A Case of Exophiala Oligosperma Successfully Treated with Voriconazole$
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phaeoseptaceae, Pleosporales) from China
Mycosphere 10(1): 757–775 (2019) www.mycosphere.org ISSN 2077 7019 Article Doi 10.5943/mycosphere/10/1/17 Morphological and phylogenetic studies of Pleopunctum gen. nov. (Phaeoseptaceae, Pleosporales) from China Liu NG1,2,3,4,5, Hyde KD4,5, Bhat DJ6, Jumpathong J3 and Liu JK1*,2 1 School of Life Science and Technology, University of Electronic Science and Technology of China, Chengdu 611731, P.R. China 2 Guizhou Key Laboratory of Agricultural Biotechnology, Guizhou Academy of Agricultural Sciences, Guiyang 550006, P.R. China 3 Faculty of Agriculture, Natural Resources and Environment, Naresuan University, Phitsanulok 65000, Thailand 4 Center of Excellence in Fungal Research, Mae Fah Luang University, Chiang Rai 57100, Thailand 5 Mushroom Research Foundation, Chiang Rai 57100, Thailand 6 No. 128/1-J, Azad Housing Society, Curca, P.O., Goa Velha 403108, India Liu NG, Hyde KD, Bhat DJ, Jumpathong J, Liu JK 2019 – Morphological and phylogenetic studies of Pleopunctum gen. nov. (Phaeoseptaceae, Pleosporales) from China. Mycosphere 10(1), 757–775, Doi 10.5943/mycosphere/10/1/17 Abstract A new hyphomycete genus, Pleopunctum, is introduced to accommodate two new species, P. ellipsoideum sp. nov. (type species) and P. pseudoellipsoideum sp. nov., collected from decaying wood in Guizhou Province, China. The genus is characterized by macronematous, mononematous conidiophores, monoblastic conidiogenous cells and muriform, oval to ellipsoidal conidia often with a hyaline, elliptical to globose basal cell. Phylogenetic analyses of combined LSU, SSU, ITS and TEF1α sequence data of 55 taxa were carried out to infer their phylogenetic relationships. The new taxa formed a well-supported subclade in the family Phaeoseptaceae and basal to Lignosphaeria and Thyridaria macrostomoides. -

Genomic Analysis of Ant Domatia-Associated Melanized Fungi (Chaetothyriales, Ascomycota) Leandro Moreno, Veronika Mayer, Hermann Voglmayr, Rumsais Blatrix, J
Genomic analysis of ant domatia-associated melanized fungi (Chaetothyriales, Ascomycota) Leandro Moreno, Veronika Mayer, Hermann Voglmayr, Rumsais Blatrix, J. Benjamin Stielow, Marcus Teixeira, Vania Vicente, Sybren de Hoog To cite this version: Leandro Moreno, Veronika Mayer, Hermann Voglmayr, Rumsais Blatrix, J. Benjamin Stielow, et al.. Genomic analysis of ant domatia-associated melanized fungi (Chaetothyriales, Ascomycota). Mycolog- ical Progress, Springer Verlag, 2019, 18 (4), pp.541-552. 10.1007/s11557-018-01467-x. hal-02316769 HAL Id: hal-02316769 https://hal.archives-ouvertes.fr/hal-02316769 Submitted on 15 Oct 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Mycological Progress (2019) 18:541–552 https://doi.org/10.1007/s11557-018-01467-x ORIGINAL ARTICLE Genomic analysis of ant domatia-associated melanized fungi (Chaetothyriales, Ascomycota) Leandro F. Moreno1,2,3 & Veronika Mayer4 & Hermann Voglmayr5 & Rumsaïs Blatrix6 & J. Benjamin Stielow3 & Marcus M. Teixeira7,8 & Vania A. Vicente3 & Sybren de Hoog1,2,3,9 Received: 20 August 2018 /Revised: 16 December 2018 /Accepted: 19 December 2018 # The Author(s) 2019 Abstract Several species of melanized (Bblack yeast-like^) fungi in the order Chaetothyriales live in symbiotic association with ants inhabiting plant cavities (domatia) or with ants that use carton-like material for the construction of nests and tunnels. -
Subcutaneous Phaeohyphomycosis Caused by Exophiala Salmonis
Case Report Clinical Microbiology Ann Lab Med 2012;32:438-441 http://dx.doi.org/10.3343/alm.2012.32.6.438 ISSN 2234-3806 • eISSN 2234-3814 Subcutaneous Phaeohyphomycosis Caused by Exophiala salmonis Young Ahn Yoon, M.D.1, Kyung Sun Park, M.D.1, Jang Ho Lee, M.T.1, Ki-Sun Sung, M.D.2, Chang-Seok Ki, M.D.1, and Nam Yong Lee, M.D.1 Departments of Laboratory Medicine and Genetics1, Orthopedic Surgery2, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea We report a case of subcutaneous infection in a 55-yr-old Korean diabetic patient who Received: June 18, 2012 presented with a cystic mass of the ankle. Black fungal colonies were observed after cul- Revision received: July 30, 2012 Accepted: September 12, 2012 turing on blood and Sabouraud dextrose agar. On microscopic observation, septated ellip- soidal or cylindrical conidia accumulating on an annellide were visualized after staining Corresponding author: Nam Yong Lee Department of Laboratory Medicine and with lactophenol cotton blue. The organism was identified as Exophiala salmonis by se- Genetics, Samsung Medical Center, quencing of the ribosomal DNA internal transcribed spacer region. Phaeohyphomycosis is 81 Irwon-ro, Gangnam-gu, Seoul 135-710, a heterogeneous group of mycotic infections caused by dematiaceous fungi and is com- Korea Tel: +82-2-3410–2706 monly associated with immunocompromised patients. The most common clinical mani- Fax: +82-2-3410–2719 festations of subcutaneous lesions are abscesses or cystic masses. To the best of our E-mail: [email protected] knowledge, this is the first reported case in Korea of subcutaneous phaeohyphomycosis caused by E. -

Diversity of Biodeteriorative Bacterial and Fungal Consortia in Winter and Summer on Historical Sandstone of the Northern Pergol
applied sciences Article Diversity of Biodeteriorative Bacterial and Fungal Consortia in Winter and Summer on Historical Sandstone of the Northern Pergola, Museum of King John III’s Palace at Wilanow, Poland Magdalena Dyda 1,2,* , Agnieszka Laudy 3, Przemyslaw Decewicz 4 , Krzysztof Romaniuk 4, Martyna Ciezkowska 4, Anna Szajewska 5 , Danuta Solecka 6, Lukasz Dziewit 4 , Lukasz Drewniak 4 and Aleksandra Skłodowska 1 1 Department of Geomicrobiology, Institute of Microbiology, Faculty of Biology, University of Warsaw, Miecznikowa 1, 02-096 Warsaw, Poland; [email protected] 2 Research and Development for Life Sciences Ltd. (RDLS Ltd.), Miecznikowa 1/5a, 02-096 Warsaw, Poland 3 Laboratory of Environmental Analysis, Museum of King John III’s Palace at Wilanow, Stanislawa Kostki Potockiego 10/16, 02-958 Warsaw, Poland; [email protected] 4 Department of Environmental Microbiology and Biotechnology, Institute of Microbiology, Faculty of Biology, University of Warsaw, Miecznikowa 1, 02-096 Warsaw, Poland; [email protected] (P.D.); [email protected] (K.R.); [email protected] (M.C.); [email protected] (L.D.); [email protected] (L.D.) 5 The Main School of Fire Service, Slowackiego 52/54, 01-629 Warsaw, Poland; [email protected] 6 Department of Plant Molecular Ecophysiology, Institute of Experimental Plant Biology and Biotechnology, Faculty of Biology, University of Warsaw, Miecznikowa 1, 02-096 Warsaw, Poland; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +48-786-28-44-96 Citation: Dyda, M.; Laudy, A.; Abstract: The aim of the presented investigation was to describe seasonal changes of microbial com- Decewicz, P.; Romaniuk, K.; munity composition in situ in different biocenoses on historical sandstone of the Northern Pergola in Ciezkowska, M.; Szajewska, A.; the Museum of King John III’s Palace at Wilanow (Poland). -

Exophiala Jeanselmei, with a Case Report and in Vitro Antifungal Susceptibility of the Species
UvA-DARE (Digital Academic Repository) Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives Badali, H. Publication date 2010 Link to publication Citation for published version (APA): Badali, H. (2010). Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:02 Oct 2021 Chapter 6 The clinical spectrum of Exophiala jeanselmei, with a case report and in vitro antifungal susceptibility of the species H. Badali 1, 2, 3, M.J. Najafzadeh 1, 2, M. van Esbroeck 4, E. van den Enden 4, B. Tarazooie 1, J.F.G.M. Meis 5, G.S. de Hoog 1, 2 1CBS-KNAW Fungal Biodiversity Centre, Utrecht, The Netherlands, 2Institute of Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands, 3Department of Medical Mycology and Parasitology, School of Medicine/Molecular and Cell Biology Research Centre, Mazandaran University of Medical Sciences, Sari, Iran, 4Institute of Tropical Medicine, Nationalestraat 155, 2000 Antwerp, Belgium,5Department of Medical Microbiology and Infectious Diseases, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands. -

Indoor Wet Cells As a Habitat for Melanized Fungi, Opportunistic
www.nature.com/scientificreports OPEN Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other Received: 23 June 2017 Accepted: 30 April 2018 vertebrates Published: xx xx xxxx Xiaofang Wang1,2, Wenying Cai1, A. H. G. Gerrits van den Ende3, Junmin Zhang1, Ting Xie4, Liyan Xi1,5, Xiqing Li1, Jiufeng Sun6 & Sybren de Hoog3,7,8,9 Indoor wet cells serve as an environmental reservoir for a wide diversity of melanized fungi. A total of 313 melanized fungi were isolated at fve locations in Guangzhou, China. Internal transcribed spacer (rDNA ITS) sequencing showed a preponderance of 27 species belonging to 10 genera; 64.22% (n = 201) were known as human opportunists in the orders Chaetothyriales and Venturiales, potentially causing cutaneous and sometimes deep infections. Knufa epidermidis was the most frequently encountered species in bathrooms (n = 26), while in kitchens Ochroconis musae (n = 14), Phialophora oxyspora (n = 12) and P. europaea (n = 10) were prevalent. Since the majority of species isolated are common agents of cutaneous infections and are rarely encountered in the natural environment, it is hypothesized that indoor facilities explain the previously enigmatic sources of infection by these organisms. Black yeast-like and other melanized fungi are frequently isolated from clinical specimens and are known as etiologic agents of a gamut of opportunistic infections, but for many species their natural habitat is unknown and hence the source and route of transmission remain enigmatic. Te majority of clinically relevant black yeast-like fungi belong to the order Chaetothyriales, while some belong to the Venturiales. Propagules are mostly hydro- philic1 and reluctantly dispersed by air, infections mostly being of traumatic origin. -

Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm)
Editorial | Journal of Gandaki Medical College-Nepal Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm) Reddy KR Professor & Head Microbiology Department Gandaki Medical College & Teaching Hospital, Pokhara, Nepal Medical Mycology, a study of fungal epidemiology, ecology, pathogenesis, diagnosis, prevention and treatment in human beings, is a newly recognized discipline of biomedical sciences, advancing rapidly. Earlier, the fungi were believed to be mere contaminants, commensals or nonpathogenic agents but now these are commonly recognized as medically relevant organisms causing potentially fatal diseases. The discipline of medical mycology attained recognition as an independent medical speciality in the world sciences in 1910 when French dermatologist Journal of Raymond Jacques Adrien Sabouraud (1864 - 1936) published his seminal treatise Les Teignes. This monumental work was a comprehensive account of most of then GANDAKI known dermatophytes, which is still being referred by the mycologists. Thus he MEDICAL referred as the “Father of Medical Mycology”. COLLEGE- has laid down the foundation of the field of Medical Mycology. He has been aptly There are significant developments in treatment modalities of fungal infections NEPAL antifungal agent available. Nystatin was discovered in 1951 and subsequently and we have achieved new prospects. However, till 1950s there was no specific (J-GMC-N) amphotericin B was introduced in 1957 and was sanctioned for treatment of human beings. In the 1970s, the field was dominated by the azole derivatives. J-GMC-N | Volume 10 | Issue 01 developed to treat fungal infections. By the end of the 20th century, the fungi have Now this is the most active field of interest, where potential drugs are being January-June 2017 been reported to be developing drug resistance, especially among yeasts. -
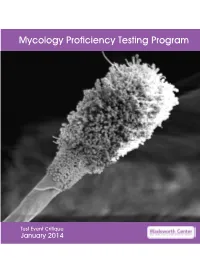
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Fungal Diversity in Lichens: from Extremotolerance to Interactions with Algae
life Review Fungal Diversity in Lichens: From Extremotolerance to Interactions with Algae Lucia Muggia 1,* ID and Martin Grube 2 1 Department of Life Sciences, University of Trieste, via Licio Giorgieri 10, 34127 Trieste, Italy 2 Institute of Biology, Karl-Franzens University of Graz, Holteigasse 6, 8010 Graz, Austria; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +39-040-558-8825 Received: 11 April 2018; Accepted: 21 May 2018; Published: 22 May 2018 Abstract: Lichen symbioses develop long-living thallus structures even in the harshest environments on Earth. These structures are also habitats for many other microscopic organisms, including other fungi, which vary in their specificity and interaction with the whole symbiotic system. This contribution reviews the recent progress regarding the understanding of the lichen-inhabiting fungi that are achieved by multiphasic approaches (culturing, microscopy, and sequencing). The lichen mycobiome comprises a more or less specific pool of species that can develop symptoms on their hosts, a generalist environmental pool, and a pool of transient species. Typically, the fungal classes Dothideomycetes, Eurotiomycetes, Leotiomycetes, Sordariomycetes, and Tremellomycetes predominate the associated fungal communities. While symptomatic lichenicolous fungi belong to lichen-forming lineages, many of the other fungi that are found have close relatives that are known from different ecological niches, including both plant and animal pathogens, and rock colonizers. A significant fraction of yet unnamed melanized (‘black’) fungi belong to the classes Chaethothyriomycetes and Dothideomycetes. These lineages tolerate the stressful conditions and harsh environments that affect their hosts, and therefore are interpreted as extremotolerant fungi. Some of these taxa can also form lichen-like associations with the algae of the lichen system when they are enforced to symbiosis by co-culturing assays. -

A Worldwide List of Endophytic Fungi with Notes on Ecology and Diversity
Mycosphere 10(1): 798–1079 (2019) www.mycosphere.org ISSN 2077 7019 Article Doi 10.5943/mycosphere/10/1/19 A worldwide list of endophytic fungi with notes on ecology and diversity Rashmi M, Kushveer JS and Sarma VV* Fungal Biotechnology Lab, Department of Biotechnology, School of Life Sciences, Pondicherry University, Kalapet, Pondicherry 605014, Puducherry, India Rashmi M, Kushveer JS, Sarma VV 2019 – A worldwide list of endophytic fungi with notes on ecology and diversity. Mycosphere 10(1), 798–1079, Doi 10.5943/mycosphere/10/1/19 Abstract Endophytic fungi are symptomless internal inhabits of plant tissues. They are implicated in the production of antibiotic and other compounds of therapeutic importance. Ecologically they provide several benefits to plants, including protection from plant pathogens. There have been numerous studies on the biodiversity and ecology of endophytic fungi. Some taxa dominate and occur frequently when compared to others due to adaptations or capabilities to produce different primary and secondary metabolites. It is therefore of interest to examine different fungal species and major taxonomic groups to which these fungi belong for bioactive compound production. In the present paper a list of endophytes based on the available literature is reported. More than 800 genera have been reported worldwide. Dominant genera are Alternaria, Aspergillus, Colletotrichum, Fusarium, Penicillium, and Phoma. Most endophyte studies have been on angiosperms followed by gymnosperms. Among the different substrates, leaf endophytes have been studied and analyzed in more detail when compared to other parts. Most investigations are from Asian countries such as China, India, European countries such as Germany, Spain and the UK in addition to major contributions from Brazil and the USA. -

Environmental Prospecting of Black Yeast-Like Agents of Human Disease
www.nature.com/scientificreports OPEN Environmental prospecting of black yeast‑like agents of human disease using culture‑independent methodology Flávia de Fátima Costa1, Nickolas Menezes da Silva1, Morgana Ferreira Voidaleski2, Vinicius Almir Weiss2, Leandro Ferreira Moreno2, Gabriela Xavier Schneider2, Mohammad J. Najafzadeh3, Jiufeng Sun4, Renata Rodrigues Gomes2, Roberto Tadeu Raittz5, Mauro Antonio Alves Castro5, Graciela Bolzón Inez de Muniz6, G. Sybren de Hoog2,7* & Vania Aparecida Vicente1,2* Melanized fungi and black yeasts in the family Herpotrichiellaceae (order Chaetothyriales) are important agents of human and animal infectious diseases such as chromoblastomycosis and phaeohyphomycosis. The oligotrophic nature of these fungi enables them to survive in adverse environments where common saprobes are absent. Due to their slow growth, they lose competition with common saprobes, and therefore isolation studies yielded low frequencies of clinically relevant species in environmental habitats from which humans are thought to be infected. This problem can be solved with metagenomic techniques which allow recognition of microorganisms independent from culture. The present study aimed to identify species of the family Herpotrichiellaceae that are known to occur in Brazil by the use of molecular markers to screen public environmental metagenomic datasets from Brazil available in the Sequence Read Archive (SRA). Species characterization was performed with the BLAST comparison of previously described barcodes and padlock probe sequences. A total of 18,329 sequences was collected comprising the genera Cladophialophora, Exophiala, Fonsecaea, Rhinocladiella and Veronaea, with a focus on species related to the chromoblastomycosis. The data obtained in this study demonstrated presence of these opportunists in the investigated datasets. The used techniques contribute to our understanding of environmental occurrence and epidemiology of black fungi. -

Exophiala Spinifera and Its Allies: Diagnostics from 109 Morphology to DNA Barcoding
UvA-DARE (Digital Academic Repository) Developing species recognition and diagnostics of rare opportunistic fungi Zeng, J. Publication date 2007 Document Version Final published version Link to publication Citation for published version (APA): Zeng, J. (2007). Developing species recognition and diagnostics of rare opportunistic fungi. IBED. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:01 Oct 2021 Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Opportunistic Rare of Diagnostics and Recognition Species Developing Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Jingsi Zeng Jingsi Zeng Developing Species Recognition and Diagnostics of Rare Opportunistic Fungi Jingsi Zeng Promotor Prof. Dr. G.S. de Hoog Centraalbureau voor Schimmelcultures Fungal Biodiversity Centre, Royal Netherlands Academy of Arts and Sciences Institute for Biodiversity and Ecosystem Dynamics, University of Amsterdam Co-promotor Dr.