GP Fellowship Scheme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
BD22 Neath Port Talbot Unitary Development Plan
G White, Head of Planning, The Quays, Brunel Way, Baglan Energy Park, Neath, SA11 2GG. Foreword The Unitary Development Plan has been adopted following a lengthy and com- plex preparation. Its primary aims are delivering Sustainable Development and a better quality of life. Through its strategy and policies it will guide planning decisions across the County Borough area. Councillor David Lewis Cabinet Member with responsibility for the Unitary Development Plan. CONTENTS Page 1 PART 1 INTRODUCTION Introduction 1 Supporting Information 2 Supplementary Planning Guidance 2 Format of the Plan 3 The Community Plan and related Plans and Strategies 3 Description of the County Borough Area 5 Sustainability 6 The Regional and National Planning Context 8 2 THE VISION The Vision for Neath Port Talbot 11 The Vision for Individual Localities and Communities within 12 Neath Port Talbot Cwmgors 12 Ystalyfera 13 Pontardawe 13 Dulais Valley 14 Neath Valley 14 Neath 15 Upper Afan Valley 15 Lower Afan Valley 16 Port Talbot 16 3 THE STRATEGY Introduction 18 Settlement Strategy 18 Transport Strategy 19 Coastal Strategy 21 Rural Development Strategy 21 Welsh Language Strategy 21 Environment Strategy 21 4 OBJECTIVES The Objectives in terms of the individual Topic Chapters 23 Environment 23 Housing 24 Employment 25 Community and Social Impacts 26 Town Centres, Retail and Leisure 27 Transport 28 Recreation and Open Space 29 Infrastructure and Energy 29 Minerals 30 Waste 30 Resources 31 5 PART 1 POLICIES NUMBERS 1-29 32 6 SUSTAINABILITY APPRAISAL Sustainability -

Past Present Future Cwmafan
About the Bevan Foundation The Bevan Foundation is Wales’ most innovative and influential think tank. We develop lasting solutions to poverty and inequality. Our vision is for Wales to be a nation where everyone has a decent standard of living, a healthy and fulfilled life, and a voice in the decisions that affect them. As an independent, registered charity, the Bevan Foundation relies on the generosity of individuals and organisations for its work, as well as charitable trusts and foundations. You can find out more about how you can support us and get involved here: https://www.bevanfoundation.org/support-us/organisations/ Acknowledgements This paper is part of the Three Towns project which is looking at the pre-conditions for growing the foundational economy in Treharris in Merthyr Tydfil, Treherbert in Rhondda Cynon Taf and Cwmafan in Neath Port Talbot. It is funded by the Welsh Government’s Foundational Economy Challenge Fund. Copyright Bevan Foundation Cover image courtesy of David Slee, Cwmafan Author – Lloyd Jones Bevan Foundation 145a High Street Merthyr Tydfil, CF47 8DP February 2021 [email protected] www.bevanfoundation.org Registered charity no 1104191 Company registered in Wales no 4175018 Contents Contents .................................................................................................................................................. 1 Summary ................................................................................................................................................. 2 1. -

Neath Port Talbot County Borough Council Aspires to Deliver an Inclusive Education Service That Celebrates Diversity and Respects Everyone’S Right to Education
Appendix A Admission to Community Schools 2019/2020 1. Introduction The Council is the admission authority for all community maintained schools in the County Borough. As admission authority, the Council determines the criteria that will be applied when allocating places at community schools. This document sets out the admission arrangements that will apply during 2019/20 for: nursery classes based at community primary schools; community primary schools; community secondary schools; and the Welsh-medium sixth form at a community secondary school. For voluntary aided (i.e. Faith) schools, it is each school’s governing body that determines the admission arrangements, details of which can be obtained from the respective governing body. This policy document sets out the principles underpinning the admission arrangements for community schools together with the procedures and the timetables for admission during the 2019/20 school year (appendices 1, 2, 3 & 4). Further details to assist parents in applying for a school place choosing a school for their child will be set out in the ‘Information for Parents Handbook 2019/2020’ which will be available to parents in October 2018, prior to the application date. The handbook will contain important information about schools in the County Borough including their admission numbers, the catchment areas they serve together and their partner school arrangements. The handbook also contains the published admission arrangements for individual voluntary aided (i.e. Faith) schools. In this respect, the ‘Information for Parents Handbook 2019/2020 forms an integral part of the information available to parents on school admission. 2. Context Neath Port Talbot County Borough Council aspires to deliver an inclusive education service that celebrates diversity and respects everyone’s right to education. -
![LDP Policy H1 Housing Sites - Description of Site Constraints & Infrastructure Requirements [DRAFT STRUCTURE]](https://docslib.b-cdn.net/cover/6043/ldp-policy-h1-housing-sites-description-of-site-constraints-infrastructure-requirements-draft-structure-736043.webp)
LDP Policy H1 Housing Sites - Description of Site Constraints & Infrastructure Requirements [DRAFT STRUCTURE]
Contents 1 INTRODUCTION 1 2 POLICY H1 HOUSING SITES 3 3 2.1 Neath STRUCTURE] 2.1.1 H1/1 Gorffwysfa Care Home, Bryncoch 3 2.1.2 H1/2 Leiros Park Extension, Bryncoch 5 [DRAFT 2.1.3 H1/3 Groves Road (Phase 2), Cimla 7 2.1.4 H1/4 Ocean View, Jersey Marine 7 2.1.5 H1/5 Dwr Y Felin Lower School, Longford 7 2.1.6 H1/6 Hafod House Care Home, Neath 7 Requirements 2.1.7 H1/7 Neath Town Centre Redevelopment, Neath 7 2.1.8 H1/8 Crymlyn Grove (Phase 2), Skewen 7 2.1.9 H1/9 Crymlyn Grove (Phase 3), Skewen 7 Infrastructure 2.1.10 H1/10 Wern Goch, Skewen 7 & 2.1.11 H1/11 Neath Road / Fairyland Road, Tonna 7 2.1.12 H1/LB/1 Waunceirch, Bryncoch 7 2.1.13 H1/LB/2 Groves Road (Phase 1), Cimla 7 Constraints 2.1.14 H1/LB/3 Elba Crescent 7 Site 2.1.15 H1/LB/4 Area 1, Coed Darcy Urban Village, Llandarcy 7 of 2.1.16 H1/LB/5 Coed Darcy Urban Village, Llandarcy 7 2.1.17 H1/LB/6 Eaglesbush, Melincryddan 7 Description 2.1.18 H1/LB/7 Garthmor (Phase 2), Melincryddan 7 - 2.1.19 H1/LB/8 Briton Ferry Road, Neath 7 2.1.20 H1/LB/9 The Ropewalk, Neath 7 Sites 2.1.21 H1/LB/10 Barrons Court, Neath Abbey 7 2.1.22 H1/LB/11 Cardonnel Road, Skewen 7 Housing 2.1.23 H1/LB/12 Crymlyn Grove (Phase 1), Skewen 7 H1 2.2 Port Talbot 7 Policy 2.2.1 H1/12 Blaenbaglan School (land to the rear of), Baglan 8 LDP 2.2.2 H1/13 Hawthorn Close, Cwmafan 8 2.2.3 H1/14 Western Logs, Cwmafan 8 2.2.4 H1/15 Neath Port Talbot College (Margam Campus) 8 2.2.5 H1/16 Glanafan Comprehensive School, Port Talbot 8 2.2.6 H1/17 Harbourside, Port Talbot 8 2.2.7 H1/18 Afan Lido and land to the rear of Tywyn School, -
Description of the Parish
The Parish of Cwmafan St Michaels Church Annual Report & Accounts 2016 Description of the Parish St Michael’s Church is in the Parish of Cwmafan in the Rural Deanery of Margam and the Diocese of Llandaff in the Church in Wales. Worship has taken place on this site since the 12th century when records show a building dedicated to St Michael on the site in 1180. Priest in Charge: The Reverend Elaine Jenkyns, 66 Dinas Baglan Road, Port Talbot SA12 8AF Curate: The Reverend Stephen Jenkyns Independent Financial Mr Philip Hunkin, W B V Chartered Accountants Ltd (Watkins, Examiner: Bradfield, Vaughan), Woodfield House, Castle Walk, Neath, SA11 3LN Bankers: Lloyds TSB, Station Road, Port Talbot Architects: Caroe & Partners, Penniless Porch, Market Place, Wells, Somerset. BA5 2RB The Objectives and Constitution of the PCC The objective of the Parochial Church Council is to ensure that the life and work of the Church within the Parish helps to fulfil the mission of the Church in Wales both locally and more widely, whereby to advance the Christian religion throughout the world. The PCC is not a body corporate. Its composition, procedure and powers are regulated by the Constitution of the Church in Wales, as amended from time to time by its Governing Body. Elections are held at an Annual Easter Vestry Meeting, which last year took place on March 20th 2016 and this year will take place on April 9th 2017. All persons whose names are entered on the Electoral Roll are entitled to vote and to stand for election. Before assuming office, every member of the Council must sign a declaration that he/she will be bound by the Constitution. -

Player Registration Football Association of Wales
Player Registration TRANSFER Friday, 9 December, 2016 Football Association Of Wales Active Name ID DOB Player Status Transfer From To Date ABDILLAHI Omar 495049 12/10/1986 Non-Contract 02/12/2016 Pontypridd Town FC AFC Butetown AHMED Shaheen D 470620 05/09/1985 Non-Contract 03/12/2016 Llandudno Albion Penmaenmawr Phoenix FC ANDREWS Kelly L 617223 04/06/1984 Non-Contract 08/12/2016 Hafod Ladies FC Splott Albion Ladies AVO Adam L 483977 30/01/1986 Non-Contract 02/12/2016 Penllergaer Kilvey Fords F.C BABBS Graeme 539916 08/09/1987 Non-Contract 05/12/2016 Gorseinon Athletic Alltwen United FC BAILEY Ieuan 592978 24/08/2000 Non-Contract 02/12/2016 St Johns United FC Cwmbach Royal Stars FC (<18) BALL Nicholas J 495402 25/02/1973 Non-Contract 02/12/2016 Rassau AFC Ebbw Vale Town BARLEY Mathew O 549330 01/10/1993 Non-Contract 09/12/2016 Bethesda Athletic FC Llangoed and District BERRY Megan E 638029 09/08/1998 Non-Contract 03/12/2016 Goytre United Womens Caerphilly Castle Ladies & Girls FC BEYNON Ricky L 620509 24/10/1999 Non-Contract 08/12/2016 Afan Lido FC Trefelin BGC (<18) BISHOP Jay 707782 09/04/2007 Non-Contract 05/12/2016 Rafa Junior FC Fairwater Juniors (<18) BOULD Liam 581561 07/01/1998 Non-Contract 02/12/2016 Cwmffrwdoer Sports Blaenavon Blues AFC Club BRADLEY Keegan 665599 04/08/1997 Non-Contract 08/12/2016 Llanidloes Town FC Rhayader Town FC CAMPISI Joseph J 564862 03/11/1997 Non-Contract 02/12/2016 Pontardawe Town FC Rhos Rovers AFC CANIFF Ryan 473517 03/07/1987 Non-Contract 07/12/2016 Tredegar Town FC Ebbw Vale Town CHAMBERS Joshua -

Cabinet Director of Education, Leisure And
NEATH PORT TALBOT COUNTY BOROUGH COUNCIL CABINET 20th June 2018 DIRECTOR OF EDUCATION, LEISURE AND LIFELONG LEARNING ALED EVANS MATTER FOR DECISION WARDS AFFECTED: Cymmer, Glyncorrwg, Gwynfi, Margam, Taibach, Port Talbot, Bryn & Cwmafan, Pelenna STRATEGIC SCHOOL IMPROVEMENT PROGRAMME – FUTURE OF SECONDARY EDUCATION IN THE UPPER AFAN VALLEY Purpose of report 1. To obtain Cabinet approval to publish a proposal to make arrangements for pupils who would otherwise attend Cymer Afan Comprehensive school to receive their secondary education at a new build school in Margam, Ysgol Cwm Brombil, and to close Cymer Afan Comprehensive. 2. Publication of the proposal provides a 28th day period for the submission of objections. Following the period for submitting objections, Cabinet will need to meet to consider objections 1 received before taking a decision as to whether or not the proposal should be implemented. 3. This Cabinet report needs to be read in conjunction with the consultation report (appendix A), the consultation document (appendix B) and the Education, Skills and Culture Cabinet Board1 report of November 2017 (appendix C). Executive summary 4. The Council is responsible for promoting high educational standards and for delivering efficient primary and secondary education. This will involve reviewing the number and type of schools the Council has in its area and assessing whether or not best use is being made of resources and facilities in order to ensure future provision is sustainable. 5. Secondary education in the upper Afan Valley is provided at Cymer Afan Comprehensive school as part of a federation of five schools, four primary and one secondary. 6. -

Schedule of Buildings of Local Importance (Consultation Draft
Port Talbot Schedule Bryn & Cwmafan Ward: Settlement: Building Name: of Buildings Bryn & Cwmafan Oakwood Former St John’s Church of Ref: BCA001 Validation Stage I Stage II Grid Reference: E279441 Local N193985 Importance Address: Oakwood Avenue Site Location Plan (Consultation Draft - January 2019) 348 Port Talbot Description: Traditional early C20 church building set in original church yard forming a significant feature and open area in the centre of the village. The building has been rendered and refurbished and converted to 2019) residential use. Most windows replaced or partly replaced, but some original stone tracery retained together with stonework features and doorway surrounds. Small belfry on west end and substantial entrance porch. January - Draft (Consultation Importance Local of Buildings of Schedule Architectural Historic Historical / Group / Old or Rare Interest Interest Cultural settlement Local X X X Association character Buildings Value Justification for Consideration: An important and prominent building in the centre of the village that has been converted retaining some original character and form. Group value with village school buildings (BCA002) and listed Bethel Chapel. Notes: Notes: Coflein: Identified but no further information 349 Port Talbot Schedule Ward: Settlement: Building Name: Bryn & Cwmafan Oakwood Former Pontrhydyfen Primary School of Buildings Ref: BCA002 Validation Stage I Stage II Grid Reference: E277396 N194038 of Address: School Street Local Importance Site Location Plan (Consultation Draft - January -
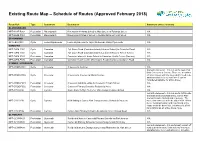
Existing Route Map – Schedule of Routes (Approved February 2018)
Existing Route Map – Schedule of Routes (Approved February 2018) Route Ref: Type Settlement Destination Statement (where relevant) BLAENGWRACH NPT-BLAE-P002 Pedestrian Blaengwrach Blaengwrach Infants School to High Street via Edwards Street N/A NPT-BLAE-P003 Pedestrian Blaengwrach Blaengwrach Primary School to Residential Area / High Street N/A BRYNAMMAN NPT-LBA-C001 Cycle Lower Brynamman Lower Brynamman to Twyn Via Amman Valley Cycle route N/A CWMAFAN NPT-CWM-C001 Cycle Cwmafan Ty'r-Owen Road (Cwmafan Infants & Junior School) to Cwmafan Road N/A NPT-CWM-C002 Cycle Cwmafan Ty'r-Owen Road (Cwmafan Infants & Junior School) to Tarren Terrace N/A NPT-CWM-P003 Pedestrian Cwmafan Cwmafan Infants & Junior School to Cwmafan Health Centre (Doctors) N/A NPT-CWM-P005 Pedestrian Cwmafan Cwmafan Health Centre (Doctors) to Residential Area via Salem Road N/A CYMMER / CROESERW NPT-CROE-C001 Cycle Croeserw Croeserw to Cymmer N/A Fail with statement – this is a useful route that links Croeserw to Caerau. There are a number NPT-CROE-C002 Cycle Croeserw Croeserw to Caerau via Menai Avenue of minor issues with the route which need to be addressed but in its current form it can be considered suitable for active travel. NPT-CROE-P001 Pedestrian Croeserw Croeserw Industrial estate to Croeserw Primary School N/A NPT-CROE-P002 Pedestrian Croeserw Croeserw Primary School to Residential Area N/A NPT-CYM-C002 Cycle Cymmer Route From Duffryn To Cymer Afan Comprehensive School N/A Fail with statement – this is a useful NCN route that acts as an important link to Cymer Afan Comprehensive School and Croeserw. -
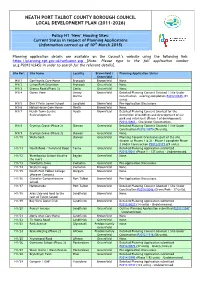
Policy H1 'New' Housing Sites: Current Status in Respect of Planning Applications
NEATH PORT TALBOT COUNTY BOROUGH COUNCIL LOCAL DEVELOPMENT PLAN (2011-2026) Policy H1 ‘New’ Housing Sites: Current Status in respect of Planning Applications (Information correct as of 10th March 2015) Planning application details are available on the Council’s website using the following link: https://planning.npt.gov.uk/welcome.asp [Note: Please type in the full application number (e.g.P2012/0345) in order to search for the relevant details]. Site Ref: Site Name Locality Brownfield / Planning Application Status Greenfield H1/1 Gorffwysfa Care Home Bryncoch Brownfield None. H1/2 Leiros Park Extension Bryncoch Greenfield None. H1/3 Groves Road (Phase 2) Cimla Greenfield None. H1/4 Ocean View Jersey Brownfield Detailed Planning Consent Granted / Site Under Marine Construction – nearing completion P2012/0345 (81 units). H1/5 Dwr Y Felin Lower School Longford Brownfield Pre-Application Discussions. H1/6 Hafod House Care Home Neath Brownfield None. H1/7 Neath Town Centre Neath Brownfield Detailed Planning Consent Granted for the Redevelopment demolition of buildings and development of car park and retail unit (Phase 1 of development) P2013/0863 – Site Under Construction. H1/8 Crymlyn Grove (Phase 2) Skewen Greenfield Detailed Planning Consent Granted / Site Under Construction P2012/0370 (76 units). H1/9 Crymlyn Grove (Phase 3) Skewen Greenfield None. H1/10 Wern Goch Skewen Greenfield Planning Consent Granted on part of the site (known as Phases 1 & 2) - Phase 1 complete Phase 2 Under Construction P2012/0171 (29 units). H1/11 Neath Road / Fairyland Road Tonna Greenfield Detailed Planning Application submitted P2015/0011 (Phase 1 – 137 units) - Undetermined. H1/12 Blaenbaglan School (land to Baglan Greenfield None. -
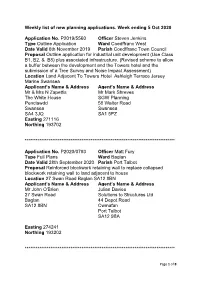
Week Ending 5Th October 2020
Weekly list of new planning applications. Week ending 5 Oct 2020 Application No. P2019/5560 Officer Steven Jenkins Type Outline Application Ward Coedffranc West Date Valid 6th November 2019 Parish Coedffranc Town Council Proposal Outline application for industrial unit development (Use Class B1, B2, & B8) plus associated infrastructure. (Revised scheme to allow a buffer between the development and the Towers hotel and the submission of a Tree Survey and Noise Impact Assessment) Location Land Adjacent To Towers Hotel Ashleigh Terrace Jersey Marine Swansea Applicant’s Name & Address Agent’s Name & Address Mr & Mrs N Zapettis Mr Mark Shreves The White House SGW Planning Penclawdd 58 Walter Road Swansea Swansea SA4 3JQ SA1 5PZ Easting 271116 Northing 193702 ********************************************************************************** Application No. P2020/0793 Officer Matt Fury Type Full Plans Ward Baglan Date Valid 28th September 2020 Parish Port Talbot Proposal Reinforced blockwork retaining wall to replace collapsed blockwork retaining wall to land adjacent to house Location 27 Swan Road Baglan SA12 8BN Applicant’s Name & Address Agent’s Name & Address Mr John O'Brien Julian Davies 27 Swan Road Solutions to Structures Ltd Baglan 44 Depot Road SA12 8BN Cwmafan Port Talbot SA12 9BA Easting 274241 Northing 193202 ********************************************************************************** Page 1 of 8 Application No. P2020/0820 Officer Andrea Davies Type Full Plans Ward Alltwen Date Valid 16th September 2020 Parish Cilybebyll Community Council Proposal Conversion of attic space to living accommodation, creation of balcony and insertion of bi fold doors to front elevation Location 4 Clos Gwenallt Alltwen Pontardawe SA8 3BD Applicant’s Name & Address Agent’s Name & Address Mr Alex Leigh Mr Thomas Connolly 4 Clos Gwenallt 21 Chalice Court Alltwen Port Talbot Pontardawe SA12 7DA SA8 3BD Easting 272631 Northing 203505 ********************************************************************************** Application No. -

UPPER OGMORE WIND FARM FIGURE 5.5 Landscape Character
Bridgend LCA Neat Port Talbot LCA 22 1: Llangynwyd Rolling Uplands and 1: Margam Marsh Forestry 3: Margam Country Park 2: Llynfi Valley Floor and Lower Slopes 4: Coedhirwaun 3: Llynfi & Garw Uplands and Forestry 21 4: Bettws Settled Farmland 5: Coedhirwaun Scarp and 19 open scarp tops 5: Garw Valley Floor and Lower Slopes 6: Mynydd Bromil, Mynydd 6: Mynydd Llangeinwyr Uplands Emroch & Mynydd Dinas UPPER OGMORE 7: Ogmore Valley Floor & Lower Slopes 7: Mynydd Margam WIND FARM 8: Goytre Valley 8: Ogmore Forest and Surrounding Uplands 9: Cefn Cethin 9: Hirwaun Common and Surrounding 10: Mynydd Bycham FIGURE 5.5 Ridges 11: Cwm Afan and Cwm Pelenna 24 10: Coity Rural Hinterland 12: Mynydd Penhydd Landscape 11: Merthyr Mawr Farmland, Warren 13: Foel Trawsnant Character and Coastline 12: Newton Down Limestone Plateau 14: Foel Fawr Areas (LCA) 15: Mynydd y Gelli 13: Porthcawl Coastline and Settled 18 Farmland 16: Briton Ferry Woods © CROWN COPYRIGHT, ALL RIGHTS RESERVED. 14: Kenfig Dunes and Coastline 17: Feol Fynyddau 2018 LICENCE NUMBER 0100031673. 15: Cefn Cribwr Ridge and Settled Site boundary Farmland 18: Mynydd Resolfen, Craig-y-Llyn Urban and Mynydd Ynyscorrwg 5km intervals from site boundary 20 11 19: Neath Valley 40 15km from site boundary 20: Gnoll Park 21: Hirfynydd 14 15 22: Banwen Pyrddin 24: Dulais Valley 17 13 16 40: Neath 12 49: Port Talbot, Sandfields, Baglan and Margam 51 9 50: Port Talbot Docks 10 3 and Margam works 51: Cwmafan 6 8 0 49 6 6 7 8 5 7 1 6 5km 2 4 50 5 3 1 4 9 Source: RES, LCAs based on online maps 10km LAYOUT DWG T-LAYOUT NO.