Hepatosplenomegaly.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GASTROMEGALY and CHRONIC DUODENAL ILEUS in CHILDREN by REGINALD MILLER, M.D., F.R.C.P., Physician, Paddington Green Children's Hospital, with H
Arch Dis Child: first published as 10.1136/adc.5.26.83 on 1 April 1930. Downloaded from GASTROMEGALY AND CHRONIC DUODENAL ILEUS IN CHILDREN BY REGINALD MILLER, M.D., F.R.C.P., Physician, Paddington Green Children's Hospital, with H. COURTNEY GAGE, L.R.C.P., M.R.C.S., Radiologist, St. Mary's Hospital, London. This paper is concerned with a series of nine children who exhibited enlargement of the stomach with visible gastric peristalsis or other signs of obstruction high in the alimentary tract. The similarity between the cases is sufficient to suggest that they all belong to one group originating in some form of duodenal obstruction. Two of the nine cases were submitted to operation and were found to be examples of chronic duodenal ileus, and it is suggested that the others of the series owe their origin to the same cause. Gastromegaly is a convenient term for the enlarged and hypertrophied stomach which is the most striking clinical feature of such cases as these. http://adc.bmj.com/ Such a condition implies obstruction to the evacuation of the stomach and may be due to various causes; and as the site and nature of the obstruction, and even its very presence, may be difficult to determine, it is useful to have a group name which covers all such cases and emphasizes their one most obvious clinical abnormality. Were, for instance, the diagnosis of chronic duodenal ileus in the present cases disputed (and the subject is one of great difficulty), they would remain as a type of gastromegaly of obscure origin. -

An 8-Year-Old Boy with Fever, Splenomegaly, and Pancytopenia
An 8-Year-Old Boy With Fever, Splenomegaly, and Pancytopenia Rachel Offenbacher, MD,a,b Brad Rybinski, BS,b Tuhina Joseph, DO, MS,a,b Nora Rahmani, MD,a,b Thomas Boucher, BS,b Daniel A. Weiser, MDa,b An 8-year-old boy with no significant past medical history presented to his abstract pediatrician with 5 days of fever, diffuse abdominal pain, and pallor. The pediatrician referred the patient to the emergency department (ED), out of concern for possible malignancy. Initial vital signs indicated fever, tachypnea, and tachycardia. Physical examination was significant for marked abdominal distension, hepatosplenomegaly, and abdominal tenderness in the right upper and lower quadrants. Initial laboratory studies were notable for pancytopenia as well as an elevated erythrocyte sedimentation rate and C-reactive protein. aThe Children’s Hospital at Montefiore, Bronx, New York; and bAlbert Einstein College of Medicine, Bronx, New York Computed tomography (CT) of the abdomen and pelvis showed massive splenomegaly. The only significant history of travel was immigration from Dr Offenbacher led the writing of the manuscript, recruited various specialists for writing the Albania 10 months before admission. The patient was admitted to a tertiary manuscript, revised all versions of the manuscript, care children’s hospital and was evaluated by hematology–oncology, and was involved in the care of the patient; infectious disease, genetics, and rheumatology subspecialty teams. Our Mr Rybinski contributed to the writing of the multidisciplinary panel of experts will discuss the evaluation of pancytopenia manuscript and critically revised the manuscript; Dr Joseph contributed to the writing of the manuscript, with apparent multiorgan involvement and the diagnosis and appropriate cared for the patient, and was critically revised all management of a rare disease. -

Thme CANADIAN MEDICAL ASSOCIATION JOURNAL 137
Aug. 1930] THmE CANADIAN MEDICAL ASSOCIATION JOURNAL 137 DYSPEPSIA By ROBERT HUTCHISON, M.D., F.R.C.P., Phystcian to the London Hospital, London, Eng. TIHE first duty of anyone who undertakes to may lead to error, as to that form, not so write about dyspepsia is to define what he very uncommon, in which vomiting and even means by the term, for it is a word which is some pain occurs after every meal; such used very loosely, as we all know, both by doc- symptoms when they occur in a young un- tors and by patients, and is often enough made married woman may easily deceive. Or take to cover any form of abdominal discomfort again the vomiting of the gastric crises in which a patient may experience. But accuracy tabes. When these crises occur, as they some- :of diagnosis and efficient treatment demand a times do, early in the disease and before more precise use than this, and I propose in the the deep reflexes have disappeared, the fact of present paper to include under the term only their nervous origin is easily overlooked, and such abdominal discomfort as is felt during the every physician and surgeon of experience progress of digestion, and which is due to organic must have known cases in which even a gastro- disease of the stomach or to a primary disorder jejunostomy has been performed for gastric of its functions. For the purposes of this defini- crises under the belief that the patient was tion the duodenum may be regarded as part of s-uffering from organic disease of the stomach. -

Digestive Conditions, Miscellaneous Examination (Tuberculous
Digestive Conditions, Miscellaneous Examination (Tuberculous peritonitis, Inguinal hernia, Ventral hernia, Femoral hernia, Visceroptosis, and Benign and Malignant new growths) Comprehensive Worksheet Name: SSN: Date of Exam: C-number: Place of Exam: A. Review of Medical Records: B. Medical History (Subjective Complaints): 1. State date of onset, and describe circumstances and initial manifestations. 2. Course of condition since onset. 3. Current treatment, response to treatment, and any side effects of treatment. 4. History of related hospitalizations or surgery, dates and location, if known, reason or type of surgery. 5. If there was hernia surgery, report side, type of hernia, type of repair, and results, including current symptoms. 6. If there was injury or wound related to hernia, state date and type of injury or wound and relationship to hernia. 7. History of neoplasm: a. Date of diagnosis, exact diagnosis, location. b. Benign or malignant. c. Types of treatment and dates. d. Last date of treatment. e. State whether treatment has been completed. 8. For tuberculosis of the peritoneum, state date of diagnosis, type(s) and dates of treatment, date on which inactivity was established, and current symptoms. C. Physical Examination (Objective Findings): Address each of the following and fully describe current findings: 1. For hernia, state: a. type and location (including side) b. diameter in cm. c. whether remediable or operable d. whether a truss or belt is indicated, and whether it is well- supported by truss or belt e. whether it is readily reducible f. whether it has been previously repaired, and if so, whether it is well-healed and whether it is recurrent g. -

Department of Veterans Affairs § 4.114
Department of Veterans Affairs § 4.114 DISEASES OF THE HEART—Continued § 4.111 Postgastrectomy syndromes. Rat- There are various postgastrectomy ing symptoms which may occur following anastomotic operations of the stom- With the following in affected parts: Arthralgia or other pain, numbness, ach. When present, those occurring or cold sensitivity plus two or during or immediately after eating and more of the following: tissue loss, known as the ‘‘dumping syndrome’’ are nail abnormalities, color changes, characterized by gastrointestinal com- locally impaired sensation, hyperhidrosis, X-ray abnormali- plaints and generalized symptoms sim- ties (osteoporosis, subarticular ulating hypoglycemia; those occurring punched out lesions, or osteo- from 1 to 3 hours after eating usually arthritis) ....................................... 30 present definite manifestations of Arthralgia or other pain, numbness, or cold sensitivity plus tissue hypoglycemia. loss, nail abnormalities, color changes, locally impaired sensa- § 4.112 Weight loss. tion, hyperhidrosis, or X-ray ab- normalities (osteoporosis, sub- For purposes of evaluating conditions articular punched out lesions, or in § 4.114, the term ‘‘substantial weight osteoarthritis) ............................... 20 loss’’ means a loss of greater than 20 Arthralgia or other pain, numbness, percent of the individual’s baseline or cold sensitivity ......................... 10 weight, sustained for three months or NOTE (1): Separately evaluate amputations of fingers or toes, and complications such as squamous cell longer; and the term ‘‘minor weight carcinoma at the site of a cold injury scar or pe- loss’’ means a weight loss of 10 to 20 ripheral neuropathy, under other diagnostic codes. percent of the individual’s baseline Separately evaluate other disabilities that have been diagnosed as the residual effects of cold in- weight, sustained for three months or jury, such as Raynaud’s phenomenon, muscle at- longer. -

Case Report Gastric Volvulus Due to Splenomegaly - a Rare Entity
Case Report Gastric Volvulus Due to Splenomegaly - A rare Entity. Ashok Mhaske Department of Surgery,People’s College of Medical Sciences and Research Centre, Bhanpur, Bhopal. 462010 , (M.P.) Abstract: Gastric volvulus is a rare condition which typically presents with intermittent episodes of abdominal pain. The volvulus occurs around an axis made by two fixed points, organo-axial or mesentero-axial. Increased pressure within the hernial sac associated with gastric distension can lead to ischemia and perforation. Acute obstruction of a gastric volvulus is thus a surgical emergency.We present an unusual case of gastric volvulus secondary to tropical splenomegaly. Tropical splenomegaly precipitating gastric volvulus is not documented till date. Key Words: Gastric volvulus, Tropical splenomegaly. Introduction: to general practitioner but as symptoms persisted she Gastric volvulus is abnormal rotation of the was referred to our tertiary care centre for expert stomach of more than 180 degrees. It can cause closed opinion and management. loop obstrcution and at times can result in On examination, vital parameters and hydration was adequate with marked tenderness in incarceration and strangulation. Berti first described epigastric region with vague lump. Her routine gastric volvulus in 1866; to date, it remains a rare investigations were inconclusive but she did partially clinical entity. Berg performed the first successful responded to antispasmodic and antacid drugs. operation on a patient with gastric volvulus in 1896. Ultrasound of abdomen and Barium studies Borchardt (1904) described the classic triad of severe revealed gastric volvulus (Fig.1 & 2) with epigastric pain, retching without vomiting and splenomegaly for which she was taken up for inability to pass a nasogastric tube. -

Visceroptosis As a Cause of Stomach Trouble
VISCEROPTOSIS AS A CAUSE OF more physicians. In the writer's opinion, the "STOMACH TROUBLE." patient, and at times the family, may all be said to be in a state of neurasthenia. And small By William D. Reid, M.D., Boston. wonder, as they often have been given as many Visceroptosis has received a large share of opinions as they have consulted doctors,—some attention from orthopedists and internists dur- advising resort to surgery and others against. ing the past two decades, and medical literature This variation in the advice received generally is not lacking in excellent articles on the sub- has an upsetting effect. ject. Nevertheless, one continues to see cases At this point a few case reports will best serve not yet diagnosed, though they have passed to picture the type of patient to which the through the hands of one or more physicians. writer would draw attention. The type to which the writer refers is that in which the comes for relief of "stomach patient Case 1. Single woman. Seen June, 1915. not will trouble." It is held that this paper Aged 34 years. Canadian ; school teacher. Said present new facts, but it is hoped that it may to have gastric ulcer, but patient believes can- lay further emphasis on an important subject. cer to be the correct diagnosis. Family History The American Illustrated Dictionary defines —-Negative. Past History—Chicken-pox, scar- let fever and measles in childhood. "Sort of as "a or the falling down, visceroptosis prolapse, until 13 years old. Sore throat once a of " It is sometiues called Glenard 's puny" the viscera. -
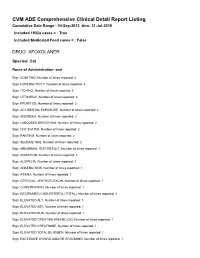
FDA CVM Comprehensive ADE Report Listing for Afoxolaner
CVM ADE Comprehensive Clinical Detail Report Listing Cumulative Date Range : 04-Sep-2013 -thru- 31-Jul-2018 Included 1932a cases = : True Included Medicated Feed cases = : False DRUG: AFOXOLANER Species: Cat Route of Administration: oral Sign: VOMITING, Number of times reported: 4 Sign: HYPERACTIVITY, Number of times reported: 3 Sign: ITCHING, Number of times reported: 3 Sign: LETHARGY, Number of times reported: 3 Sign: PRURITUS, Number of times reported: 3 Sign: ACCIDENTAL EXPOSURE, Number of times reported: 2 Sign: ANOREXIA, Number of times reported: 2 Sign: LABOURED BREATHING, Number of times reported: 2 Sign: NOT EATING, Number of times reported: 2 Sign: PANTING, Number of times reported: 2 Sign: SEIZURE NOS, Number of times reported: 2 Sign: ABNORMAL TEST RESULT, Number of times reported: 1 Sign: AGITATION, Number of times reported: 1 Sign: ALOPECIA, Number of times reported: 1 Sign: ANAEMIA NOS, Number of times reported: 1 Sign: ATAXIA, Number of times reported: 1 Sign: CERVICAL VENTROFLEXION, Number of times reported: 1 Sign: CONSTIPATION, Number of times reported: 1 Sign: DECREASED CHOLESTEROL (TOTAL), Number of times reported: 1 Sign: ELEVATED ALT, Number of times reported: 1 Sign: ELEVATED AST, Number of times reported: 1 Sign: ELEVATED BUN, Number of times reported: 1 Sign: ELEVATED CREATINE-KINASE (CK), Number of times reported: 1 Sign: ELEVATED CREATININE, Number of times reported: 1 Sign: ELEVATED TOTAL BILIRUBIN, Number of times reported: 1 Sign: EXCESSIVE LICKING AND/OR GROOMING, Number of times reported: 1 Sign: FEVER, -

General Anesthesia Complicated by Perioperative Iatrogenic Splenic Rupture
GENERAL ANESTHESIA COMPLICATED BY PERIOPERATIVE IATROGENIC SPLENIC RUPTURE JEREMY ASNIS* AND STEVEN M. NEUSTEIN** Abstract Patients with splenomegaly often present with diverse coexisting medical disease and thus offer a variety of anesthetic considerations. The challenges that come with splenectomy have also become increasingly common to the anesthesiologist, given the growing number of indications for surgical intervention including both benign and malignant disease. Removal of the spleen is associated with numerous intraoperative and postoperative risks, including massive intraoperative hemorrhage, perioperative coagulation abnormalities, and post-splenectomy infection1. When caring for the patient with an enlarged spleen scheduled for splenectomy, the anesthetic plan must address both patient and procedure specific concerns. We present a medically challenging case of a 28 year old man with splenomegaly secondary to lymphoma, who underwent elective splenectomy, which was complicated by perioperative splenic rupture and hemorrhage. Key words: splenomegaly, intraoperative rupture. Introduction Patients with splenomegaly often present with diverse coexisting medical disease and thus offer a variety of anesthetic considerations. The challenges that come with splenectomy have also become increasingly common to the anesthesiologist, given the growing number of indications for surgical intervention including both benign and malignant disease. Removal of the spleen is associated with numerous intraoperative and postoperative risks, including massive intraoperative hemorrhage, perioperative coagulation abnormalities, and post-splenectomy infection1. When caring for the patient with an enlarged spleen scheduled for splenectomy, the anesthetic plan must address both patient and procedure specific concerns. We present a medically challenging case of a 28 year old man with splenomegaly secondary to lymphoma, who underwent elective splenectomy, which was complicated by perioperative splenic rupture and hemorrhage. -

A Patient with Abdominal Pain, Vomiting and Splenomegaly
Clinicopathologic Conference A Patient with Abdominal Pain, Vomiting and Splenomegaly Eyal Reinstein MD PhD1, Rachel Pauzner MD2, Haim Mayan MD2 and Gina Schiby MD3 Departments of 1Medicine B, 2Medicine E and 3Pathology, Sheba Medical Center, Tel Hashomer, Israel IMAJ 2006;8:435-438 Case Presentation immunoglobulin G 7.2 U/ml (normal 0–15), anticardiolipin IgM R. Pauzner and H. Mayan >140 IU/ml (normal 0–15), circulating anticoagulant 1.94 (normal A 54 year old woman, married with four children, was admitted 0.9–1.3), circulating anticoagulantopartial thromboplastin time 2.81 in November 2004 because of splenomegaly and abdominal pain. (normal 0.9–1.55). Markers for malignancy and serology for hepao Her medical history included: hypertension, well controlled with titis C and B were negative. Abdominal CToangiography did not ramipril 2.5 mg/day, hypothyroidism treated with thyroxine, and demonstrate any arterial occlusions. Doppler ultrasound showed repair of an inguinal hernia 2 years earlier. In January 2003 she normal flow in the portal system and splenic vein. Repeated was admitted, for the first time, to a surgical ward because of gastroscopy was normal and gastric scan showed normal gastric abdominal pain from which she had been suffering for the previoo evacuation. Bone marrow biopsy was normal. The patient was ous 6 months. The pains occasionally appeared after a meal and discharged for further evaluation in the outpatient clinic. were located in the right lower quadrant and epigastric area. Endoscopic ultrasound demonstrated an enlarged lymph The evaluation revealed mild splenomegaly, gallbladder stones, node anterior to the pancreas and two hypoechogenic findings and a suspected intrauterine mass. -

No Stones, Some Groans, and Psychiatric Overtones with “Non-Specific” Splenomegaly
Open Access Case Report DOI: 10.7759/cureus.4638 No Stones, Some Groans, and Psychiatric Overtones with “Non-specific” Splenomegaly Jonathan C. Li 1 , Emma Lundsmith 2 1. Internal Medicine, Sidney Kimmel Medical College - Thomas Jefferson University, Philadelphia, USA 2. Internal Medicine, Thomas Jefferson University Hospital, Philadelphia, USA Corresponding author: Jonathan C. Li, [email protected] Abstract Hypercalcemia is a potentially life-threatening electrolyte imbalance that is commonly caused by hyperparathyroidism, supplement or medication use, and/or malignancy. Splenomegaly is commonly a non- specific finding, but in the setting of hypercalcemia, may provide diagnostic insight into the underlying pathology and warrant further evaluation. A 70-year-old man presented from his outpatient provider with serum calcium > 15 mg/dL with complaints of one-month fatigue, weakness, poor oral intake, 10 lbs. unintentional weight loss, and periodic confusion noted by his wife. He received an extensive inpatient workup which was non-diagnostic. Splenomegaly was observed on radiographic imaging and reported as “nonspecific”. Following discharge, denosumab was required to manage the hypercalcemia. Eventually, a diagnosis of primary splenic lymphoma was made months later. Laparoscopic splenectomy was planned but was advanced to an open laparotomy intraoperatively due to the rapid growth of the neoplasm. Early and close investigation of the spleen is warranted when splenomegaly presents in the setting of hypercalcemia and, as in this case, may prevent significant therapeutic burden. Categories: Endocrinology/Diabetes/Metabolism, Radiology, Oncology Keywords: splenic lymphoma, hypercalcemia of malignancy, hypercalcemia, splenomegaly, sonography Introduction Hypercalcemia is a potentially life-threatening electrolyte imbalance that is commonly caused by hyperparathyroidism, supplement or medication use, and/or malignancy [1-2]. -

Of Gastroptosis, Which, Though Only an Incidental Part Enteroptosis, Is
Dr. J. R. Pennington, Chicago : The general practitioner mobility of the stomach, which is affected by the posi¬ is entitled to the same information as the specialist; conse¬ tion of the individual, by the weight of the stomach quently, I intended that this paper should contain statistical contents and by the tension or relaxation of the abdom¬ information not obtained the and other readily by average inal muscles. We have endeavored to determine the physician. Dr. Hirschman is to be commended for his normal of the stomach in a of valuable suggestions, and were they put into practice "by position study 1,000 insurance companies and others they would do much for the cases, and have come to the conclusion that in the control of this dreaded disease. supine position the textbook teachings are correct ; but in the upright position there is a wide normal variation depending on the anatomic make-up of various types of individuals. there seems to be as much A CLINICAL AND ROENTGENOGRAPHIC Indeed, difference in the size, contour and position of the STUDY OF GASTROPTOSIS stomachs of men as there is of their mouths. come so as OBSERVATIONS IN ONE THOUSAND GASTRO- We have also to the conclusion that far is it matters INTESTINAL PATIENTS gastric digestion concerned, very little whether a stomach is in the high position or in the brim SEALE HARRIS, M.D. of the pelvis, so long as its muscular tonus is good and AND the intra-abdominal pressure is normal. We have J. P. CHAPMAN, M.D. repeatedly found patients whose stomachs in the BIRMINGHAM, ALA.