Phaeohyphomycosis Caused by Exophiala Species in Immunocompromised Hosts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Subcutaneous Phaeohyphomycosis Caused by Exophiala Salmonis
Case Report Clinical Microbiology Ann Lab Med 2012;32:438-441 http://dx.doi.org/10.3343/alm.2012.32.6.438 ISSN 2234-3806 • eISSN 2234-3814 Subcutaneous Phaeohyphomycosis Caused by Exophiala salmonis Young Ahn Yoon, M.D.1, Kyung Sun Park, M.D.1, Jang Ho Lee, M.T.1, Ki-Sun Sung, M.D.2, Chang-Seok Ki, M.D.1, and Nam Yong Lee, M.D.1 Departments of Laboratory Medicine and Genetics1, Orthopedic Surgery2, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea We report a case of subcutaneous infection in a 55-yr-old Korean diabetic patient who Received: June 18, 2012 presented with a cystic mass of the ankle. Black fungal colonies were observed after cul- Revision received: July 30, 2012 Accepted: September 12, 2012 turing on blood and Sabouraud dextrose agar. On microscopic observation, septated ellip- soidal or cylindrical conidia accumulating on an annellide were visualized after staining Corresponding author: Nam Yong Lee Department of Laboratory Medicine and with lactophenol cotton blue. The organism was identified as Exophiala salmonis by se- Genetics, Samsung Medical Center, quencing of the ribosomal DNA internal transcribed spacer region. Phaeohyphomycosis is 81 Irwon-ro, Gangnam-gu, Seoul 135-710, a heterogeneous group of mycotic infections caused by dematiaceous fungi and is com- Korea Tel: +82-2-3410–2706 monly associated with immunocompromised patients. The most common clinical mani- Fax: +82-2-3410–2719 festations of subcutaneous lesions are abscesses or cystic masses. To the best of our E-mail: [email protected] knowledge, this is the first reported case in Korea of subcutaneous phaeohyphomycosis caused by E. -

MULTI-DISCIPLINE REVIEW Summary Review Office Director Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208901Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multi-disciplinary Review and Evaluation – NDA 208901 NDA 208901: Multi-Disciplinary Review and Evaluation Application Type NDA Application Number(s) 208901 Priority or Standard Standard Submit Date(s) February 16, 2018 Received Date(s) February 16, 2018 PDUFA Goal Date December 16, 2018 Division Division of Anti-Infective Products Review Completion Date November 28, 2018 Established Name Itraconazole (Proposed) Trade Name TOLSURA Pharmacologic Class Azole antifungal Code name SUBA-itraconazole Applicant Mayne Pharma International Pty Ltd. Formulation(s) Oral capsule-65 mg Dosing Regimen 130 mg to 260 mg daily Applicant Proposed Treatment of the following fungal infections in Indication(s)/Population(s) immunocompromised and non-immunocompromised patients: 1) Blastomycosis, pulmonary and extrapulmonary 2) Histoplasmosis, including chronic cavitary pulmonary disease and disseminated, non-meningeal histoplasmosis, and 3) Aspergillosis, pulmonary and extrapulmonary, in patients who are intolerant of or who are refractory to Amphotericin B therapy. (b) (4) Regulatory Action Approval Approved Treatment of the following fungal infections in Indication(s)/Population(s) immunocompromised and non-immunocompromised adult patients: x Blastomycosis, pulmonary and extrapulmonary x Histoplasmosis, including chronic cavitary pulmonary -

Exophiala Jeanselmei, with a Case Report and in Vitro Antifungal Susceptibility of the Species
UvA-DARE (Digital Academic Repository) Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives Badali, H. Publication date 2010 Link to publication Citation for published version (APA): Badali, H. (2010). Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:02 Oct 2021 Chapter 6 The clinical spectrum of Exophiala jeanselmei, with a case report and in vitro antifungal susceptibility of the species H. Badali 1, 2, 3, M.J. Najafzadeh 1, 2, M. van Esbroeck 4, E. van den Enden 4, B. Tarazooie 1, J.F.G.M. Meis 5, G.S. de Hoog 1, 2 1CBS-KNAW Fungal Biodiversity Centre, Utrecht, The Netherlands, 2Institute of Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands, 3Department of Medical Mycology and Parasitology, School of Medicine/Molecular and Cell Biology Research Centre, Mazandaran University of Medical Sciences, Sari, Iran, 4Institute of Tropical Medicine, Nationalestraat 155, 2000 Antwerp, Belgium,5Department of Medical Microbiology and Infectious Diseases, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands. -

Indoor Wet Cells As a Habitat for Melanized Fungi, Opportunistic
www.nature.com/scientificreports OPEN Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other Received: 23 June 2017 Accepted: 30 April 2018 vertebrates Published: xx xx xxxx Xiaofang Wang1,2, Wenying Cai1, A. H. G. Gerrits van den Ende3, Junmin Zhang1, Ting Xie4, Liyan Xi1,5, Xiqing Li1, Jiufeng Sun6 & Sybren de Hoog3,7,8,9 Indoor wet cells serve as an environmental reservoir for a wide diversity of melanized fungi. A total of 313 melanized fungi were isolated at fve locations in Guangzhou, China. Internal transcribed spacer (rDNA ITS) sequencing showed a preponderance of 27 species belonging to 10 genera; 64.22% (n = 201) were known as human opportunists in the orders Chaetothyriales and Venturiales, potentially causing cutaneous and sometimes deep infections. Knufa epidermidis was the most frequently encountered species in bathrooms (n = 26), while in kitchens Ochroconis musae (n = 14), Phialophora oxyspora (n = 12) and P. europaea (n = 10) were prevalent. Since the majority of species isolated are common agents of cutaneous infections and are rarely encountered in the natural environment, it is hypothesized that indoor facilities explain the previously enigmatic sources of infection by these organisms. Black yeast-like and other melanized fungi are frequently isolated from clinical specimens and are known as etiologic agents of a gamut of opportunistic infections, but for many species their natural habitat is unknown and hence the source and route of transmission remain enigmatic. Te majority of clinically relevant black yeast-like fungi belong to the order Chaetothyriales, while some belong to the Venturiales. Propagules are mostly hydro- philic1 and reluctantly dispersed by air, infections mostly being of traumatic origin. -

Cerebral Phaeohyphomycosis: a Rare Case from South India
July 2020, Vol 6, Issue 3, No 22 Case Report: Cerebral Phaeohyphomycosis: A Rare Case from South India M. G. Sabarinadh1* , Josey T Verghese1 , Suma Job1 1. Department of Radiodiagnosis, Radiodiagnosis Medical Council of India, Government T D Medical College, Alappuzha, India Use your device to scan and read the article online Citation: Sabarinadh MG, Verghese JT, Job S. Cerebral Phaeohyphomycosis: A Rare Case from South India. Iran J Neurosurg. 2020; 6(3):155-160. http://dx.doi.org/10.32598/irjns.6.3.7 : http://dx.doi.org/10.32598/irjns.6.3.7 A B S T R A C T Background and Importance: Cerebral phaeohyphomycosis is a rare but frequently fatal Article info: clinical entity caused by dematiaceous fungi like Cladophialophora bantiana. Fungal brain Received: 10 Jan 2020 abscess often presents with subtle clinical symptoms and signs, and present diagnostic dilemma due to its imaging appearance that may be indistinguishable from other intracranial Accepted: 23 May 2020 space-occupying lesions. Still, certain imaging patterns on Computed Tomography (CT) and 01 Jul 2020 Available Online: Magnetic Resonance Imaging (MRI) help to narrow down the differential diagnosis and initiate prompt treatment of these infections. Case Presentation: A 48-year-old immunocompetent man presented with right-sided hemiparesis and hemisensory loss and a provisional diagnosis of stroke was made. The radiological evaluation suggested the possibility of a cerebral abscess. Accordingly, surgical excision of the lesion was performed and the histopathological examination of the specimen revealed the etiology as phaeohyphomycosis. The patient was further treated with antifungals and discharged when general conditions improved. -

Case Report Fábio Muradás Girardi1, Anderson Lima Da Rocha2, Mireille Angelo Bernardes Sousa2, Michelle Virginia Eidt3
Case Report http://dx.doi.org/10.4322/2357-9730.74514 FULMINANT AURICULAR MUCORMYCOSIS IN A DIABETIC PATIENT Fábio Muradás Girardi1, Anderson Lima da Rocha2, Mireille Angelo Bernardes Sousa2, Michelle Virginia Eidt3 ABSTRACT Clin Biomed Res. 2017;37(4):362-365 Human mucormycosis is an atypical fungal infection that commonly affects the skin, 1 Head and Neck Surgery Department, but rarely the auricular region. A 32-year-old diabetic woman, agricultural worker, Ana Nery Hospital. Santa Cruz do Sul, was admitted with swelling, redness and mild signs of epidermolysis of the left ear, RS, Brazil. associated with intense pain, facial paralysis and septic signs. The ear cellulitis evolved into necrosis of the same region on the following day. Surgical debridement 2 Laboratório Hermes Pardini. Belo was performed and antimycotic therapy was started with poor response. The patient Horizonte, MG, Brazil. died in 48h. Culture was confirmatory for Rhizopus sp. Keywords: Mucormycosis; fungal infections; diabetes; Rhizopus 3 Department of Clinical Medicine, Ana Nery Hospital. Santa Cruz do Sul, RS, Brazil. Mucormycosis is a rare but aggressive fungal infection, which occurs most often among patients with diabetes mellitus and other immunosuppressed individuals1. Most cases are associated to Rhizopus sp, a genus of common Corresponding author: Fábio Muradás Girardi saprophytic fungi on plants and decaying organic matter. Most human infections [email protected] are rhinocerebral and sinopulmonary. Cutaneous mucormycosis are also Head and Neck Department, Ana Nery frequent and generally result from direct inoculation of fungal spores in the Hospital skin through any kind of injury, causing tissue necrosis by angioinvasion. Rua Pereira da Cunha, 209. -

Application to Add Itraconazole and Voriconazole to the Essential List of Medicines for Treatment of Fungal Diseases – Support Document
Application to add itraconazole and voriconazole to the essential list of medicines for treatment of fungal diseases – Support document 1 | Page Contents Page number Summary 3 Centre details supporting the application 3 Information supporting the public health relevance and review of 4 benefits References 7 2 | Page 1. Summary statement of the proposal for inclusion, change or deletion As a growing trend of invasive fungal infections has been noticed worldwide, available few antifungal drugs requires to be used optimally. Invasive aspergillosis, systemic candidiasis, chronic pulmonary aspergillosis, fungal rhinosinusitis, allergic bronchopulmonary aspergillosis, phaeohyphomycosis, histoplasmosis, sporotrichosis, chromoblastomycosis, and relapsed cases of dermatophytosis are few important concern of southeast Asian regional area. Considering the high burden of fungal diseases in Asian countries and its associated high morbidity and mortality (often exceeding 50%), we support the application of including major antifungal drugs against filamentous fungi, itraconazole and voriconazole in the list of WHO Essential Medicines (both available in oral formulation). The inclusion of these oral effective antifungal drugs in the essential list of medicines (EML) would help in increased availability of these agents in this part of the world and better prompt management of patients thereby reducing mortality. The widespread availability of these drugs would also stimulate more research to facilitate the development of better combination therapies. -

Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm)
Editorial | Journal of Gandaki Medical College-Nepal Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm) Reddy KR Professor & Head Microbiology Department Gandaki Medical College & Teaching Hospital, Pokhara, Nepal Medical Mycology, a study of fungal epidemiology, ecology, pathogenesis, diagnosis, prevention and treatment in human beings, is a newly recognized discipline of biomedical sciences, advancing rapidly. Earlier, the fungi were believed to be mere contaminants, commensals or nonpathogenic agents but now these are commonly recognized as medically relevant organisms causing potentially fatal diseases. The discipline of medical mycology attained recognition as an independent medical speciality in the world sciences in 1910 when French dermatologist Journal of Raymond Jacques Adrien Sabouraud (1864 - 1936) published his seminal treatise Les Teignes. This monumental work was a comprehensive account of most of then GANDAKI known dermatophytes, which is still being referred by the mycologists. Thus he MEDICAL referred as the “Father of Medical Mycology”. COLLEGE- has laid down the foundation of the field of Medical Mycology. He has been aptly There are significant developments in treatment modalities of fungal infections NEPAL antifungal agent available. Nystatin was discovered in 1951 and subsequently and we have achieved new prospects. However, till 1950s there was no specific (J-GMC-N) amphotericin B was introduced in 1957 and was sanctioned for treatment of human beings. In the 1970s, the field was dominated by the azole derivatives. J-GMC-N | Volume 10 | Issue 01 developed to treat fungal infections. By the end of the 20th century, the fungi have Now this is the most active field of interest, where potential drugs are being January-June 2017 been reported to be developing drug resistance, especially among yeasts. -
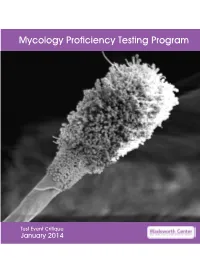
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Phaeohyphomycosis Caused by Coniothyrium
Phaeohyphomycosis Caused by Coniothyrium Kimberly Siu, BA; Allan K. Izumi, MD A 49-year-old immunosuppressed heart trans- plant recipient developed a superficial and subcu- taneous granulomatous infection caused by Coniothyrium. The patient responded to a combi- nation of surgical excision and antifungal agents. We review phaeohyphomycotic infections including this second report of a Coniothyrium infection. Cutis. 2004;73:127-130. haeohyphomycosis is a group of mycotic infec- tions caused by dematiaceous fungi. Ajello P coined the term phaeohyphomycosis to distin- guish it from chromoblastomycosis.1 The infection may present as superficial cutaneous, subcutaneous, or systemic infections that typically are introduced into the skin by trauma in individuals who are either immunocompetent or immunocompro- mised.1,2 Coniothyrium is a type of phaeohyphomy- cotic infection in humans and is a saprophytic fungus that causes disease in roses and sugar cane.3 This is a report of an immunosuppressed heart transplant recipient with diabetes with both a superficial and deep granulomatous infection caused by Coniothyrium. To our knowledge, the only other report of Coniothyrium causing human infection was found in a patient with acute myelog- enous leukemia.3 Case Report A 49-year-old immunocompromised male heart transplant recipient with diabetes presented to our clinic. He was on a therapeutic regimen of azathio- prine, mycophenolate mofetil, cyclosporine, pred- nisone, and insulin and had an 8-month history of gradually enlarging granulomatous annular and Figure 1. Granulomatous nodular and subcutaneous nodular plaques on his legs and knees. His history plaques on the legs. also was significant for a cytomegalovirus infection and disseminated herpes zoster. -
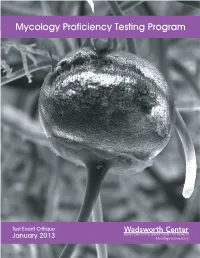
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2013 Mycology Laboratory Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 15 Mold Descriptions 16 M-1 Exserohilum species 16 M-2 Phialophora species 20 M-3 Chrysosporium species 25 M-4 Fusarium species 30 M-5 Rhizopus species 34 Yeast Descriptions 38 Y-1 Rhodotorula mucilaginosa 38 Y-2 Trichosporon asahii 41 Y-3 Candida glabrata 44 Y-4 Candida albicans 47 Y-5 Geotrichum candidum 50 Direct Detection - Cryptococcal Antigen 53 Antifungal Susceptibility Testing - Yeast 55 Antifungal Susceptibility Testing - Mold (Educational) 60 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Changing Taxonomic Concepts and Their Impact on Nomenclatural Stability
Journal of Medical and Veterinary Mycology (1994), 32, Supplement 1, 113-122 Changing taxonomic concepts and their impact on nomenclatural stability G. S. DE HOOG 1, L. SIGLER 2, W. A. UNTEREINER 3, K. J. KWON-CHUNG 4, E. GUI~HO 5 AND J. M. J. UIJTHOF 1 1Centraalbureau voor Schimmelcultures, Baarn, The Netherlands," 2 University of Alberta Microfungus Collection, Edmonton, and 3Department of Botany, University of Toronto, Toronto, Canada," 4Clinical Mycology Section, National Institute of Health, Bethesda, USA; and s Unitd de Mycologie, Institut Pasteur, France Experimental techniques, which are routinely applied in yeast systematics, are currently finding recognition in a growing number of filamentous taxa. Some other biochemical markers have recently been developed in hyphomycete taxonomy. The spectrum of potential criteria now comprises characters of coenzyme-Q systems, secondary metabo- lites, protein electrophoresis, serology, nuclear (n) DNA/DNA reassociation, mole% G+C of DNA, protein electrophoresis, nutritional physiology and ultrastructural and karyological data. In addition, a wide range of molecular techniques is gaining rapid acceptance in evolutionary, systematic, ecological and epidemiological studies. Depend- ing on the aim of the study, partial DNA sequencing (mainly of SS and LS ribosomal genes and their spacers, but also of other genes), PCR-ribotyping and mitochondrial (mt) DNA restriction analyses are particularly powerful; for the establishment of the taxo- nomic position of taxa, 5.8S ribosomal (r) rRNA sequencing and Southern blotting with conserved genes are useful. Together with renewed in-depth morphological studies and the elucidation of teleomorph connections and (syn)anamorph life cycles, these tech- For personal use only. niques provide tools for an improved understanding of the phylogeny and ecological role of the distinguished taxa.