OHNEP Oral Health Case Study Resource
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An 8-Year-Old Boy with Fever, Splenomegaly, and Pancytopenia
An 8-Year-Old Boy With Fever, Splenomegaly, and Pancytopenia Rachel Offenbacher, MD,a,b Brad Rybinski, BS,b Tuhina Joseph, DO, MS,a,b Nora Rahmani, MD,a,b Thomas Boucher, BS,b Daniel A. Weiser, MDa,b An 8-year-old boy with no significant past medical history presented to his abstract pediatrician with 5 days of fever, diffuse abdominal pain, and pallor. The pediatrician referred the patient to the emergency department (ED), out of concern for possible malignancy. Initial vital signs indicated fever, tachypnea, and tachycardia. Physical examination was significant for marked abdominal distension, hepatosplenomegaly, and abdominal tenderness in the right upper and lower quadrants. Initial laboratory studies were notable for pancytopenia as well as an elevated erythrocyte sedimentation rate and C-reactive protein. aThe Children’s Hospital at Montefiore, Bronx, New York; and bAlbert Einstein College of Medicine, Bronx, New York Computed tomography (CT) of the abdomen and pelvis showed massive splenomegaly. The only significant history of travel was immigration from Dr Offenbacher led the writing of the manuscript, recruited various specialists for writing the Albania 10 months before admission. The patient was admitted to a tertiary manuscript, revised all versions of the manuscript, care children’s hospital and was evaluated by hematology–oncology, and was involved in the care of the patient; infectious disease, genetics, and rheumatology subspecialty teams. Our Mr Rybinski contributed to the writing of the multidisciplinary panel of experts will discuss the evaluation of pancytopenia manuscript and critically revised the manuscript; Dr Joseph contributed to the writing of the manuscript, with apparent multiorgan involvement and the diagnosis and appropriate cared for the patient, and was critically revised all management of a rare disease. -

Case Report Gastric Volvulus Due to Splenomegaly - a Rare Entity
Case Report Gastric Volvulus Due to Splenomegaly - A rare Entity. Ashok Mhaske Department of Surgery,People’s College of Medical Sciences and Research Centre, Bhanpur, Bhopal. 462010 , (M.P.) Abstract: Gastric volvulus is a rare condition which typically presents with intermittent episodes of abdominal pain. The volvulus occurs around an axis made by two fixed points, organo-axial or mesentero-axial. Increased pressure within the hernial sac associated with gastric distension can lead to ischemia and perforation. Acute obstruction of a gastric volvulus is thus a surgical emergency.We present an unusual case of gastric volvulus secondary to tropical splenomegaly. Tropical splenomegaly precipitating gastric volvulus is not documented till date. Key Words: Gastric volvulus, Tropical splenomegaly. Introduction: to general practitioner but as symptoms persisted she Gastric volvulus is abnormal rotation of the was referred to our tertiary care centre for expert stomach of more than 180 degrees. It can cause closed opinion and management. loop obstrcution and at times can result in On examination, vital parameters and hydration was adequate with marked tenderness in incarceration and strangulation. Berti first described epigastric region with vague lump. Her routine gastric volvulus in 1866; to date, it remains a rare investigations were inconclusive but she did partially clinical entity. Berg performed the first successful responded to antispasmodic and antacid drugs. operation on a patient with gastric volvulus in 1896. Ultrasound of abdomen and Barium studies Borchardt (1904) described the classic triad of severe revealed gastric volvulus (Fig.1 & 2) with epigastric pain, retching without vomiting and splenomegaly for which she was taken up for inability to pass a nasogastric tube. -
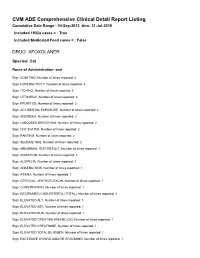
FDA CVM Comprehensive ADE Report Listing for Afoxolaner
CVM ADE Comprehensive Clinical Detail Report Listing Cumulative Date Range : 04-Sep-2013 -thru- 31-Jul-2018 Included 1932a cases = : True Included Medicated Feed cases = : False DRUG: AFOXOLANER Species: Cat Route of Administration: oral Sign: VOMITING, Number of times reported: 4 Sign: HYPERACTIVITY, Number of times reported: 3 Sign: ITCHING, Number of times reported: 3 Sign: LETHARGY, Number of times reported: 3 Sign: PRURITUS, Number of times reported: 3 Sign: ACCIDENTAL EXPOSURE, Number of times reported: 2 Sign: ANOREXIA, Number of times reported: 2 Sign: LABOURED BREATHING, Number of times reported: 2 Sign: NOT EATING, Number of times reported: 2 Sign: PANTING, Number of times reported: 2 Sign: SEIZURE NOS, Number of times reported: 2 Sign: ABNORMAL TEST RESULT, Number of times reported: 1 Sign: AGITATION, Number of times reported: 1 Sign: ALOPECIA, Number of times reported: 1 Sign: ANAEMIA NOS, Number of times reported: 1 Sign: ATAXIA, Number of times reported: 1 Sign: CERVICAL VENTROFLEXION, Number of times reported: 1 Sign: CONSTIPATION, Number of times reported: 1 Sign: DECREASED CHOLESTEROL (TOTAL), Number of times reported: 1 Sign: ELEVATED ALT, Number of times reported: 1 Sign: ELEVATED AST, Number of times reported: 1 Sign: ELEVATED BUN, Number of times reported: 1 Sign: ELEVATED CREATINE-KINASE (CK), Number of times reported: 1 Sign: ELEVATED CREATININE, Number of times reported: 1 Sign: ELEVATED TOTAL BILIRUBIN, Number of times reported: 1 Sign: EXCESSIVE LICKING AND/OR GROOMING, Number of times reported: 1 Sign: FEVER, -

General Anesthesia Complicated by Perioperative Iatrogenic Splenic Rupture
GENERAL ANESTHESIA COMPLICATED BY PERIOPERATIVE IATROGENIC SPLENIC RUPTURE JEREMY ASNIS* AND STEVEN M. NEUSTEIN** Abstract Patients with splenomegaly often present with diverse coexisting medical disease and thus offer a variety of anesthetic considerations. The challenges that come with splenectomy have also become increasingly common to the anesthesiologist, given the growing number of indications for surgical intervention including both benign and malignant disease. Removal of the spleen is associated with numerous intraoperative and postoperative risks, including massive intraoperative hemorrhage, perioperative coagulation abnormalities, and post-splenectomy infection1. When caring for the patient with an enlarged spleen scheduled for splenectomy, the anesthetic plan must address both patient and procedure specific concerns. We present a medically challenging case of a 28 year old man with splenomegaly secondary to lymphoma, who underwent elective splenectomy, which was complicated by perioperative splenic rupture and hemorrhage. Key words: splenomegaly, intraoperative rupture. Introduction Patients with splenomegaly often present with diverse coexisting medical disease and thus offer a variety of anesthetic considerations. The challenges that come with splenectomy have also become increasingly common to the anesthesiologist, given the growing number of indications for surgical intervention including both benign and malignant disease. Removal of the spleen is associated with numerous intraoperative and postoperative risks, including massive intraoperative hemorrhage, perioperative coagulation abnormalities, and post-splenectomy infection1. When caring for the patient with an enlarged spleen scheduled for splenectomy, the anesthetic plan must address both patient and procedure specific concerns. We present a medically challenging case of a 28 year old man with splenomegaly secondary to lymphoma, who underwent elective splenectomy, which was complicated by perioperative splenic rupture and hemorrhage. -

A Patient with Abdominal Pain, Vomiting and Splenomegaly
Clinicopathologic Conference A Patient with Abdominal Pain, Vomiting and Splenomegaly Eyal Reinstein MD PhD1, Rachel Pauzner MD2, Haim Mayan MD2 and Gina Schiby MD3 Departments of 1Medicine B, 2Medicine E and 3Pathology, Sheba Medical Center, Tel Hashomer, Israel IMAJ 2006;8:435-438 Case Presentation immunoglobulin G 7.2 U/ml (normal 0–15), anticardiolipin IgM R. Pauzner and H. Mayan >140 IU/ml (normal 0–15), circulating anticoagulant 1.94 (normal A 54 year old woman, married with four children, was admitted 0.9–1.3), circulating anticoagulantopartial thromboplastin time 2.81 in November 2004 because of splenomegaly and abdominal pain. (normal 0.9–1.55). Markers for malignancy and serology for hepao Her medical history included: hypertension, well controlled with titis C and B were negative. Abdominal CToangiography did not ramipril 2.5 mg/day, hypothyroidism treated with thyroxine, and demonstrate any arterial occlusions. Doppler ultrasound showed repair of an inguinal hernia 2 years earlier. In January 2003 she normal flow in the portal system and splenic vein. Repeated was admitted, for the first time, to a surgical ward because of gastroscopy was normal and gastric scan showed normal gastric abdominal pain from which she had been suffering for the previoo evacuation. Bone marrow biopsy was normal. The patient was ous 6 months. The pains occasionally appeared after a meal and discharged for further evaluation in the outpatient clinic. were located in the right lower quadrant and epigastric area. Endoscopic ultrasound demonstrated an enlarged lymph The evaluation revealed mild splenomegaly, gallbladder stones, node anterior to the pancreas and two hypoechogenic findings and a suspected intrauterine mass. -

No Stones, Some Groans, and Psychiatric Overtones with “Non-Specific” Splenomegaly
Open Access Case Report DOI: 10.7759/cureus.4638 No Stones, Some Groans, and Psychiatric Overtones with “Non-specific” Splenomegaly Jonathan C. Li 1 , Emma Lundsmith 2 1. Internal Medicine, Sidney Kimmel Medical College - Thomas Jefferson University, Philadelphia, USA 2. Internal Medicine, Thomas Jefferson University Hospital, Philadelphia, USA Corresponding author: Jonathan C. Li, [email protected] Abstract Hypercalcemia is a potentially life-threatening electrolyte imbalance that is commonly caused by hyperparathyroidism, supplement or medication use, and/or malignancy. Splenomegaly is commonly a non- specific finding, but in the setting of hypercalcemia, may provide diagnostic insight into the underlying pathology and warrant further evaluation. A 70-year-old man presented from his outpatient provider with serum calcium > 15 mg/dL with complaints of one-month fatigue, weakness, poor oral intake, 10 lbs. unintentional weight loss, and periodic confusion noted by his wife. He received an extensive inpatient workup which was non-diagnostic. Splenomegaly was observed on radiographic imaging and reported as “nonspecific”. Following discharge, denosumab was required to manage the hypercalcemia. Eventually, a diagnosis of primary splenic lymphoma was made months later. Laparoscopic splenectomy was planned but was advanced to an open laparotomy intraoperatively due to the rapid growth of the neoplasm. Early and close investigation of the spleen is warranted when splenomegaly presents in the setting of hypercalcemia and, as in this case, may prevent significant therapeutic burden. Categories: Endocrinology/Diabetes/Metabolism, Radiology, Oncology Keywords: splenic lymphoma, hypercalcemia of malignancy, hypercalcemia, splenomegaly, sonography Introduction Hypercalcemia is a potentially life-threatening electrolyte imbalance that is commonly caused by hyperparathyroidism, supplement or medication use, and/or malignancy [1-2]. -

Concurrent Ehrlichiosisand Babesiosis in A
Concurrent ehrlichiosis and babesiosis in a dog Alan R. Klag, Laurie E. Dunbar, Christine A. Girard A10-week-old intact male terrier-cross dog was pre- hemoglobinuria; and hyperbilirubinemia, bilirubinuria, sented to the Cote St. Luc Hospital for Animals on respectively) decreased our suspicion of its presence December 7, 1988 for routine examination. History in our case. The initial presence of regenerative revealed that the dog was a stray recently adopted in anemia, however, along with other clinical signs con- Greece. In accordance with Canadian regulations, the sistent with babesiosis, resulted in its inclusion as a dif- dog was examined and vaccinated by a veterinarian ferential diagnosis. A serum sample was sent to the in Greece prior to entering Canada one week before Laboratory of Veterinary Diagnostic Medicine of the presentation. Upon arrival in Canada, the owner had University of Illinois for determination ofE. canis and observed tapeworm segments in the stool but the B. canis antibody titers. Treatment with oral puppy was otherwise normal. oxytetracycline at 22 mg/kg (Apotetra, Apotex, On physical examination, the abnormal findings Toronto, Ontario) every eight hours was initiated. The were a poor hair coat, splenomegaly, pale mucous dog was also given oral metronidazole at 25 mg/kg membranes, a small pustule on the lateral maxillary (Apo-metronidazole, Apotex, Toronto, Ontario) every gingiva, and generalized gingivitis. The puppy was twelve hours for periodontal disease. bright, alert, and responsive. Initial diagnostic workup On day 2 of hospitalization, petechial hemorrhages included a complete blood count (CBC) (Table 1) and were observed on the gingiva and on the right pinna. -

Hypersplenism in Wilson's Disease
Gut: first published as 10.1136/gut.13.3.220 on 1 March 1972. Downloaded from Gut, 1972, 13, 220-224 Hypersplenism in Wilson's disease G. THOMAS STRICKLAND,' N-K. CHANG, AND WILLIAM M. BECKNER2 From the Departments of Clinical Investigation and Medical Physics, US Naval Medical Research Unit No. 2, Taipei, Taiwan, Republic of China SUMMARY Thirteen patients with Wilson's disease were compared with seven cirrhotic and 13 normal controls to define better the haematological abnormalities in this condition. Hypersplenism (anaemia, leukopenia, thrombocytopenia, and reduced red cell survival) commonly occurred in patients with both Wilson's disease and cirrhosis. These abnormalities correlated with splenic enlargement. Despite reduced haematocrits, red cell mass was greater in these two groups than in normal controls. Plasma volume and the body haematocrit/peripheral haematocrit ratios were also greater in patients with Wilson's disease and cirrhosis. Increased splenic sequestration of 51Cr-tagged red blood cells was not demonstrated in any subjects. The hypersplenism in patients with Wilson's disease is similar to that found in patients with cirrhosis from other causes. Splenomegaly and pancytopenia are common in On physical examination seven were noted to have Wilson's disease, a rare hereditary illness with an enlarged spleens; another had had a splenectomy for excessive burden of copper in the body. Patients with 'hypersplenism'. The data from the seven patients Wilson's disease have cirrhosis of the liver, a with clinically enlarged spleens and the remaining condition in which hypersplenism is frequent. six were analysed separately. The seven control http://gut.bmj.com/ Haemolytic anaemia has also been reported in subjects with cirrhosis had the diagnosis established Wilson's disease (Mclntyre, Clink, Levi, Cumings, by liver biopsy. -

Splenic Infarction: an Uncommon Presentation of Acute Infectious Mononucleosis
Splenic infarction: An uncommon presentation of acute infectious mononucleosis Madhulika Urella, MD1, Roma Srivastava, MD1, Waseem Ahmed, MD2, Yehuda Lebowicz, MD1 Author Affiliations: 1. Joan C. Edwards School of Medicine, Marshall University, Huntington, West Virginia 2. Marshall University, Huntington, West Virginia The authors have no financial disclosures to declare and no conflicts of interest to report. Corresponding Author: Madhulika Urella, MD Joan C. Edwards School of Medicine Marshall University Huntington, West Virginia Email: [email protected] Abstract Splenic infarction is a relatively uncommon diagnosis. It occurs when the splenic artery or one of its sub-branches is occluded with an infected or bland embolus or clot. Splenic infarction may be caused by atrial fibrillation, bacterial endocarditis, sickle cell disease, antiphospholipid syndrome, and trauma whereas an infectious etiology is uncommon. It is considered a rare presentation of acute infectious mononucleosis. Currently, its pathogenesis is still unclear. We describe a 24-year-old African American female who was admitted for evaluation of left-sided chest pain. Chest imaging, an abdominal ultrasound, and initial laboratory data were normal, followed by a negative hypercoagulability panel. Signs and symptoms of infectious etiology were absent, however, both IgM and IgG antibodies for Ebstein-Barr virus (EBV) viral capsid antigen were high. Contrast-enhanced abdominal computed tomography revealed splenomegaly and multiple infarcts in the spleen, which eventually led to the diagnosis of infectious mononucleosis-associated splenic infarction, resolving the diagnostic dilemma. Keywords Epstein-Barr virus, infectious mononucleosis, splenic infarction Introduction Splenic infarction is a rare presentation of acute infectious mononucleosis, occurring when the splenic artery or a sub-branch becomes occluded with an embolus or clot. -

Episode 77 –Fever in the Returning Traveler
Case 1 General approach to fever in the returning traveler A 60 year-old male, presents with a fever to your ED. He recently returned from India, where he spent 3 weeks visiting Episode 77 –Fever in the Returning relatives. He has no significant past medical history. Traveler Immunizations are up to date. He did id not receive any travel immunizations or malaria prophylaxis. The fever started 2 With Dr. Matthew Muller & Dr. Nazanin Meshkat days ago, and is associated with cough and chills. In the ED his vital signs are: Temp 38.4°C, BP 135/85, HR 120 bpm, RR Prepared by Dr. Keerat Grewal and Dr. Anton Helman, March 2016 22 and O2 saturation 94% on RA. Every year an increasing number of people travel abroad, and Key historical elements for fever in the returning travelers to tropical destinations are often immunologically traveler naïve to the regions they’re going to. It’s very common for travelers to get sick. In fact, about 2/3 of travelers get sick While it seems obvious here, one of the common errors that while they’re traveling or soon after their return, and emergency providers make in assessing fever is simply somewhere between 3 and 19% of travelers to developing forgetting to ask a travel history and thus missing the deadly countries will develop a fever. tropical disease diagnosis that has a vague presentation. Fever in the returning traveler is usually not caused by a Ask about travel in every patient who presents with fever dangerous tropical disease. These patients are much more The following areas are important to ask about in fever in the likely to have typical viral illnesses as a cause for their fever. -

A 7 Year Old Girl with Anemia and Massive Hepatosplenomegaly Mohammad Mizanur Rahman, Md
| Case Presentation | No. 01-2018 | A 7 year old girl with anemia and massive hepatosplenomegaly Mohammad Mizanur Rahman, Md. Mehedhi Hasan Shourov, Debashish Saha, Md. Abdul Ali Miah and S. M. Motahar Hossain Article Info Presentation of Case advised to get her admitted into the children ward for further management. In the child Departet of Heatology, Ared Dr. Md. Mehedhi Hasan Shourov: A 7 year old ward, patient and her parents were thoroughly Fores Istitute of Pathology, Dhaka Catoet, Dhaka, Bagladesh MMR, girl reported to the child outpatient department interviewed and the child was re-examined. MMHS; Departet of Bioheistry, of a military hospital in Chittagong (South-East The indoor physician ordered initial routine Dhaka Catoet, Dhaka, Bagladesh part of Bangladesh) Cantonment with the com- investigations such as complete blood count, DS; Departet of Mediie, Co- plaints of generalized weakness, loss of appe- peripheral blood film examination, malaria ied Military Hospital, Dhaka, Bagla- desh MAAM, SMMH tite, gradual distention of the abdomen and parasite, immuno-chromatographic test for weight loss. malaria, random blood sugar, liver function tests, urine routine and microscopic examina- The child was reasonably well and performing tion. After getting the results of all investi- For Correspondene: all her daily activities at her own 1 year before. Mohaad Mizaur Raha gations, child specialists sat together, reviewed She was also going to the school regularly and [email protected] her history, physical findings and the results of was worried when her parents noticed the all investigations so far received, discussed the Reeied: Otoer distension of her abdomen and reluctant to take case in details and decided to refer the patient Aepted: Jauary food adequately. -

Gastrointestinal Bleeding in Infants and Children
Gastrointestinal Bleeding in Infants and Children John T. Boyle Pediatrics in Review 2008;29;39 DOI: 10.1542/pir.29-2-39 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://pedsinreview.aappublications.org/content/29/2/39 Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly publication, it has been published continuously since 1979. Pediatrics in Review is owned, published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2008 by the American Academy of Pediatrics. All rights reserved. Print ISSN: 0191-9601. Downloaded from http://pedsinreview.aappublications.org/ at UNIV OF CHICAGO on May 9, 2013 Article gastroenterology Gastrointestinal Bleeding in Infants and Children John T. Boyle, MD* Objectives After completing this article, readers should be able to: 1. Develop a differential diagnosis based on the clinical presentation of gastrointestinal Author Disclosure (GI) blood loss. Dr Boyle did not 2. Discuss the age-related causes of upper and lower GI bleeding. disclose any financial 3. Delineate the sequence of evaluation and decision process in a child who has GI relationships relevant bleeding. to this article. 4. Describe new medical therapies and endoscopic maneuvers to control GI bleeding. Case Study A previously well 3-week-old female infant presented with a 2-day history of rectal bleeding. Her parents described three to five loose stools per day mixed with bright and dark red blood and mucus. Associated symptoms included episodic nonbilious, nonbloody emesis and an erythem- atous rash on her arms and legs.