Subcutaneous Phaeohyphomycosis Caused by Exophiala Salmonis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exophiala Jeanselmei, with a Case Report and in Vitro Antifungal Susceptibility of the Species
UvA-DARE (Digital Academic Repository) Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives Badali, H. Publication date 2010 Link to publication Citation for published version (APA): Badali, H. (2010). Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:02 Oct 2021 Chapter 6 The clinical spectrum of Exophiala jeanselmei, with a case report and in vitro antifungal susceptibility of the species H. Badali 1, 2, 3, M.J. Najafzadeh 1, 2, M. van Esbroeck 4, E. van den Enden 4, B. Tarazooie 1, J.F.G.M. Meis 5, G.S. de Hoog 1, 2 1CBS-KNAW Fungal Biodiversity Centre, Utrecht, The Netherlands, 2Institute of Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands, 3Department of Medical Mycology and Parasitology, School of Medicine/Molecular and Cell Biology Research Centre, Mazandaran University of Medical Sciences, Sari, Iran, 4Institute of Tropical Medicine, Nationalestraat 155, 2000 Antwerp, Belgium,5Department of Medical Microbiology and Infectious Diseases, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands. -

Indoor Wet Cells As a Habitat for Melanized Fungi, Opportunistic
www.nature.com/scientificreports OPEN Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other Received: 23 June 2017 Accepted: 30 April 2018 vertebrates Published: xx xx xxxx Xiaofang Wang1,2, Wenying Cai1, A. H. G. Gerrits van den Ende3, Junmin Zhang1, Ting Xie4, Liyan Xi1,5, Xiqing Li1, Jiufeng Sun6 & Sybren de Hoog3,7,8,9 Indoor wet cells serve as an environmental reservoir for a wide diversity of melanized fungi. A total of 313 melanized fungi were isolated at fve locations in Guangzhou, China. Internal transcribed spacer (rDNA ITS) sequencing showed a preponderance of 27 species belonging to 10 genera; 64.22% (n = 201) were known as human opportunists in the orders Chaetothyriales and Venturiales, potentially causing cutaneous and sometimes deep infections. Knufa epidermidis was the most frequently encountered species in bathrooms (n = 26), while in kitchens Ochroconis musae (n = 14), Phialophora oxyspora (n = 12) and P. europaea (n = 10) were prevalent. Since the majority of species isolated are common agents of cutaneous infections and are rarely encountered in the natural environment, it is hypothesized that indoor facilities explain the previously enigmatic sources of infection by these organisms. Black yeast-like and other melanized fungi are frequently isolated from clinical specimens and are known as etiologic agents of a gamut of opportunistic infections, but for many species their natural habitat is unknown and hence the source and route of transmission remain enigmatic. Te majority of clinically relevant black yeast-like fungi belong to the order Chaetothyriales, while some belong to the Venturiales. Propagules are mostly hydro- philic1 and reluctantly dispersed by air, infections mostly being of traumatic origin. -

Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm)
Editorial | Journal of Gandaki Medical College-Nepal Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm) Reddy KR Professor & Head Microbiology Department Gandaki Medical College & Teaching Hospital, Pokhara, Nepal Medical Mycology, a study of fungal epidemiology, ecology, pathogenesis, diagnosis, prevention and treatment in human beings, is a newly recognized discipline of biomedical sciences, advancing rapidly. Earlier, the fungi were believed to be mere contaminants, commensals or nonpathogenic agents but now these are commonly recognized as medically relevant organisms causing potentially fatal diseases. The discipline of medical mycology attained recognition as an independent medical speciality in the world sciences in 1910 when French dermatologist Journal of Raymond Jacques Adrien Sabouraud (1864 - 1936) published his seminal treatise Les Teignes. This monumental work was a comprehensive account of most of then GANDAKI known dermatophytes, which is still being referred by the mycologists. Thus he MEDICAL referred as the “Father of Medical Mycology”. COLLEGE- has laid down the foundation of the field of Medical Mycology. He has been aptly There are significant developments in treatment modalities of fungal infections NEPAL antifungal agent available. Nystatin was discovered in 1951 and subsequently and we have achieved new prospects. However, till 1950s there was no specific (J-GMC-N) amphotericin B was introduced in 1957 and was sanctioned for treatment of human beings. In the 1970s, the field was dominated by the azole derivatives. J-GMC-N | Volume 10 | Issue 01 developed to treat fungal infections. By the end of the 20th century, the fungi have Now this is the most active field of interest, where potential drugs are being January-June 2017 been reported to be developing drug resistance, especially among yeasts. -
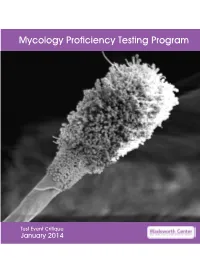
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2013 Mycology Laboratory Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 15 Mold Descriptions 16 M-1 Exserohilum species 16 M-2 Phialophora species 20 M-3 Chrysosporium species 25 M-4 Fusarium species 30 M-5 Rhizopus species 34 Yeast Descriptions 38 Y-1 Rhodotorula mucilaginosa 38 Y-2 Trichosporon asahii 41 Y-3 Candida glabrata 44 Y-4 Candida albicans 47 Y-5 Geotrichum candidum 50 Direct Detection - Cryptococcal Antigen 53 Antifungal Susceptibility Testing - Yeast 55 Antifungal Susceptibility Testing - Mold (Educational) 60 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Changing Taxonomic Concepts and Their Impact on Nomenclatural Stability
Journal of Medical and Veterinary Mycology (1994), 32, Supplement 1, 113-122 Changing taxonomic concepts and their impact on nomenclatural stability G. S. DE HOOG 1, L. SIGLER 2, W. A. UNTEREINER 3, K. J. KWON-CHUNG 4, E. GUI~HO 5 AND J. M. J. UIJTHOF 1 1Centraalbureau voor Schimmelcultures, Baarn, The Netherlands," 2 University of Alberta Microfungus Collection, Edmonton, and 3Department of Botany, University of Toronto, Toronto, Canada," 4Clinical Mycology Section, National Institute of Health, Bethesda, USA; and s Unitd de Mycologie, Institut Pasteur, France Experimental techniques, which are routinely applied in yeast systematics, are currently finding recognition in a growing number of filamentous taxa. Some other biochemical markers have recently been developed in hyphomycete taxonomy. The spectrum of potential criteria now comprises characters of coenzyme-Q systems, secondary metabo- lites, protein electrophoresis, serology, nuclear (n) DNA/DNA reassociation, mole% G+C of DNA, protein electrophoresis, nutritional physiology and ultrastructural and karyological data. In addition, a wide range of molecular techniques is gaining rapid acceptance in evolutionary, systematic, ecological and epidemiological studies. Depend- ing on the aim of the study, partial DNA sequencing (mainly of SS and LS ribosomal genes and their spacers, but also of other genes), PCR-ribotyping and mitochondrial (mt) DNA restriction analyses are particularly powerful; for the establishment of the taxo- nomic position of taxa, 5.8S ribosomal (r) rRNA sequencing and Southern blotting with conserved genes are useful. Together with renewed in-depth morphological studies and the elucidation of teleomorph connections and (syn)anamorph life cycles, these tech- For personal use only. niques provide tools for an improved understanding of the phylogeny and ecological role of the distinguished taxa. -

Update July 4, 2018 BIBLIOGRAPHY: 1. Todd JR, Matsumoto T, Ueno R
Update July 4, 2018 BIBLIOGRAPHY: 1. Todd JR, Matsumoto T, Ueno R. Murugayan J, Britten A, King JW, Odaka Y, Oberle A, Weise C, Roesler U, Pore RS. 2018. Medical phycology 2017. Medical Mycology. 56(Suppl. 1):S118-S204. 2. Noguchi H, Hiruma M, Matsumoto T, Kano R, Ihn H. 2017. Ungual aspergillosis successfully treated with topical efinaconazole. J. Dermatol. 44:8-90. 3. Noguchi H, Hiruma M, Matsumoto T. Yaguchi T, Tashima H, Ihn H. 2017. Multiple subcutaneous Candida abscesses on the palm and finger in an immunocompetent patient. J. Dermatol. 44:e176-e177. 4. Noguchi H, Hiruma M, Matsumoto T, Kano R, Tanaka M, Yaguchi T, Sonoda K, Ihn H. 2017. Fungal melanonychia: Ungual phaeohyphomycosis caused by Botryosphaera dothidea. Acta Dermato-Venereologica. 97:765-766. 5. Noguchi H, Hiruma M, Matsumoto T, Yaguchi T, Sano A, Mitsui N, Watanabe S, Ihn H. 2017. Subcutaneous cystic phaeohyphomycosis due to Pleurostomophora richardsiae. J. Dermatol. 44:e62-e63. 6. Noguchi H, Hiruma M, Matsumoto T, Kano R, Ihn H. 2016. Ungual hyalohyphomycosis caused by Fusarium proliferatum in an immunocompetent patient. J. Dermatol. 44:848-850. 7. Todd JR, King JW, Oberle A, Matsumoto T, Odaka Y, Fowler M, Pore RS, Shahan TA, Yin L, Sanusi ID. 2012. Protothecosis: Report of a case with 20-year follow- up, and review of previously published cases. Med. Mycol. 50:673-689. 8. Matsumoto T, Cooper Jr. CR, Szaniszlo PJ. 2011. Chromoblastomycosis and phaeohyphomycosis. In: Tropical Infectious Diseases: Principles, Pathogens, and Practice, Third Edition, One Volume Set with Web site, Edited by Guerrant RL, Walker DH, Weller PF., Elsevier, Edingburgh, U.K., pp.569-572. -

Exophiala Spinifera and Its Allies: Diagnostics from 109 Morphology to DNA Barcoding
UvA-DARE (Digital Academic Repository) Developing species recognition and diagnostics of rare opportunistic fungi Zeng, J. Publication date 2007 Document Version Final published version Link to publication Citation for published version (APA): Zeng, J. (2007). Developing species recognition and diagnostics of rare opportunistic fungi. IBED. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:01 Oct 2021 Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Opportunistic Rare of Diagnostics and Recognition Species Developing Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Jingsi Zeng Jingsi Zeng Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Jingsi Zeng Promotor Prof. Dr. G.S. de Hoog Centraalbureau voor Schimmelcultures Fungal Biodiversity Centre, Royal Netherlands Academy of Arts and Sciences Institute for Biodiversity and Ecosystem Dynamics, University of Amsterdam Co-promotor Dr. -

Fungal Infections
Fungal infections Natural defence against fungi y Fatty acid content of the skin y pH of the skin, mucosal surfaces and body fluids y Epidermal turnover y Normal flora Predisposing factors y Tropical climate y Manual labour population y Low socioeconomic status y Profuse sweating y Friction with clothes, synthetic innerwear y Malnourishment y Immunosuppressed patients HIV, Congenital Immunodeficiencies, patients on corticosteroids, immunosuppressive drugs, Diabetes Fungal infections: Classification y Superficial cutaneous: y Surface infections eg. P.versicolor, Dermatophytosis, Candidiasis, T.nigra, Piedra y Subcutaneous: Mycetoma, Chromoblastomycosis, Sporotrichosis y Systemic: (opportunistic infection) Histoplasmosis, Candidiasis Of these categories, Dermatophytosis, P.versicolor, Candidiasis are common in daily practice Pityriasis versicolor y Etiologic agent: Malassezia furfur Clinical features: y Common among youth y Genetic predisposition, familial occurrence y Multiple, discrete, discoloured, macules. y Fawn, brown, grey or hypopigmented y Pinhead sized to large sheets of discolouration y Seborrheic areas, upper half of body: trunk, arms, neck, abdomen. y Scratch sign positive PITYRIASIS VERSICOLOR P.versicolor : Investigations y Wood’s Lamp examination: y Yellow fluorescence y KOH preparation: Spaghetti and meatball appearance Coarse mycelium, fragmented to short filaments 2-5 micron wide and up to 2-5 micron long, together with spherical, thick-walled yeasts 2-8 micron in diameter, arranged in grape like fashion. P.versicolor: Differential diagnosis y Vitiligo y Pityriasis rosea y Secondary syphilis y Seborrhoeic dermatitis y Erythrasma y Melasma Treatment P. versicolor Topical: y Ketoconazole , Clotrimazole, Miconazole, Bifonazole, Oxiconazole, Butenafine,Terbinafine, Selenium sulfide, Sodium thiosulphate Oral: y Fluconazole 400mg single dose y Ketoconazole 200mg OD x 14days yGriseofulvin is NOT effective. -

Trinidad and Tobago, Denning, Mycoses, 2015
mycoses Diagnosis,Therapy and Prophylaxis of Fungal Diseases Supplement article Burden of serious fungal infections in Trinidad and Tobago David W. Denning1,2 and Harish C. Gugnani3 1The University of Manchester, Manchester Academic Health Science Centre, Manchester, UK, 2National Aspergillosis Centre, The University Hospital of South Manchester, Manchester, UK and 3Microbiology and Epidemiology, Saint James School of Medicine, Kralendjik, Bonaire Dutch Caribbean Summary The information on the prevalence of fungal infections in the Caribbean region including Trinidad and Tobago (population 1 339 000 million) is scanty. Tinea capi- tis is common in children, being predominant in those of African descent, with no definitive estimate. Asthma is also common affecting 77 000–139 000 adults with an estimated 1927–3491 affected by allergic bronchopulmonary aspergillosis (ABPA) and 2544–4608 with severe asthma and fungal sensitisation (SAFS). An estimated 23 763 women have ≥4 attacks of vaginal candidiasis annually. Among the estimated 14 000 HIV-infected patients, 750 cases of oesophageal candidiasis, 400 cases of Pneumocystis pneumonia (PCP) and 50 cases of cryptococcal meningi- tis are anticipated. Histoplasma capsulatum is endemic in the islands with a 49% skin positivity rate in those <60 years old. Three cases of cutaneous histoplasmosis in AIDS patients have been reported. Three cases of pulmonary histoplasmosis were reported among German biologists following exposure to bats in a cave in Trinidad. Using a low mean international incidence figure for candidaemia of 5/100 000, 67 cases of candidaemia are estimated. The burden of fungal infections in Trinidad and Tobago is considerable and requires appropriate diagnostic and clinical expertise. -

Phaeohyphomycosis Caused by Exophiala Species in Immunocompromised Hosts
Phaeohyphomycosis Caused by Exophiala Species PHAEOHYPHOMYCOSIS CAUSED BY EXOPHIALA SPECIES IN IMMUNOCOMPROMISED HOSTS Jyh-Ming Liou,1 Jann-Tay Wang,1,4 Min-Hshi Wang,1,4 Shei-Shen Wang,3 and Po-Ren Hsueh1,2 Abstract: Exophiala species are rarely implicated in clinical diseases. In the past 2 years, (J Formos Med Assoc we have treated phaeohyphomycosis caused by Exophiala species in three 2002;101:523–6) immunocompromised patients. Two of these patients presented with subcutaneous abscess or cutaneous verrucous lesions due to Exophiala jeanselmei. The former, an Key words: 81-year-old woman, had pulmonary tuberculosis and the latter, a 62-year-old man, phaeohyphomycosis had undergone heart transplantation and was receiving immunosuppressive Exophiala jeanselmei treatment. The third patient, a 62-year-old woman, had acute lymphoblastic leukemia Wangiella dermatitidis and developed lymphadenitis due to Wangiella (Exophiala) dermatitidis. In each case, the fungus was discovered on a Gram stain of the aspirated material and was identified by conventional tests. One patient died of bacterial pneumonia with acute respiratory distress syndrome and the other two were treated successfully with surgical excision and antifungal agents. With the more frequent and widespread use of immunosup- pressive agents, the incidence of Exophiala infection will certainly increase. Surgical excision or debridement with or without antifungal agents may offer the possibility of cure for phaeohyphomycosis due to Exophiala species. Exophiala species were first identified on the island of [8], patients treated with steroids [9], and healthy Martinique (West Indies) by Jeanselme in 1928 [1]. individuals [10]. Nosocomial Exophiala jeanselmei They belong to the dematiaceous group of fungi and pseudoinfection involving 16 patients after sonography- are widely distributed in the environment, especially in guided aspiration of thoracic lesions has also been soil, wood, and other plant matter [1, 2]. -

Subcutaneous Phaeohyphomycosis Caused by Exophiala Jeanselmei in an Immunocompromised Host
Subcutaneous Phaeohyphomycosis Caused by Exophiala jeanselmei in an Immunocompromised Host Jenifer Hague, MD; Elizabeth Liotta, MD Phaeohyphomycosis is an infection caused by dematiaceous fungi, which are ubiquitous throughout the world. We present the case of a 41-year-old immunocompromised man with Cushing syndrome who developed a phaeohypho- mycotic infection. The patient presented with painful, progressive nodules that were biopsied and cultured to reveal dematiaceous fungi. Treatment of this condition is particularly difficult as demonstrated by this patient’s intolerance to itraconazole and amphotericin B. Because of the increasing number of immunocompromised patients and incidence of phaeohyphomycosis, a heightened level of suspicion is necessary on the part of the clinician for both diagnosis and treatment of this disease. Cutis. 2003;72:132-134. Case Report Figure 1. Individual nodular lesion with central ulceration. A 41-year-old white man with steroid-dependent reactive airway disease complicated by iatrogenic Cushing syndrome presented to the dermatology clinic with a 6-month history of progressive skin hands and right forearm. The lesions expressed a lesions, occurring at the sites of trauma (Figure 1). yellow discharge when manipulated. No erythema or The patient was maintained on inhaled steroids and adenopathy was noted. Microscopic evaluation of oral prednisone, varying in dose from 20 to 100 mg biopsy specimens revealed pseudoepitheliomatous daily dependent on respiratory symptoms, for his hyperplasia and dematiaceous fungi. Cultures were respiratory disease. positive for Exophiala jeanselmei (Figure 2). Slides of The findings from the physical examination the fungi were prepared with Gomori methenamine- revealed a characteristic cushingoid male, with ten- silver (Figure 3) and Fontana-Masson stains.