2005Msfreport-Ivorycoaststi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Côte D'ivoire
CÔTE D’IVOIRE COI Compilation August 2017 United Nations High Commissioner for Refugees Regional Representation for West Africa - RSD Unit UNHCR Côte d’Ivoire UNHCR Regional Representation for West Africa - RSD Unit UNHCR Côte d’Ivoire Côte d’Ivoire COI Compilation August 2017 This report collates country of origin information (COI) on Côte d’Ivoire up to 15 August 2017 on issues of relevance in refugee status determination for Ivorian nationals. The report is based on publicly available information, studies and commentaries. It is illustrative, but is neither exhaustive of information available in the public domain nor intended to be a general report on human-rights conditions. The report is not conclusive as to the merits of any individual refugee claim. All sources are cited and fully referenced. Users should refer to the full text of documents cited and assess the credibility, relevance and timeliness of source material with reference to the specific research concerns arising from individual applications. UNHCR Regional Representation for West Africa Immeuble FAALO Almadies, Route du King Fahd Palace Dakar, Senegal - BP 3125 Phone: +221 33 867 62 07 Kora.unhcr.org - www.unhcr.org Table of Contents List of Abbreviations .............................................................................................................. 4 1 General Information ....................................................................................................... 5 1.1 Historical background ............................................................................................ -

Militarized Youths in Western Côte D'ivoire
Militarized youths in Western Côte d’Ivoire - Local processes of mobilization, demobilization, and related humanitarian interventions (2002-2007) Magali Chelpi-den Hamer To cite this version: Magali Chelpi-den Hamer. Militarized youths in Western Côte d’Ivoire - Local processes of mobiliza- tion, demobilization, and related humanitarian interventions (2002-2007). African Studies Centre, 36, 2011, African Studies Collection. hal-01649241 HAL Id: hal-01649241 https://hal-amu.archives-ouvertes.fr/hal-01649241 Submitted on 27 Nov 2017 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. African Studies Centre African Studies Collection, Vol. 36 Militarized youths in Western Côte d’Ivoire Local processes of mobilization, demobilization, and related humanitarian interventions (2002-2007) Magali Chelpi-den Hamer Published by: African Studies Centre P.O. Box 9555 2300 RB Leiden The Netherlands [email protected] www.ascleiden.nl Cover design: Heike Slingerland Cover photo: ‘Market scene, Man’ (December 2007) Photographs: Magali Chelpi-den Hamer Printed by Ipskamp -

Côte D'ivoire Country Focus
European Asylum Support Office Côte d’Ivoire Country Focus Country of Origin Information Report June 2019 SUPPORT IS OUR MISSION European Asylum Support Office Côte d’Ivoire Country Focus Country of Origin Information Report June 2019 More information on the European Union is available on the Internet (http://europa.eu). ISBN: 978-92-9476-993-0 doi: 10.2847/055205 © European Asylum Support Office (EASO) 2019 Reproduction is authorised, provided the source is acknowledged, unless otherwise stated. For third-party materials reproduced in this publication, reference is made to the copyrights statements of the respective third parties. Cover photo: © Mariam Dembélé, Abidjan (December 2016) CÔTE D’IVOIRE: COUNTRY FOCUS - EASO COUNTRY OF ORIGIN INFORMATION REPORT — 3 Acknowledgements EASO acknowledges as the co-drafters of this report: Italy, Ministry of the Interior, National Commission for the Right of Asylum, International and EU Affairs, COI unit Switzerland, State Secretariat for Migration (SEM), Division Analysis The following departments reviewed this report, together with EASO: France, Office Français de Protection des Réfugiés et Apatrides (OFPRA), Division de l'Information, de la Documentation et des Recherches (DIDR) Norway, Landinfo The Netherlands, Immigration and Naturalisation Service, Office for Country of Origin Information and Language Analysis (OCILA) Dr Marie Miran-Guyon, Lecturer at the École des Hautes Études en Sciences Sociales (EHESS), researcher, and author of numerous publications on the country reviewed this report. It must be noted that the review carried out by the mentioned departments, experts or organisations contributes to the overall quality of the report, but does not necessarily imply their formal endorsement of the final report, which is the full responsibility of EASO. -
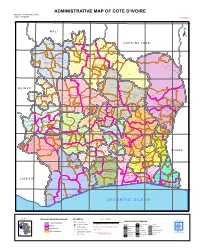
ADMINISTRATIVE MAP of COTE D'ivoire Map Nº: 01-000-June-2005 COTE D'ivoire 2Nd Edition
ADMINISTRATIVE MAP OF COTE D'IVOIRE Map Nº: 01-000-June-2005 COTE D'IVOIRE 2nd Edition 8°0'0"W 7°0'0"W 6°0'0"W 5°0'0"W 4°0'0"W 3°0'0"W 11°0'0"N 11°0'0"N M A L I Papara Débété ! !. Zanasso ! Diamankani ! TENGRELA [! ± San Koronani Kimbirila-Nord ! Toumoukoro Kanakono ! ! ! ! ! !. Ouelli Lomara Ouamélhoro Bolona ! ! Mahandiana-Sokourani Tienko ! ! B U R K I N A F A S O !. Kouban Bougou ! Blésségué ! Sokoro ! Niéllé Tahara Tiogo !. ! ! Katogo Mahalé ! ! ! Solognougo Ouara Diawala Tienny ! Tiorotiérié ! ! !. Kaouara Sananférédougou ! ! Sanhala Sandrégué Nambingué Goulia ! ! ! 10°0'0"N Tindara Minigan !. ! Kaloa !. ! M'Bengué N'dénou !. ! Ouangolodougou 10°0'0"N !. ! Tounvré Baya Fengolo ! ! Poungbé !. Kouto ! Samantiguila Kaniasso Monogo Nakélé ! ! Mamougoula ! !. !. ! Manadoun Kouroumba !.Gbon !.Kasséré Katiali ! ! ! !. Banankoro ! Landiougou Pitiengomon Doropo Dabadougou-Mafélé !. Kolia ! Tougbo Gogo ! Kimbirila Sud Nambonkaha ! ! ! ! Dembasso ! Tiasso DENGUELE REGION ! Samango ! SAVANES REGION ! ! Danoa Ngoloblasso Fononvogo ! Siansoba Taoura ! SODEFEL Varalé ! Nganon ! ! ! Madiani Niofouin Niofouin Gbéléban !. !. Village A Nyamoin !. Dabadougou Sinémentiali ! FERKESSEDOUGOU Téhini ! ! Koni ! Lafokpokaha !. Angai Tiémé ! ! [! Ouango-Fitini ! Lataha !. Village B ! !. Bodonon ! ! Seydougou ODIENNE BOUNDIALI Ponondougou Nangakaha ! ! Sokoro 1 Kokoun [! ! ! M'bengué-Bougou !. ! Séguétiélé ! Nangoukaha Balékaha /" Siempurgo ! ! Village C !. ! ! Koumbala Lingoho ! Bouko Koumbolokoro Nazinékaha Kounzié ! ! KORHOGO Nongotiénékaha Togoniéré ! Sirana -

Cote D'ivoire Summary Full Resettlement Plan (Frp)
AFRICAN DEVELOPMENT BANK GROUP PROJECT : GRID REINFORCEMENT AND RURAL ELECTRIFICATION PROJECT COUNTRY : COTE D’IVOIRE SUMMARY FULL RESETTLEMENT PLAN (FRP) Project Team : Mr. R. KITANDALA, Electrical Engineer, ONEC.1 Mr. P. DJAIGBE, Principal Energy Officer ONEC.1/SNFO Mr. M.L. KINANE, Principal Environmental Specialist ONEC.3 Mr. S. BAIOD, Consulting Environmentalist, ONEC.3 Project Team Sector Director: Mr. A.RUGUMBA, Director, ONEC Regional Director: Mr. A. BERNOUSSI, Acting Director, ORWA Division Manager: Mr. Z. AMADOU, Division Manager, ONEC.1, 1 GRID REIFORCEMENT AND RURAL ELECTRIFICATION PROJECT Summary FRP Project Name : GRID REIFORCEMENT AND RURAL ELECTRIFICATION PROJECT Country : COTE D’IVOIRE Project Number : P-CI-FA0-014 Department : ONEC Division: ONEC 1 INTRODUCTION This document presents the summary Full Resettlement Plan (FRP) of the Grid Reinforcement and Rural Electrification Project. It defines the principles and terms of establishment of indemnification and compensation measures for project affected persons and draws up an estimated budget for its implementation. This plan has identified 543 assets that will be affected by the project, while indicating their socio- economic status, the value of the assets impacted, the terms of compensation, and the institutional responsibilities, with an indicative timetable for its implementation. This entails: (i) compensating owners of land and developed structures, carrying out agricultural or commercial activities, as well as bearing trees and graves, in the road right-of-way for loss of income, at the monetary value replacement cost; and (ii) encouraging, through public consultation, their participation in the plan’s planning and implementation. 1. PROJECT DESCRIPTION AND IMPACT AREA 1.1. Project Description and Rationale The Grid Reinforcement and Rural Electrification Project seeks to strengthen power transmission infrastructure with a view to completing the primary network, ensuring its sustainability and, at the same time, upgrading its available power and maintaining its balance. -

République De Cote D'ivoire
R é p u b l i q u e d e C o t e d ' I v o i r e REPUBLIQUE DE COTE D'IVOIRE C a r t e A d m i n i s t r a t i v e Carte N° ADM0001 AFRIQUE OCHA-CI 8°0'0"W 7°0'0"W 6°0'0"W 5°0'0"W 4°0'0"W 3°0'0"W Débété Papara MALI (! Zanasso Diamankani TENGRELA ! BURKINA FASO San Toumoukoro Koronani Kanakono Ouelli (! Kimbirila-Nord Lomara Ouamélhoro Bolona Mahandiana-Sokourani Tienko (! Bougou Sokoro Blésségu é Niéllé (! Tiogo Tahara Katogo Solo gnougo Mahalé Diawala Ouara (! Tiorotiérié Kaouara Tienn y Sandrégué Sanan férédougou Sanhala Nambingué Goulia N ! Tindara N " ( Kalo a " 0 0 ' M'Bengué ' Minigan ! 0 ( 0 ° (! ° 0 N'd énou 0 1 Ouangolodougou 1 SAVANES (! Fengolo Tounvré Baya Kouto Poungb é (! Nakélé Gbon Kasséré SamantiguilaKaniasso Mo nogo (! (! Mamo ugoula (! (! Banankoro Katiali Doropo Manadoun Kouroumba (! Landiougou Kolia (! Pitiengomon Tougbo Gogo Nambonkaha Dabadougou-Mafélé Tiasso Kimbirila Sud Dembasso Ngoloblasso Nganon Danoa Samango Fononvogo Varalé DENGUELE Taoura SODEFEL Siansoba Niofouin Madiani (! Téhini Nyamoin (! (! Koni Sinémentiali FERKESSEDOUGOU Angai Gbéléban Dabadougou (! ! Lafokpokaha Ouango-Fitini (! Bodonon Lataha Nangakaha Tiémé Villag e BSokoro 1 (! BOUNDIALI Ponond ougou Siemp urgo Koumbala ! M'b engué-Bougou (! Seydougou ODIENNE Kokoun Séguétiélé Balékaha (! Villag e C ! Nangou kaha Togoniéré Bouko Kounzié Lingoho Koumbolokoro KORHOGO Nongotiénékaha Koulokaha Pign on ! Nazinékaha Sikolo Diogo Sirana Ouazomon Noguirdo uo Panzaran i Foro Dokaha Pouan Loyérikaha Karakoro Kagbolodougou Odia Dasso ungboho (! Séguélon Tioroniaradougou -

Crystal Reports
ELECTION DES DEPUTES A L'ASSEMBLEE NATIONALE SCRUTIN DU 06 MARS 2021 LISTE DEFINITIVE DES CANDIDATS PAR CIRCONSCRIPTION ELECTORALE Region : TONKPI Nombre de Sièges 190 - BIANKOUMA, BLAPLEU, KPATA ET SANTA, COMMUNES ET SOUS-PREFECTURES 1 Dossier N° Date de dépôt COULEURS U-00915 15/01/2021 INDEPENDANT VERT BLANC ADMINISTRATEUR TCHENICIEN T GONETY TIA PROSPER M S LOHI GBONGUE M HOSPITALIER SUPERIEUR Dossier N° Date de dépôt COULEURS U-00929 19/01/2021 INDEPENDANT OR INSPECTEUR DIOMANDE GONDOT GUY T MOUSSA DIOMANDE M S M ETUDIANT PEDAGOGIQUE XAVIER Dossier N° Date de dépôt COULEURS U-01333 21/01/2021 RASSEMBLEMENT DES HOUPHOUETISTES POUR LA DEMOCRATIE ET LA PAIX VERT ORANGE ENSEIGNANT ASSISTANT DU T MAMADOU DELY M S GUE BLEU CELESTIN M CHERCHEUR PERSONNEL Page 1 sur 21 T : TITULAIRE S : SUPPLEANT Dossier N° Date de dépôt COULEURS U-01566 22/01/2021 UDPCI/ARC-EN-CIEL BLEU-CIEL ASSISTANTE DE AGENT DE T GUEI SINGA MIREILLE CHANTAL F S SAHI BADIA JOSEPH M DIRECTION TRANSIT Dossier N° Date de dépôt COULEURS U-01576 22/01/2021 INDEPENDANT VERT BLANC T DELI LOUA M COMPTABLE S GOH OLIVIER M ETUDIANT Dossier N° Date de dépôt COULEURS U-01809 22/01/2021 ENSEMBLE POUR LA DEMOCRATIE ET LA SOUVERAINETE BLEU CHARRON CYAN BLANC INGENIEUR DES T LOUA ZOMI M S SOUMAHORO ROBERT M PROFFESSEUR TRAVAUX PUBLICS 190 - BIANKOUMA, BLAPLEU, KPATA ET SANTA, COMMUNES ET SOUS-PREFECTURES Page 2 sur 21 T : TITULAIRE S : SUPPLEANT Nombre de Sièges 191 - GBANGBEGOUINE, GBONNE ET GOUINE, COMMUNES ET SOUS-PREFECTURES 1 Dossier N° Date de dépôt COULEURS U-00916 15/01/2021 -

Projet : Projet De Renforcement Du Reseau De Transport Et D’Electrification Rurale
GROUPE DE LA BANQUE AFRICAINE DE DEVELOPPEMENT PROJET : PROJET DE RENFORCEMENT DU RESEAU DE TRANSPORT ET D’ELECTRIFICATION RURALE PAYS : COTE D’IVOIRE RESUME DE L’ETUDE D’IMPACT ENVIRONNEMENTAL ET SOCIAL (EIES) Equipe du projet Mr R. KITANDALA, Ingénieur électricien, ONEC.1 Mr P. DJAIGBE, chargé principal de l’énergie ONEC.1/SNFO Mr. M.L. KINANE, Environnementaliste principal ONEC.3 Mr. S. BAIOD, Environnementaliste Consultant, ONEC.3 Équipe Projet Directeur Sectoriel : Mr A.RUGUMBA, Directeur, ONEC Directeur Régional: Mr A. BERNOUSSI, Directeur, p.i, ORWA Chef de Division: Mr Z. AMADKOU, Chef de Division, ONEC.1, 1 RENFORCEMENT DU RESEAU DE TRANSPORT ET D’ELECTRIFICATION RURALE Résumé du PCR Titre du projet : PROJET DE RENFORCEMENT DU RESEAU DE TRANSPORT ET D’ELECTRIFICATION RURALE Pays : COTE D’IVOIRE Numéro de projet : P-CI-FA0-014 Département : ONEC Division: ONEC 1 INTRODUCTION Le résumé du plan complet de réinstallation (PCR) relatif au Projet Renforcement du Réseau de Transport et d’Electrification Rurale est présenté dans ce document. Il définit les principes et les modalités de mise en place des actions d’indemnisation et de compensation des personnes affectées par le projet et établit un budget estimatif pour sa mise en œuvre. Ce plan a identifié 1543 propriétés qui seront affectées par le projet, tout en indiquant leur statut socio-économique, la valeur des actifs impactés, les modalités d’indemnisation, les responsabilités institutionnelles assorti d’un chronogramme indicatif pour son exécution. Il est question : (i) de compenser les personnes propriétaires de terrains, et de structures bâties, exerçant des activités agricoles ou commerciales, ainsi que les arbres en production et les sépultures, dans l’emprise routière pour la perte de revenu, au coût de remplacement de la valeur vénale ; et (ii) d’encourager, par la consultation publique, leur participation à la planification et à la mise en œuvre du plan. -

Cote D'ivoire-Programme De Renforcement Des Ouvrages Du
REPUBLIQUE DE COTE D’IVOIRE UNION – DISCIPLINE – TRAVAIL -------------------------------- MINISTERE DU PETROLE, DE L’ENERGIE ET DES ENERGIES RENOUVELABLES --------------------------------- PLAN CADRE DE REINSTALLATION DU PROGRAMME DE RENFORCEMENT DES OUVRAGES DU SYSTEME ET D’ACCES A L ’ELECTRICITE (PROSER) DE 253 LOCALITES DANS LES REGIONS DU BAFING, DU BERE, DU WORODOUGOU, DU CAVALLY, DU GUEMON ET DU TONKPI RAPPORT FINAL Octobre 2019 CONSULTING SECURITE INDUSTRIELLE Angré 8ème Tranche, Immeuble ELVIRA Tél :22 52 56 38/ Cel :08 79 54 29 [email protected] Plan Cadre de Réinstallation du Programme de Renforcement des Ouvrages du Système et d’accès à l ’Electricité (PROSER) de 253 localités dans les Régions du Bafing, du Béré, du Worodougou, du Cavally, du Guémon et du Tonkpi TABLE DES MATIERES LISTE DES ACRONYMES VIII LISTE DES TABLEAUX X LISTE DES PHOTOS XI LISTE DES FIGURES XII DEFINITION DES TERMES UTILISES DANS CE RAPPORT XIII RESUME EXECUTIF XVII 1 INTRODUCTION 1 1.1 Programme de Renforcement des Ouvrages du Système et d’accès à l ’Electricité (PROSER) de 253 localités dans les Régions du Bafing, du Béré, du Worodougou, du Cavally, du Guémon et du Tonkpi 1 1.1.1 Situation de l’électrification rurale en Côte d’Ivoire 1 1.1.2 Justification du plan cadre de réinstallation 1 1.2 Objectifs du PCR 2 1.3 Approche méthodologique utilisée 3 1.3.1 Cadre d’élaboration du PCR 3 1.3.2 Revue documentaire 3 1.3.3 Visites de terrain et entretiens 3 1.4 Contenu et structuration du PCR 5 2 DESCRIPTION DU PROJET 7 2.1 Objectifs -

Rapport De La Cellule De Production
REPUBLIQUE DE CÔTE D’IVOIRE Union – Discipline – Travail -------------------------------------- MINISTERE DU PETROLE, DE L’ENERGIE ET DES ENERGIES RENOUVELABLES -------------------------------------- -------------------------------------- PROJET DE RENFORCEMENT DES OUVRAGES DU SYSTEME ELECTRIQUE ET D’ACCES A L’ELECTRICITE (PROSER) – PHASE 1 : ELECTRIFICATION RURALE DE 1 088 LOCALITES -------------------------------------- Lot 01 : Electrification Rurale de 253 localités dans les régions du Bafing, du Béré, du Worodougou, du Cavally, du Guémon et du Tonkpi -------------------------------------- PLAN CADRE DE REINSTALLATION (PCR) RAPPORT FINAL -- Octobre 2019 -- Plan Cadre de Réinstallation du Programme de Renforcement des Ouvrages du Système et d’accès à l ’Electricité (PROSER) de 253 localités dans les Régions du Bafing, du Béré, du Worodougou, du Cavally, du Guémon et du Tonkpi TABLE DES MATIERES LISTE DES SIGLES ET ACRONYMES VIII LISTE DES TABLEAUX X LISTE DES PHOTOS XI LISTE DES FIGURES XII DEFINITION DES TERMES UTILISES DANS CE RAPPORT XIII RESUME EXECUTIF XVII 1 INTRODUCTION 1 1.1 Programme de Renforcement des Ouvrages du Système Electrique et d’accès à l ’Electricité (PROSER) de 253 localités dans les Régions du Bafing, du Béré, du Worodougou, du Cavally, du Guémon et du Tonkpi 1 1.1.1 Situation de l’électrification rurale en Côte d’Ivoire 1 1.1.2 Justification du plan cadre de réinstallation 1 1.2 Objectifs du PCR 2 1.3 Approche méthodologique utilisée 3 1.3.1 Cadre d’élaboration du PCR 3 1.3.2 Revue documentaire 3 1.3.3 Visites -

Annuaire Statistique D'état Civil 2017 a Bénéficié De L’Appui Technique Et Financier De L’UNICEF
4 5 REPUBLIQUE DE CÔTE D’IVOIRE Union – Discipline – Travail ------------------ MINISTERE DE L'INTERIEUR ET DE LA SECURITE ---------------------------------- DIRECTION DES ETUDES, DE LA PROGRAMMATION ET DU SUIVI-EVALUATION ANNUAIRE STATISTIQUE D'ETAT CIVIL 2017 Les personnes ci-dessous nommées ont contribué à l’élaboration de cet annuaire : - Dr YAPI Amoncou Fidel MIS/DEPSE - GANNON née GNAHORE Ange-Lydie - KOYE Taneaucoa Modeste Eloge - YAO Kouakou Joseph MIS/DGAT - BINATE Mariame - GOGONE-BI Botty Maxime MIS/DGDDL - ADOU Danielle MIS/DAFM - ATSAIN Jean Jacques - ZEBA Rigobert MJDH/DECA - YAO Kouakou Charles-Elie MIS/CF - KOFFI Kouakou Roger - KOUAKOU Yao Alexis Thierry ONI - KOUDOUGNON Amone EPSE DJAGOURI DIIS - KONE Daouda SOUS-PREFECTURE DE KREGBE - TANO Hermann - BAKAYOKO Massoma INS - GNANZOU N'Guethas Sylvie Koutoua - TOURE Brahima - KOUAME Aya Charlotte EPSE KASSI ONP - IRIE BI Kouai Mathieu INTELLIGENCE MULTIMEDIA - YAO Gnekpie Florent - SIGUI Mokie Hyacinthe UNICEF 6 PREFACE Les efforts consentis par le Gouvernement pour hisser la Côte d’Ivoire au rang des pays émergents et consolider sa position dans la sous-région, ont notamment abouti à l’inscription de la réforme du système de l’état civil au nombre des actions prioritaires du Plan National de Développement (PND) 2016-2020. En effet, la problématique de l’enregistrement des faits d’état civil, constitue l’une des préoccupations majeures de l’Etat de Côte d’Ivoire pour la promotion des droits des individus, de la bonne gouvernance et de la planification du développement. Dans cette perspective, le Ministère de l’Intérieur et de la Sécurité (MIS), à travers la Direction des Etudes, de la Programmation et du Suivi-Evaluation (DEPSE), s’est engagé depuis 2012 à élaborer et éditer de façon régulière l’annuaire statistique des faits d’état civil. -

Ion Du Ministere D'etat, Ministere De L'interieur Et De La Securite
PPORT SUR LES ABUS DES DROITS DE L'HOMME COMMIS PAR DES DOZOS EN RÉPUBLIQUE DE CÔTE D'IVOIRE ION DU MINISTERE D'ETAT, MINISTERE DE L'INTERIEUR ET DE LA SECURITE Dans un rapport en date du mois de juin 2013, l'ONUCI et le bureau du Haut Commissariat aux Droits de l'Homme ont traité les abus des droits de l'homme commis par les Dozos en Côte d'Ivoire. Certaines recommandations formulées dans ce rapport font déjà l'objet de mesures en cours ou déjà exécuté au Ministère d'Etat, Ministère de l'Intérieur et de la Sécurité. 1. RAPPEL DES RECOMMANDATIONS DU RAPPORT Le rapport recommande aux autorités ivoiriennes: de déoloyer des forces de sécurité, de façon permanente et sur l'ensemble du territoire national afin de limiter le recours de la population aux Dozos et de renforcer la confiance entre ceux-ci et la population, notamment dans les localités où les forces de l'ordre sont inexistantes; de doter ces dernières de la formation et de moyens logistiques adéquats et les encourager à la discipline pour mener à bien leurs missions de défense et de protection des personnes et des biens; de mettre en œuvre toutes les mesures nécessaires afin que les Dozos cessent d'exercer des fonctions en matière de sécurité; d'inciter et d'accompagner les Dozos à mener un recensement général de leurs effectifs; de prendre toutes les mesures nécessaires pour s'assurer que les Dozos se conforment aux prescriptions du décret du 4 juillet 2012 portant réglementation des armes et des munitions en Côte d'Ivoire.