järjestelmäpiiriin pohjautuva moduuli ja moduulin kans- sa käytettävä evaluointiemolevy. Tälle laitteistolle oli valmiina laitteistovalmistajan toimittama Yocto Linux -työkalun käyttöön perustuva laitteistotukipaketti. Tässä työssä otettiin käyttöön evaluointiemolevystä poikkeava tämän laitteen vaati- mukset toteuttava lopullinen emolevy. Valmiiseen laitteistotukipaketin komponent- teihin käynnistyslataajaan, Linuxiin, laitteistopuuhun ja Yocto-resepteihin tehtiin tarvittavat muutokset, joilla lopullisen emolevyn laitteiston ominaisuudet saatiin otettua käyttöön. Laitteiston ominaisuuksien lisäksi ohjelmistoalustaan toteutettiin alustavasti ajo- neuvo-PC:ssä tarvittavat Linux-kirjastot ja ohjelmistokomponentit valmiina saata- villa olleiden Yocto-reseptien pohjalta. -

YOCTO-PROJEKTI JA OHJELMISTOKEHITYS SULAUTETUILLE JÄRJESTELMILLE – Sovellusohjelma Raspberry Pi 3 -Alustalle 2
Opinnäytetyö AMK Tieto- ja viestintätekniikka 2019 Rauno Vesti YOCTO-PROJEKTI JA OHJELMISTOKEHITYS SULAUTETUILLE JÄRJESTELMILLE – Sovellusohjelma Raspberry Pi 3 -alustalle 2 OPINNÄYTETYÖ (AMK) | TIIVISTELMÄ TURUN AMMATTIKORKEAKOULU Tieto- ja viestintätekniikka 2019 | 40 sivua Rauno Vesti YOCTO-PROJEKTI JA OHJELMISTOKEHITYS SULAUTETUILLE JÄRJESTELMILLE • Sovellusohjelma Raspberry Pi 3 -alustalle Sulautettujen järjestelmien kehitys on tänä päivänä voimakkaasti kasvava tietotekniikan ala, johon erityisesti Internet of Things (IoT, esineiden Internet) avaa valtavat kehitysnäkymät. Opinnäytetyö liittyy keskeisesti juuri tähän tietotekniikan haaraan, ja aiheena on Yocto SDK (Software Development Kit) -sovelluskehitysympäristön asennus ja käyttö. Ohjelmointi ei varsinaisesti kuulunut opinnäytetyön piiriin, vaan ainoastaan hyvin pieni esimerkkiohjelma luotiin ja testattiin Raspberry Pi 3 -minitietokoneella. Työssä lähdettiin liikkeelle Yocto SDK:n asennustiedoston luomisesta Yocto-projektin työvälineillä, mutta itse Yocto-projektin asennus oletettiin jo ennalta suoritetuksi. Yocto-projekti ja Yocto SDK:n uusin versio ovat toiminnoiltaan keskenään lähes vastaavia, joskin Yocto SDK on enemmän suunniteltu nimenomaan sovellusohjelmien kehitykseen ja Yocto-projekti käyttöjärjestelmien luomiseen. Uusimmat versiot näistä järjestelmistä kykenevät molempiin tehtäviin, eikä ero näiden kahden välillä ole suuri. Opinnäytetyössä Yocto SDK asennettiin Linux Ubuntu 18.04 -järjestelmään Yocto-projektilla luodun asennustiedoston avulla. Yocto SDK:n asentamisen