SUMAN Guideline 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

YOGA INFLUENCE YOGA INFLUENCE English Version of YOGAPRABHAVA Discourse by Saint Gulabrao Maharaj on ‘Patanjala Yogasutra’
YOGA INFLUENCE YOGA INFLUENCE English Version of YOGAPRABHAVA Discourse by Saint Gulabrao Maharaj on ‘Patanjala Yogasutra’ Translated By Vasant Joshi Published by Vasant Joshi YOGA INFLUENCE YOGA INFLUENCE English Version of YOGAPRABHAVA Discourse by Saint Gulabrao Maharaj on ‘Patanjala Yogasutra’ * Self Published by: Vasant Joshi English Translator: Vasant Joshi © B-8, Sarasnagar, Siddhivinayak Society, Shukrawar Peth, Pune 411021. Mobile.: +91-9422024655 | Email : [email protected] * All rights reserved with English Translator No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical including photocopying recording or by any information storage and retrieval system, without permission in writing from the English Translator. * Typesetting and Formatting Books and Beyond Mrs Ujwala Marne New Ahire Gaon, Warje, Pune. Mobile. : +91-8805412827 / 7058084127 | Email: [email protected] * Preface by : Dr. Vijay Bhatkar, Chief Mentor, Multiversity. * Cover Design by : Aadity Ingawale * First Edition : 26th January 2021 YOGA INFLUENCE DEDICATED TO THE MEMORY OF G My Brother My Sister Late Prabhakar Joshi Late Sudha Natu yG y YOGA INFLUENCE INDEX Subject Page No. Part I Preface - Dr. Vijay Bhatkar I Prologue of English Translator - Vasant Joshi IV Acquaintance - Dr. K. M. Ghatate VI Autobiography of Saint Gulabrao Maharaj XLII Introduction - Rajeshwar Tripurwar LI Swami Bechiranand - Rajeshwar Tripurwar LVI Tribute - Vasant Joshi LIX Part II Chapter I : Introduction 4 to 37 Aphorism 1 to 22 Chapter II : God Meditation 38 to 163 Aphorism 23 to 33 Chpter III : Study 164 to 300 Aphorism 34 to 39 Chapter IV : Fruit of Yoga Study 301 to 357 Aphorism 40 to 44 Pious Behaviour Indication 358 to 362 Steps Perfection 363 to 370 Part III Appendix : Glossary of Technical Terms 373 to 395 References 396 G YOGA INFLUENCE PART I YOGA INFLUENCE INDEX Subject Page No. -
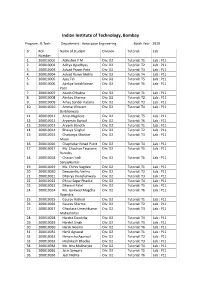
Rolllist Btech DD Bs2020batch
Indian Institute of Technology, Bombay Program : B.Tech. Department : Aerospace Engineering Batch Year : 2020 Sr. Roll Name of Student Division Tutorial Lab Number 1. 200010001 Abhishek P M Div: D2 Tutorial: T1 Lab : P11 2. 200010002 Aditya Upadhyay Div: D2 Tutorial: T2 Lab : P11 3. 200010003 Advait Pravin Pote Div: D2 Tutorial: T3 Lab : P11 4. 200010004 Advait Ranvir Mehla Div: D2 Tutorial: T4 Lab : P11 5. 200010005 Ajay Tak Div: D2 Tutorial: T5 Lab : P11 6. 200010006 Ajinkya Satishkumar Div: D2 Tutorial: T6 Lab : P11 Patil 7. 200010007 Akash Chhabra Div: D2 Tutorial: T1 Lab : P11 8. 200010008 Akshay Sharma Div: D2 Tutorial: T2 Lab : P11 9. 200010009 Amay Sunder Kataria Div: D2 Tutorial: T3 Lab : P11 10. 200010010 Ammar Khozem Div: D2 Tutorial: T4 Lab : P11 Barbhaiwala 11. 200010011 Anup Nagdeve Div: D2 Tutorial: T5 Lab : P11 12. 200010012 Aryaman Bansal Div: D2 Tutorial: T6 Lab : P11 13. 200010013 Aryank Banoth Div: D2 Tutorial: T1 Lab : P11 14. 200010014 Bhavya Singhal Div: D2 Tutorial: T2 Lab : P11 15. 200010015 Chaitanya Shankar Div: D2 Tutorial: T3 Lab : P11 Moon 16. 200010016 Chaphekar Ninad Punit Div: D2 Tutorial: T4 Lab : P11 17. 200010017 Ms. Chauhan Tejaswini Div: D2 Tutorial: T5 Lab : P11 Ramdas 18. 200010018 Chavan Yash Div: D2 Tutorial: T6 Lab : P11 Sanjaykumar 19. 200010019 Ms. Chinni Vagdevi Div: D2 Tutorial: T1 Lab : P11 20. 200010020 Deepanshu Verma Div: D2 Tutorial: T2 Lab : P11 21. 200010021 Dhairya Jhunjhunwala Div: D2 Tutorial: T3 Lab : P11 22. 200010022 Dhruv Sagar Phadke Div: D2 Tutorial: T4 Lab : P11 23. 200010023 Dhwanil Patel Div: D2 Tutorial: T5 Lab : P11 24. -

Use of Theses
THESES SIS/LIBRARY TELEPHONE: +61 2 6125 4631 R.G. MENZIES LIBRARY BUILDING NO:2 FACSIMILE: +61 2 6125 4063 THE AUSTRALIAN NATIONAL UNIVERSITY EMAIL: [email protected] CANBERRA ACT 0200 AUSTRALIA USE OF THESES This copy is supplied for purposes of private study and research only. Passages from the thesis may not be copied or closely paraphrased without the written consent of the author. THE PRATYUTPANNA-BUDDHA-SAMMUKHAVASTHITA- SAMADHI-SUTRA AN ANNOTATED ENGLISH TRANSLATION OF THE TIBETAN VERSION WITH SEVERAL APPENDICES A Thesis submitted for the Degree of Doctor of Philosophy in the Australian National University August, 1979 by Paul Harrison This thesis is based on my own research carried out from 1976 to 1979 at the Australian National University. ABSTRACT The present work consists of a study of the Pratyutpanna-buddha- sammukhavasthita-samadhi-sutra (hereafter: PraS), a relatively early example of Mahayana Buddhist canonical literature. After a brief Intro duction (pp. xxi-xli), which attempts to place the PraS in its historical context, the major portion of the work (pp. 1-186) is devoted to an annotated English translation of the Tibetan version of the sutra, with detailed reference to the three main Chinese translations. Appendix A (pp. 187-252) then attempts a resolution of some of the many problems surrounding the various Chinese versions of the PraS. These are examined both from the point of view of internal evidence and on the basis of bibliographical information furnished by the Chinese Buddhist scripture-catalogues. Some tentative conclusions are advanced concerning the textual history of the PraS in China. -

In Search of a Global Theosophical India in Tarakishore Choudhury's
Bharatbhoomi Punyabhoomi: In Search of a Global Theosophical India in Tarakishore Choudhury’s Writings Author: Arkamitra Ghatak Stable URL: http://www.globalhistories.com/index.php/GHSJ/article/view/105 DOI: http://dx.doi.org/10.17169/GHSJ.2017.105 Source: Global Histories, Vol. 3, No. 1 (Apr. 2017), pp. 39–61 ISSN: 2366-780X Copyright © 2017 Arkamitra Ghatak License URL: https://creativecommons.org/licenses/by/4.0/ Publisher information: ‘Global Histories: A Student Journal’ is an open-access bi-annual journal founded in 2015 by students of the M.A. program Global History at Freie Universität Berlin and Humboldt-Universität zu Berlin. ‘Global Histories’ is published by an editorial board of Global History students in association with the Freie Universität Berlin. Freie Universität Berlin Global Histories: A Student Journal Friedrich-Meinecke-Institut Koserstraße 20 14195 Berlin Contact information: For more information, please consult our website www.globalhistories.com or contact the editor at: [email protected]. Bharatbhoomi Punyabhoomi: In Search of a Global Theosophical India in Tarakishore Choudhury’s Writings ARKAMITRA GHATAK Arkamitra Ghatak completed her major in History at Presidency University, Kolkata, in 2016, securing the first rank in the order of merit and was awarded the Gold Medal for Academic Ex- cellence. She is currently pursuing a Master in History at Presidency University. Her research interests include intellectual history in its plural spatialities, expressions of feminine subjec- tivities and spiritualities, as well as articulations of power and piety in cultural performances, especially folk festivals. She has presented several research papers at international student seminars organized at Presidency University, Jadavpur University and other organizations. -

Modern-Baby-Names.Pdf
All about the best things on Hindu Names. BABY NAMES 2016 INDIAN HINDU BABY NAMES Share on Teweet on FACEBOOK TWITTER www.indianhindubaby.com Indian Hindu Baby Names 2016 www.indianhindubaby.com Table of Contents Baby boy names starting with A ............................................................................................................................... 4 Baby boy names starting with B ............................................................................................................................. 10 Baby boy names starting with C ............................................................................................................................. 12 Baby boy names starting with D ............................................................................................................................. 14 Baby boy names starting with E ............................................................................................................................. 18 Baby boy names starting with F .............................................................................................................................. 19 Baby boy names starting with G ............................................................................................................................. 19 Baby boy names starting with H ............................................................................................................................. 22 Baby boy names starting with I .............................................................................................................................. -

Curriculum Vitae
Curriculum Vitae 1 Name : Mrs. Durga Khatri 2 Designation : Asst. Professor 3 Department : College Education 4 Education Qualification : Level Name of University Year Title/ Remark/ Medal M A MDS University Ajmer 1998 NET UGC 2000 5 Teaching / Research Experience: UG 17.5 Years PG 9 Years Research nil 6 Membership (Academic Bodies): Nil 7 Academic Courses Attended: Course Place Duration Sponsoring Agency Orientation Course jodhpur Jnv 28 days(11.7.2005 to6.8.2005) uni.johpur jodhpur ‘’ 21 days (14.8.2006 to3.9.2006) Refresher jodhpur “ 21 days (31.10.2011 to 19.11.2011) MDSUNI Ajmer 21 days(11.12.2013to 31.12.2013 Ajmer Other (Workshop/ short term course RAJ Summer School/ jaipur 6 days( 3.8.2015to8.82015) Camp etc.) uni.jaipur 1 8 Seminar/ Conference attended: Internat./ Attended/ Name of Seminar/ National/ Paper Title of Paper Date Conference Regional Presented Sansdiy loktantra National conference Paper National Feb 11-12 2006 GOVT. college Barmer presented me girte naitik mulya RGA National conference. Papar Power potential from National 26oct-28oct.2015 GOVT.college Ajmer presented soyabean husk International seminar Paper Rajasthan me aadivasi janjati international Aug.9-10 2016 JNV Uni. Jodhpur presented samuday ;ek vishleshan Rashtriya sangoshthi Vaidik vagnmay me Rajasthan Sanskrit National attened Feb 6-7 2016 paryavaran sanrashan Akadami International conference Paper Guru Jambheshwer international Geeta me Rajniti Dec. 8-10 2016 presented uni.Hisar . Rashtriya Sangoshthi Bharat me Mahila Paper SGSG Govt.college National Manvadhikaron ka Jan. 9,2017 presented Nasirabad sanrakshan Teerth paryatan ke vikas me Rashtriya Sangoshthi Paper 30 Nov.-1 National sarkar ki bhumika evam Govt. -

The Realisation of the Absolute
THE REALISATION OF THE ABSOLUTE SWAMI KRISHNANANDA The Divine Life Society Sivananda Ashram, Rishikesh, India Website: www.swami-krishnananda.org ABOUT THIS EDITION Though this eBook edition is designed primarily for digital readers and computers, it works well for print too. Page size dimensions are 5.5" x 8.5", or half a regular size sheet, and can be printed for personal, non-commercial use: two pages to one side of a sheet by adjusting your printer settings. 2 CONTENTS Publishers’ Note ........................................................................................ 4 Foreword ..................................................................................................... 5 Preface .......................................................................................................... 7 Chapter One: Introduction .................................................................. 13 Chapter Two: The Nature of the World ......................................... 26 Chapter Three: The Need for Integral Knowledge .................... 53 Chapter Four: The Nature of Reality .............................................. 66 Chapter Five: The Process of Truth-Realisation ......................122 Chapter Six: The Attainment of Liberation ................................163 Chapter Seven: Conclusion ...............................................................190 Explanatory Notes ................................................................................195 Notes ..........................................................................................................207 -

Satsanga and Svadhyaya
SATSANGA AND SVADHYAYA The Glory, the Importance and the Life-transforming Power of Holy Company and Spiritual Books. By SRI SWAMI SIVANANDA SERVE, LOVE, GIVE, PURIFY, MEDITATE, REALIZE Sri Swami Sivananda So Says Founder of Sri Swami Sivananda The Divine Life Society A DIVINE LIFE SOCIETY PUBLICATION First Edition: 1965 Sixteenth Edition: 1996 (3,000 Copies) World Wide Web (WWW) Edition: 2000 WWW site: http://www.SivanandaDlshq.org/ This WWW reprint is for free distribution © The Divine Life Trust Society ISBN 81-7052-125-4 Published By THE DIVINE LIFE SOCIETY P.O. SHIVANANDANAGAR—249 192 Distt. Tehri-Garhwal, Uttar Pradesh, Himalayas, India. PUBLISHERS’ NOTE This book offers, between the covers of one volume, the varied writings of H.H. Sri Swami Sivanandaji Maharaj on the subject of Satsanga or holy company and the related topic of Svadhyaya or daily study of sacred literature. The second part of the book throws more light on the subject. Therein Swami Chidanandaji Maharaj analyses in detail the subtle connection and the subtle distinction between the company of a holy man and the company of the Guru and points out clearly the circumstances under which Satsanga can prove most fruitful for the Sadhaka. It is a slightly abstract subject, but one which is vital for all spiritual seekers. It is our sincere hope that the pages that follow will open up a glorious new chapter in the lives of many. THE DIVINE LIFE SOCIETY s:ts:ög:tv:ð en:Hs:ög:tv:ö en:Hs:ög:tv:ð en:m::ðühtv:m:Î . -

The Seventy-Five Dharmas (Elements of Existence) in the Abhidharmakosa of Vasubandhu
The Seventy-Five Dharmas (Elements of Existence) in the Abhidharmakosa of Vasubandhu Created Elements, Samskrta-dharma (Dharmas 1-72) I. Forms, Rupani Sense Organs 1. eye, caksu 2. ear, srotra 3. nose, ghrana 4. tongue, jihva 5. body, kaya Sense Objects 6. form, rupa 7. sound, sabda 8. smell, gandha 9. taste. rasa 10. touch, sprastavya 11. element with no manifestation, avijnapti-rupa II. Mind, Citta 12. Mind, Citta III. Concomitant Mental Faculties, Caitasika or Citta-samprayukta-samskara A. General Functions, Mahabhumika 13. feeling, sensation, vedana 14. conception, idea, samjna 15. will, volition, cetana 16. touch, contact, sparsa 17. wish, chanda 18. intellect, mati 19. mindfulness, smrti 20. attention, manaskara 21. decision, abhimoksa 22. concentration, samadhi B. General Functions of Good, Kusala-mahabhumika 23. faith, sraddha 24. energy, effort, virya 25. equanimity, upeksa 26. self respect, shame, hri 27. decorum, apatrapya 28. non-greediness, alobha 29. non-ill-will, advesa 30. non-violence, non-harm, ahimsa 31. confidence, prasrabdhi 32. exertion, apramada C. General Functions of Defilement, Klesa mahabhumika 33. ignorance, moha 34. idleness, non-diligence, pramada 35. indolence, idleness vs. virya, kausidya 36. non-belief, asraddhya 37. low-mindedness, torpor, styana 38. high-mindedness, restlessness, dissipation, auddhatya D. General Functions of Evil, Akusala-mahabhumika 39. lack of self-respect, shamelessness, ahrikya 40. lack of decorum, anapatrapya E. Minor Functions of Defilement, Upaklesa-bhumika 41. anger, krodha 42. concealment, hypocrisy, mraksa 43. parsimony, matsarya 44. jealousy, envy, irsya 45. affliction, pradasa 46. violence, harm, vihimsa 47. enmity, breaking friend, upanaha 48. deceit, maya 49. fraudulence, perfidy, sathya 50. arrogance, mada F. -
Journal-2021-Final-1.Pdf
Journal of Mental Health Education The Journal of Mental Health Education is the official publication of The Department of Mental Health Education, NIMHANS. The journal is peer-reviewed, is published annually, and accepts high-quality work or writings in the broad fields of mental, neurological and neurosurgical health and promotion. The journal is being published through funding from the Dr. RN Moorthy Foundation. With the goal of dissemination of knowledge to increase the wider public awareness of mental health and to promote research in the field Mental Health Education, the Department of Mental Health Education publishes the Journal of Mental Health Education, a peer-reviewed online Journal with Annual print compilation of issues. The first issue of the journal was published in 2017 under the Editorship of Prof. S.K. Chaturvedi and Dr. Meena K.S. Further details about the Department of Mental Health Education and its activities are available at http://mentalhealtheducationnimhans.org/ Journal Ethics The Journal is committed to meeting and upholding the standards of ethical behavior at all stages of the publication process. We follow closely the industry associations, such as the Committee on Publication Ethics (COPE), International Committee of Medical Journal Editors (ICMJE) and World Association of Medical Editors (WAME), that set standards and provide guidelines for the best practices in order to meet these requirements. Open Access Publication and Creative Commons Licensing This is an open access Journal and articles are distributed under the terms of the Creative Commons Attributions-Non-Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credits is given and the new creations are licensed under the identical terms. -

The Bodhisattva Ideal in Selected Buddhist
i THE BODHISATTVA IDEAL IN SELECTED BUDDHIST SCRIPTURES (ITS THEORETICAL & PRACTICAL EVOLUTION) YUAN Cl Thesis Submitted for the Degree of Doctor of Philosophy School of Oriental and African Studies University of London 2004 ProQuest Number: 10672873 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 10672873 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 Abstract This thesis consists of seven chapters. It is designed to survey and analyse the teachings of the Bodhisattva ideal and its gradual development in selected Buddhist scriptures. The main issues relate to the evolution of the teachings of the Bodhisattva ideal. The Bodhisattva doctrine and practice are examined in six major stages. These stages correspond to the scholarly periodisation of Buddhist thought in India, namely (1) the Bodhisattva’s qualities and career in the early scriptures, (2) the debates concerning the Bodhisattva in the early schools, (3) the early Mahayana portrayal of the Bodhisattva and the acceptance of the six perfections, (4) the Bodhisattva doctrine in the earlier prajhaparamita-siltras\ (5) the Bodhisattva practices in the later prajnaparamita texts, and (6) the evolution of the six perfections (paramita) in a wide range of Mahayana texts. -

State District Branch Address Centre Ifsc Contact1 Contact2 Contact3 Micr Code
STATE DISTRICT BRANCH ADDRESS CENTRE IFSC CONTACT1 CONTACT2 CONTACT3 MICR_CODE ANDAMAN NO 26. MG ROAD AND ABERDEEN BAZAR , NICOBAR PORT BLAIR -744101 704412829 704412829 ISLAND ANDAMAN PORT BLAIR ,A & N ISLANDS PORT BLAIR IBKL0001498 8 7044128298 8 744259002 UPPER GROUND FLOOR, #6-5-83/1, ANIL ANIL NEW BUS STAND KUMAR KUMAR ANDHRA ROAD, BHUKTAPUR, 897889900 ANIL KUMAR 897889900 PRADESH ADILABAD ADILABAD ADILABAD 504001 ADILABAD IBKL0001090 1 8978899001 1 1ST FLOOR, 14- 309,SREERAM ENCLAVE,RAILWAY FEDDER ROADANANTAPURA ANDHRA NANTAPURANDHRA ANANTAPU 08554- PRADESH ANANTAPUR ANANTAPUR PRADESH R IBKL0000208 270244 D.NO.16-376,MARKET STREET,OPPOSITE CHURCH,DHARMAVA RAM- 091 ANDHRA 515671,ANANTAPUR DHARMAVA 949497979 PRADESH ANANTAPUR DHARMAVARAM DISTRICT RAM IBKL0001795 7 515259202 SRINIVASA SRINIVASA IDBI BANK LTD, 10- RAO RAO 43, BESIDE SURESH MYLAPALL SRINIVASA MYLAPALL MEDICALS, RAILWAY I - RAO I - ANDHRA STATION ROAD, +91967670 MYLAPALLI - +91967670 PRADESH ANANTAPUR GUNTAKAL GUNTAKAL - 515801 GUNTAKAL IBKL0001091 6655 +919676706655 6655 18-1-138, M.F.ROAD, AJACENT TO ING VYSYA BANK, HINDUPUR , ANANTAPUR DIST - 994973715 ANDHRA PIN:515 201 9/98497191 PRADESH ANANTAPUR HINDUPUR ANDHRA PRADESH HINDUPUR IBKL0001162 17 515259102 AGRICULTURE MARKET COMMITTEE, ANANTAPUR ROAD, TADIPATRI, 085582264 ANANTAPUR DIST 40 ANDHRA PIN : 515411 /903226789 PRADESH ANANTAPUR TADIPATRI ANDHRA PRADESH TADPATRI IBKL0001163 2 515259402 BUKARAYASUNDARA M MANDAL,NEAR HP GAS FILLING 91 ANDHRA STATION,ANANTHAP ANANTAPU 929710487 PRADESH ANANTAPUR VADIYAMPETA UR