Iv. Isolation of Vibrio Cholerae from Fecal Specimens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Burkholderia Cenocepacia Integrates Cis-2-Dodecenoic Acid and Cyclic Dimeric Guanosine Monophosphate Signals to Control Virulence
Burkholderia cenocepacia integrates cis-2-dodecenoic acid and cyclic dimeric guanosine monophosphate signals to control virulence Chunxi Yanga,b,c,d,1, Chaoyu Cuia,b,c,1, Qiumian Yea,b, Jinhong Kane, Shuna Fua,b, Shihao Songa,b, Yutong Huanga,b, Fei Hec, Lian-Hui Zhanga,c, Yantao Jiaf, Yong-Gui Gaod, Caroline S. Harwoodb,g,2, and Yinyue Denga,b,c,2 aState Key Laboratory for Conservation and Utilization of Subtropical Agro-Bioresources, South China Agricultural University, Guangzhou 510642, China; bGuangdong Innovative Research Team of Sociomicrobiology, College of Agriculture, South China Agricultural University, Guangzhou 510642, China; cIntegrative Microbiology Research Centre, South China Agricultural University, Guangzhou 510642, China; dSchool of Biological Sciences, Nanyang Technological University, Singapore 637551; eCenter for Crop Germplasm Resources, Institute of Crop Sciences, Chinese Academy of Agricultural Sciences, Beijing 100081, China; fState Key Laboratory of Plant Genomics, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, China; and gDepartment of Microbiology, University of Washington, Seattle, WA 98195 Contributed by Caroline S. Harwood, October 30, 2017 (sent for review June 1, 2017; reviewed by Maxwell J. Dow and Tim Tolker-Nielsen) Quorum sensing (QS) signals are used by bacteria to regulate N-octanoyl homoserine lactone (C8-HSL). The two QS systems biological functions in response to cell population densities. Cyclic have both distinct and overlapping effects on gene expression diguanosine monophosphate (c-di-GMP) regulates cell functions in (16, 17). response to diverse environmental chemical and physical signals One of the ways in which QS systems can act is by controlling that bacteria perceive. In Burkholderia cenocepacia, the QS signal levels of intracellular cyclic diguanosine monophosphate (c-di-GMP) receptor RpfR degrades intracellular c-di-GMP when it senses the in bacteria (18–21). -

Cholera Transmission: the Host, Pathogen and Bacteriophage Dynamic
REVIEWS Cholera transmission: the host, pathogen and bacteriophage dynamic Eric J. Nelson*, Jason B. Harris‡§, J. Glenn Morris Jr||, Stephen B. Calderwood‡§ and Andrew Camilli* Abstract | Zimbabwe offers the most recent example of the tragedy that befalls a country and its people when cholera strikes. The 2008–2009 outbreak rapidly spread across every province and brought rates of mortality similar to those witnessed as a consequence of cholera infections a hundred years ago. In this Review we highlight the advances that will help to unravel how interactions between the host, the bacterial pathogen and the lytic bacteriophage might propel and quench cholera outbreaks in endemic settings and in emergent epidemic regions such as Zimbabwe. 15 O antigen Diarrhoeal diseases, including cholera, are the leading progenitor O1 El Tor strain . Although the O139 sero- The outermost, repeating cause of morbidity and the second most common cause group caused devastating outbreaks in the 1990s, the El oligosaccharide portion of LPS, of death among children under 5 years of age globally1,2. Tor strain remains the dominant strain globally11,16,17. which makes up the outer It is difficult to gauge the exact morbidity and mortality An extensive body of literature describes the patho- leaflet of the outer membrane of Gram-negative bacteria. of cholera because the surveillance systems in many physiology of cholera. In brief, pathogenic strains har- developing countries are rudimentary, and many coun- bour key virulence factors that include cholera toxin18 Cholera toxin tries are hesitant to report cholera cases to the WHO and toxin co-regulated pilus (TCP)19,20, a self-binding A protein toxin produced by because of the potential negative economic impact pilus that tethers bacterial cells together21, possibly V. -

Inverse Regulation of Vibrio Cholerae Biofilm Dispersal by Polyamine Signals Andrew a Bridges1,2, Bonnie L Bassler1,2*
RESEARCH ARTICLE Inverse regulation of Vibrio cholerae biofilm dispersal by polyamine signals Andrew A Bridges1,2, Bonnie L Bassler1,2* 1Department of Molecular Biology, Princeton University, Princeton, United States; 2The Howard Hughes Medical Institute, Chevy Chase, United States Abstract The global pathogen Vibrio cholerae undergoes cycles of biofilm formation and dispersal in the environment and the human host. Little is understood about biofilm dispersal. Here, we show that MbaA, a periplasmic polyamine sensor, and PotD1, a polyamine importer, regulate V. cholerae biofilm dispersal. Spermidine, a commonly produced polyamine, drives V. cholerae dispersal, whereas norspermidine, an uncommon polyamine produced by vibrios, inhibits dispersal. Spermidine and norspermidine differ by one methylene group. Both polyamines control dispersal via MbaA detection in the periplasm and subsequent signal relay. Our results suggest that dispersal fails in the absence of PotD1 because endogenously produced norspermidine is not reimported, periplasmic norspermidine accumulates, and it stimulates MbaA signaling. These results suggest that V. cholerae uses MbaA to monitor environmental polyamines, blends of which potentially provide information about numbers of ‘self’ and ‘other’. This information is used to dictate whether or not to disperse from biofilms. Introduction Bacteria frequently colonize environmental habitats and infection sites by forming surface-attached multicellular communities called biofilms. Participating in the biofilm lifestyle allows bacteria to col- lectively acquire nutrients and resist threats (Flemming et al., 2016). By contrast, the individual free- *For correspondence: swimming state allows bacteria to roam. The global pathogen Vibrio cholerae undergoes repeated [email protected] rounds of clonal biofilm formation and disassembly, and both biofilm formation and biofilm exit are central to disease transmission as V. -

Vibrio Cholerae O1, O139)
Cholera! (Toxigenic Vibrio cholerae O1, O139) Note: Only toxigenic strains of Vibrio cholerae serogroups O1 and O139 cause epidemics and are reportable as cholera. This guidance is intended for management of patients with toxigenic strains of V. cholerae serogroups O1 and O139 and early management (i.e., before laboratory confirmation is available) of patients with cholera-like illness returning from regions where cholera activity has been reported (e.g., travelers returning from Haiti or the Dominican Republic). For management of non-toxigenic strains of V. cholerae O1 and O139, toxigenic strains of other V. cholerae serogroups (e.g. O75 and O141), and other Vibrio species, refer to the guidance for vibriosis. PROTOCOL CHECKLIST Enter available information into Merlin within 24 hours of notification Review background on disease, case definition, laboratory testing (section 2, 3, and 4) Contact provider (section 5) Confirm diagnosis Obtain available demographic and clinical information Determine what information was provided to the patient Ensure collection and submission of appropriate specimens (section 4) Interview patient(s) (section 5) Review disease facts (section 2) Description of illness Modes of transmission Ask about exposure to relevant risk factors (section 5) Travel to an area affected by cholera Exposure to untreated water sources Exposure to raw shellfish or undercooked seafood Consumption of food imported from an area affected by cholera Pre-existing conditions Identify any similar cases of illness among contacts Determine -

The Columbian Exchange: a History of Disease, Food, and Ideas
Journal of Economic Perspectives—Volume 24, Number 2—Spring 2010—Pages 163–188 The Columbian Exchange: A History of Disease, Food, and Ideas Nathan Nunn and Nancy Qian hhee CColumbianolumbian ExchangeExchange refersrefers toto thethe exchangeexchange ofof diseases,diseases, ideas,ideas, foodfood ccrops,rops, aandnd populationspopulations betweenbetween thethe NewNew WorldWorld andand thethe OldOld WWorldorld T ffollowingollowing thethe voyagevoyage ttoo tthehe AAmericasmericas bbyy ChristoChristo ppherher CColumbusolumbus inin 1492.1492. TThehe OldOld WWorld—byorld—by wwhichhich wwee mmeanean nnotot jjustust EEurope,urope, bbutut tthehe eentirentire EEasternastern HHemisphere—gainedemisphere—gained fromfrom tthehe CColumbianolumbian EExchangexchange iinn a nnumberumber ooff wways.ays. DDiscov-iscov- eeriesries ooff nnewew ssuppliesupplies ofof metalsmetals areare perhapsperhaps thethe bestbest kknown.nown. BButut thethe OldOld WWorldorld aalsolso ggainedained newnew staplestaple ccrops,rops, ssuchuch asas potatoes,potatoes, sweetsweet potatoes,potatoes, maize,maize, andand cassava.cassava. LessLess ccalorie-intensivealorie-intensive ffoods,oods, suchsuch asas tomatoes,tomatoes, chilichili peppers,peppers, cacao,cacao, peanuts,peanuts, andand pineap-pineap- pplesles wwereere aalsolso iintroduced,ntroduced, andand areare nownow culinaryculinary centerpiecescenterpieces inin manymany OldOld WorldWorld ccountries,ountries, namelynamely IItaly,taly, GGreece,reece, andand otherother MediterraneanMediterranean countriescountries (tomatoes),(tomatoes), -

Enteric Infections Due to Campylobacter, Yersinia, Salmonella, and Shigella*
Bulletin of the World Health Organization, 58 (4): 519-537 (1980) Enteric infections due to Campylobacter, Yersinia, Salmonella, and Shigella* WHO SCIENTIFIC WORKING GROUP1 This report reviews the available information on the clinical features, pathogenesis, bacteriology, and epidemiology ofCampylobacter jejuni and Yersinia enterocolitica, both of which have recently been recognized as important causes of enteric infection. In the fields of salmonellosis and shigellosis, important new epidemiological and relatedfindings that have implications for the control of these infections are described. Priority research activities in each ofthese areas are outlined. Of the organisms discussed in this article, Campylobacter jejuni and Yersinia entero- colitica have only recently been recognized as important causes of enteric infection, and accordingly the available knowledge on these pathogens is reviewed in full. In the better- known fields of salmonellosis (including typhoid fever) and shigellosis, the review is limited to new and important information that has implications for their control.! REVIEW OF RECENT KNOWLEDGE Campylobacterjejuni In the last few years, C.jejuni (previously called 'related vibrios') has emerged as an important cause of acute diarrhoeal disease. Although this organism was suspected of being a cause ofacute enteritis in man as early as 1954, it was not until 1972, in Belgium, that it was first shown to be a relatively common cause of diarrhoea. Since then, workers in Australia, Canada, Netherlands, Sweden, United Kingdom, and the United States of America have reported its isolation from 5-14% of diarrhoea cases and less than 1 % of asymptomatic persons. Most of the information given below is based on conclusions drawn from these studies in developed countries. -

Bacterial Foodborne and Diarrheal Disease National Case Surveillance
Bacterial Foodborne and Diarrheal Disease National Case Surveillance Annual Report, 2003 Enteric Diseases Epidemiology Branch Division of Foodborne, Bacterial and Mycotic Diseases National Center for Zoonotic, Vectorborne and Enteric Diseases Centers for Disease Control and Prevention The Bacterial Foodborne and Diarrheal Disease National Case Surveillance is published by the Enteric Diseases Epidemiology Branch, Division of Foodborne, Bacterial and Mycotic Diseases, National Center for Zoonotic, Vectorborne and Enteric Diseases, Centers for Disease Control and Prevention, Atlanta, GA 30333 SUGGESTED CITATION Centers for Disease Control and Prevention. Bacterial Foodborne and Diarrheal Disease National Case Surveillance. Annual Report, 2003. Atlanta Centers for Disease Control and Prevention; 2005: pg. Nos - 2 - Contents Executive Summary……………………………………………………………………………… - 4- Expanded Surveillance Summaries of Selected Pathogens and Diseases, 2003………………… -10- Botulism…………………………………………………………………………………. -10- Non-O157 Shiga toxin-producing Escherichia coli………………………………………-18- Salmonella………………………………………………………………………………...-22- Shigella……………………………………………………………………………………-28- Vibrio……………………………………………………………………………………...-33- Surveillance Data Sources and Background……………………………………………………... -40- National Notifiable Diseases Surveillance System and the National Electronic Telecommunications System for Surveillance…………………………………………… -40- Public Health Laboratory Information System…………………………………………... -41- Limitations common to NETSS and PHLIS…………………………………………….. -

Gonorrhea Also Called the "Clap" Or "Drip," Gonorrhea Is a Contagious Disease Transmitted Most Often Through Sexual Contact with an Infected Person
Gonorrhea Also called the "clap" or "drip," gonorrhea is a contagious disease transmitted most often through sexual contact with an infected person. Gonorrhea may also be spread by contact with infected bodily fluids, so that a mother could pass on the infection to her newborn during childbirth. Both men and women can get gonorrhea. The infection is easily spread and occurs most often in people who have many sex partners. What Causes Gonorrhea? Gonorrhea is caused by Neisseria gonorrhoeae, a bacterium that can grow and multiply easily in mucus membranes of the body. Gonorrhea bacteria can grow in the warm, moist areas of the reproductive tract, including the cervix (opening to the womb), uterus (womb), and fallopian tubes (egg canals) in women, and in the urethra (the tube that carries urine from the bladder to outside the body) in women and men. The bacteria can also grow in the mouth, throat, and anus. Gonorrhea symptoms in women ● Greenish yellow or whitish discharge from the vagina ● Lower abdominal or pelvic pain ● Burning when urinating ● Conjunctivitis (red, itchy eyes) ● Bleeding between periods ● Spotting after intercourse ● Swelling of the vulva (vulvitis) Gonorrhea symptoms in men ● Greenish yellow or whitish discharge from the penis ● Burning when urinating ● Burning in the throat (due to oral sex) ● Painful or swollen testicles ● Swollen glands in the throat (due to oral sex) In men, symptoms usually appear two to 14 days after infection. How Is Gonorrhea Treated? To cure a gonorrhea infection, your doctor will give you either an oral or injectable antibiotic. Your partner should also be treated at the same time to prevent reinfection and further spread of the disease. -

Influence of Environmental Conditions on Fatty Acid-Induced Changes in Vibrio Cholerae Persistence and Pathogenicity
University of Tennessee at Chattanooga UTC Scholar Student Research, Creative Works, and Honors Theses Publications 5-2019 Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity Abigail Doyle University of Tennessee at Chattanooga, [email protected] Follow this and additional works at: https://scholar.utc.edu/honors-theses Part of the Environmental Sciences Commons Recommended Citation Doyle, Abigail, "Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity" (2019). Honors Theses. This Theses is brought to you for free and open access by the Student Research, Creative Works, and Publications at UTC Scholar. It has been accepted for inclusion in Honors Theses by an authorized administrator of UTC Scholar. For more information, please contact [email protected]. Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity Abigail Lea Doyle Departmental Honors Thesis The University of Tennessee at Chattanooga Department of Civil and Chemical Engineering Examination Date: 08 April 2019 Bradley J. Harris, Ph.D. David Giles, Ph.D. Assistant Professor of Civil and Chemical Assistant Professor of Biology, Geology and Engineering Environmental Science Thesis Director Department Examiner ABSTRACT Vibrio cholerae, a Gram-negative bacterium, is responsible for the acute intestinal infection known as cholera. This illness is due in part to V. cholerae’s ability to sense and adapt to changing environments as it is ingested into the human body from brackish environments. It was shown in recent studies that this bacteria has the ability to uptake exogenous fatty acids, resulting in changes to V. -

Vibrio: Myths Vs. Facts “Flesh-Eating Bacteria” Is a Phrase Often At- Weakened Immune Systems Are at Higher Risk Inside This Issue
Public Health Information for Community Partners 5150 NW Milner Dr. prime Port St. Lucie, FL 34983 EPIsodes 15 August 2015 Phone (772) 462‐ 3800 www.stluciecountyhealth.com/ Vibrio: Myths vs. Facts “Flesh-eating bacteria” is a phrase often at- weakened immune systems are at higher risk Inside this issue... tached to infections associated with the group for these type of infections as well. Called a of bacteria called Vibrios. This phrase is also “necrotizing skin infection,” this is a rare, very Vibrio: Myths vs. often followed by the warning that these bacte- severe infection that can destroy muscles, skin Facts 1 ria have been found in local waters and that and surrounding tissues. SLC Reportable someone died after getting infected. Many different bacteria can cause necrotizing Diseases While “flesh eating bacteria” is a media fa- fasciitis. Streptococcus (group A Strep) is the Incidence Report 2 vorite, it is misleading, inaccurate and creates most common cause. Others include: Staph anxiety for many people. The presence of Vib- aureus (found on most people’s skin), E. coli, rios in nature does not mean that anyone who and Clostridium, to name a few. goes swimming or fishing risks a skin dissolv- “NO VIBRIO” TIPS ing bacterial infection. Continue to enjoy your water and beach activi- Fact is, Vibrios are a group of free-living bac- ties using the following prevention measures: teria found in coastal waters worldwide that Additional Vibrio Vulnificus If you have a weakened immune system, liv- reproduce rapidly in warmer, brackish or low information can be found at: er disease or other chronic condition, avoid http://www.floridahealth.gov/ salt waters. -
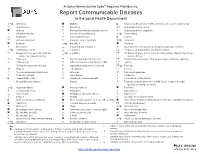
Report Communicable Diseases to the Local Health Department
Arizona Administrative Code Requires Providers to: Report Communicable Diseases to the Local Health Department *O Amebiasis Glanders O Respiratory disease in a health care institution or correctional facility Anaplasmosis Gonorrhea * Rubella (German measles) Anthrax Haemophilus influenzae, invasive disease Rubella syndrome, congenital Arboviral infection Hansen’s disease (Leprosy) *O Salmonellosis Babesiosis Hantavirus infection O Scabies Basidiobolomycosis Hemolytic uremic syndrome *O Shigellosis Botulism *O Hepatitis A Smallpox Brucellosis Hepatitis B and Hepatitis D Spotted fever rickettsiosis (e.g., Rocky Mountain spotted fever) *O Campylobacteriosis Hepatitis C Streptococcal group A infection, invasive disease Chagas infection and related disease *O Hepatitis E Streptococcal group B infection in an infant younger than 90 days of age, (American trypanosomiasis) invasive disease Chancroid HIV infection and related disease Streptococcus pneumoniae infection (pneumococcal invasive disease) Chikungunya Influenza-associated mortality in a child 1 Syphilis Chlamydia trachomatis infection Legionellosis (Legionnaires’ disease) *O Taeniasis * Cholera Leptospirosis Tetanus Coccidioidomycosis (Valley Fever) Listeriosis Toxic shock syndrome Colorado tick fever Lyme disease Trichinosis O Conjunctivitis, acute Lymphocytic choriomeningitis Tuberculosis, active disease Creutzfeldt-Jakob disease Malaria Tuberculosis latent infection in a child 5 years of age or younger (positive screening test result) *O Cryptosporidiosis -

Vibrio Inhibens Sp. Nov., a Novel Bacterium with Inhibitory Activity Against Vibrio Species
The Journal of Antibiotics (2012) 65, 301–305 & 2012 Japan Antibiotics Research Association All rights reserved 0021-8820/12 www.nature.com/ja ORIGINAL ARTICLE Vibrio inhibens sp. nov., a novel bacterium with inhibitory activity against Vibrio species Jose´ Luis Balca´zar1,2, Miquel Planas1 and Jose´ Pintado1 Strain BFLP-10T, isolated from faeces of wild long-snouted seahorses (Hippocampus guttulatus), is a Gram-negative, motile and facultatively anaerobic rod. This bacterium produces inhibitory activity against Vibrio species. Phylogenetic analysis based on 16S rRNA gene sequences showed that strain BFLP-10T was a member of the genus Vibrio and was most closely related to Vibrio owensii (99%), Vibrio communis (98.9%), Vibrio sagamiensis (98.9%) and Vibrio rotiferianus (98.4%). However, multilocus sequence analysis using gyrB, pyrH, recA and topA genes revealed low levels of sequence similarity (o91.2%) with these closely related species. In addition, strain BFLP-10T could be readily differentiated from other closely related species by several phenotypic properties and fatty acid profiles. The G þ C content of the DNA was 45.6 mol%. On the basis of phenotypic, chemotaxonomic and phylogenetic data, strain BFLP-10T represents a novel species within the genus Vibrio, for which the name Vibrio inhibens sp. nov. is proposed. The type strain is BFLP-10T (¼ CECT 7692T ¼ DSM 23440T). The Journal of Antibiotics (2012) 65, 301–305; doi:10.1038/ja.2012.22; published online 4 April 2012 Keywords: polyphasic taxonomic analysis; seahorses; Vibrio inhibens INTRODUCTION Physiological and biochemical characterization The family Vibrionaceae currently comprises six validly published Gram reaction was determined using the non-staining (KOH) method.13 Cell genera: Vibrio,1 Photobacterium,2 Salinivibrio,3 Enterovibrio,4 Grimontia5 morphology and motility were studied using phase-contrast microscopy and 14 and Aliivibrio.6 Vibrio species are common inhabitants of aquatic electron microscopy as previously described by Herrera et al.