Campylobacter Jejuni Survival Strategies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pdf/47/12/943/1655814/0362-028X-47 12 943.Pdf by Guest on 25 September 2021 Washington, D.C
943 Journal of Food Protection, Vol. 47, No. 12, Pages 943-949 (December 1984) Copyright®, International Association of Milk, Food, and Environmental Sanitarians Campylobacter jejuni and Campylobacter coli Production of a Cytotonic Toxin Immunologically Similar to Cholera Toxin BARBARA A. McCARDELL1*, JOSEPH M. MADDEN1 and EILEEN C. LEE2'3 Division of Microbiology, Food and Drug Administration, Washington, D.C. 20204, and Department of Biology, The Catholic University of America,Downloaded from http://meridian.allenpress.com/jfp/article-pdf/47/12/943/1655814/0362-028x-47_12_943.pdf by guest on 25 September 2021 Washington, D.C. 20064 (Received for publication September 6, 1983) ABSTRACT monella typhimurium is related to CT (31), although its role in pathogenesis has not been determined. Production An enzyme-linked immunosorbent assay (ELISA) based on by some strains of Aeromonas species of a toxin which binding to cholera toxin (CT) antibody was used to screen cell- free supernatant fluids from 11 strains of Campylobacter jejuni can be partially neutralized by CT antiserum in rat loops and one strain of Campylobacter coli. Positive results for seven suggests some relationship to CT (21). of the eight clinical isolates as well as for one animal and one Although Campylobacter jejuni and Campylobacter food isolate suggested that these strains produced an extracellu coli have long been known as animal pathogens, only in lar factor immunologically similar to CT. An affinity column recent years have their importance and prevalence in (packed with Sepharose 4B conjugated to purified anti-CT IgG human disease been recognized (13,22). With the advent via cyanogen bromide) was used to separate the extracellular of improved methods (77), C. -

Cholera Transmission: the Host, Pathogen and Bacteriophage Dynamic
REVIEWS Cholera transmission: the host, pathogen and bacteriophage dynamic Eric J. Nelson*, Jason B. Harris‡§, J. Glenn Morris Jr||, Stephen B. Calderwood‡§ and Andrew Camilli* Abstract | Zimbabwe offers the most recent example of the tragedy that befalls a country and its people when cholera strikes. The 2008–2009 outbreak rapidly spread across every province and brought rates of mortality similar to those witnessed as a consequence of cholera infections a hundred years ago. In this Review we highlight the advances that will help to unravel how interactions between the host, the bacterial pathogen and the lytic bacteriophage might propel and quench cholera outbreaks in endemic settings and in emergent epidemic regions such as Zimbabwe. 15 O antigen Diarrhoeal diseases, including cholera, are the leading progenitor O1 El Tor strain . Although the O139 sero- The outermost, repeating cause of morbidity and the second most common cause group caused devastating outbreaks in the 1990s, the El oligosaccharide portion of LPS, of death among children under 5 years of age globally1,2. Tor strain remains the dominant strain globally11,16,17. which makes up the outer It is difficult to gauge the exact morbidity and mortality An extensive body of literature describes the patho- leaflet of the outer membrane of Gram-negative bacteria. of cholera because the surveillance systems in many physiology of cholera. In brief, pathogenic strains har- developing countries are rudimentary, and many coun- bour key virulence factors that include cholera toxin18 Cholera toxin tries are hesitant to report cholera cases to the WHO and toxin co-regulated pilus (TCP)19,20, a self-binding A protein toxin produced by because of the potential negative economic impact pilus that tethers bacterial cells together21, possibly V. -

Vibrio Cholerae O1, O139)
Cholera! (Toxigenic Vibrio cholerae O1, O139) Note: Only toxigenic strains of Vibrio cholerae serogroups O1 and O139 cause epidemics and are reportable as cholera. This guidance is intended for management of patients with toxigenic strains of V. cholerae serogroups O1 and O139 and early management (i.e., before laboratory confirmation is available) of patients with cholera-like illness returning from regions where cholera activity has been reported (e.g., travelers returning from Haiti or the Dominican Republic). For management of non-toxigenic strains of V. cholerae O1 and O139, toxigenic strains of other V. cholerae serogroups (e.g. O75 and O141), and other Vibrio species, refer to the guidance for vibriosis. PROTOCOL CHECKLIST Enter available information into Merlin within 24 hours of notification Review background on disease, case definition, laboratory testing (section 2, 3, and 4) Contact provider (section 5) Confirm diagnosis Obtain available demographic and clinical information Determine what information was provided to the patient Ensure collection and submission of appropriate specimens (section 4) Interview patient(s) (section 5) Review disease facts (section 2) Description of illness Modes of transmission Ask about exposure to relevant risk factors (section 5) Travel to an area affected by cholera Exposure to untreated water sources Exposure to raw shellfish or undercooked seafood Consumption of food imported from an area affected by cholera Pre-existing conditions Identify any similar cases of illness among contacts Determine -

Comparative Analysis of Four Campylobacterales
REVIEWS COMPARATIVE ANALYSIS OF FOUR CAMPYLOBACTERALES Mark Eppinger*§,Claudia Baar*§,Guenter Raddatz*, Daniel H. Huson‡ and Stephan C. Schuster* Abstract | Comparative genome analysis can be used to identify species-specific genes and gene clusters, and analysis of these genes can give an insight into the mechanisms involved in a specific bacteria–host interaction. Comparative analysis can also provide important information on the genome dynamics and degree of recombination in a particular species. This article describes the comparative genomic analysis of representatives of four different Campylobacterales species — two pathogens of humans, Helicobacter pylori and Campylobacter jejuni, as well as Helicobacter hepaticus, which is associated with liver cancer in rodents and the non-pathogenic commensal species, Wolinella succinogenes. ε CHEMOLITHOTROPHIC The -subdivision of the Proteobacteria is a large group infection can lead to gastric cancer in humans 9–11 An organism that is capable of of CHEMOLITHOTROPHIC and CHEMOORGANOTROPHIC microor- and liver cancer in rodents, respectively .The using CO, CO2 or carbonates as ganisms with diverse metabolic capabilities that colo- Campylobacter representative C. jejuni is one of the the sole source of carbon for cell nize a broad spectrum of ecological habitats. main causes of bacterial food-borne illness world- biosynthesis, and that derives Representatives of the ε-subgroup can be found in wide, causing acute gastroenteritis, and is also energy from the oxidation of reduced inorganic or organic extreme marine and terrestrial environments ranging the most common microbial antecedent of compounds. from oceanic hydrothermal vents to sulphidic cave Guillain–Barré syndrome12–15.Besides their patho- springs. Although some members are free-living, others genic potential in humans, C. -

The Columbian Exchange: a History of Disease, Food, and Ideas
Journal of Economic Perspectives—Volume 24, Number 2—Spring 2010—Pages 163–188 The Columbian Exchange: A History of Disease, Food, and Ideas Nathan Nunn and Nancy Qian hhee CColumbianolumbian ExchangeExchange refersrefers toto thethe exchangeexchange ofof diseases,diseases, ideas,ideas, foodfood ccrops,rops, aandnd populationspopulations betweenbetween thethe NewNew WorldWorld andand thethe OldOld WWorldorld T ffollowingollowing thethe voyagevoyage ttoo tthehe AAmericasmericas bbyy ChristoChristo ppherher CColumbusolumbus inin 1492.1492. TThehe OldOld WWorld—byorld—by wwhichhich wwee mmeanean nnotot jjustust EEurope,urope, bbutut tthehe eentirentire EEasternastern HHemisphere—gainedemisphere—gained fromfrom tthehe CColumbianolumbian EExchangexchange iinn a nnumberumber ooff wways.ays. DDiscov-iscov- eeriesries ooff nnewew ssuppliesupplies ofof metalsmetals areare perhapsperhaps thethe bestbest kknown.nown. BButut thethe OldOld WWorldorld aalsolso ggainedained newnew staplestaple ccrops,rops, ssuchuch asas potatoes,potatoes, sweetsweet potatoes,potatoes, maize,maize, andand cassava.cassava. LessLess ccalorie-intensivealorie-intensive ffoods,oods, suchsuch asas tomatoes,tomatoes, chilichili peppers,peppers, cacao,cacao, peanuts,peanuts, andand pineap-pineap- pplesles wwereere aalsolso iintroduced,ntroduced, andand areare nownow culinaryculinary centerpiecescenterpieces inin manymany OldOld WorldWorld ccountries,ountries, namelynamely IItaly,taly, GGreece,reece, andand otherother MediterraneanMediterranean countriescountries (tomatoes),(tomatoes), -

Enteric Infections Due to Campylobacter, Yersinia, Salmonella, and Shigella*
Bulletin of the World Health Organization, 58 (4): 519-537 (1980) Enteric infections due to Campylobacter, Yersinia, Salmonella, and Shigella* WHO SCIENTIFIC WORKING GROUP1 This report reviews the available information on the clinical features, pathogenesis, bacteriology, and epidemiology ofCampylobacter jejuni and Yersinia enterocolitica, both of which have recently been recognized as important causes of enteric infection. In the fields of salmonellosis and shigellosis, important new epidemiological and relatedfindings that have implications for the control of these infections are described. Priority research activities in each ofthese areas are outlined. Of the organisms discussed in this article, Campylobacter jejuni and Yersinia entero- colitica have only recently been recognized as important causes of enteric infection, and accordingly the available knowledge on these pathogens is reviewed in full. In the better- known fields of salmonellosis (including typhoid fever) and shigellosis, the review is limited to new and important information that has implications for their control.! REVIEW OF RECENT KNOWLEDGE Campylobacterjejuni In the last few years, C.jejuni (previously called 'related vibrios') has emerged as an important cause of acute diarrhoeal disease. Although this organism was suspected of being a cause ofacute enteritis in man as early as 1954, it was not until 1972, in Belgium, that it was first shown to be a relatively common cause of diarrhoea. Since then, workers in Australia, Canada, Netherlands, Sweden, United Kingdom, and the United States of America have reported its isolation from 5-14% of diarrhoea cases and less than 1 % of asymptomatic persons. Most of the information given below is based on conclusions drawn from these studies in developed countries. -

Survival of Escherichia Coli O157:H7 and Campylobacter Jejuni in Bottled Purified Drinking Water Under Different Storage Conditions
0 Journal of Food Protection, Vol. 000, No. 000, 0000, Pages 000–000 doi:10.4315/0362-028X.JFP-10-368 Copyright G, International Association for Food Protection Survival of Escherichia coli O157:H7 and Campylobacter jejuni in Bottled Purified Drinking Water under Different Storage Conditions HAMZAH M. AL-QADIRI,1* XIAONAN LU,2 NIVIN I. AL-ALAMI,3 AND BARBARA A. RASCO2 1Department of Nutrition and Food Technology, Faculty of Agriculture, The University of Jordan, Amman 11942, Jordan; 2School of Food Science, Box 646376, Washington State University, Pullman, Washington 99164-6376, USA; and 3Water and Environment Research and Study Center, The University of Jordan, Amman 11942, Jordan MS 10-368: Received 1 September 2010/Accepted 15 October 2010 ABSTRACT ;< Survival of Escherichia coli O157:H7 and Campylobacter jejuni that were separately inoculated into bottled purified drinking water was investigated during storage at 22, 4, and 218uC for 5, 7, and 2 days, respectively. Two inoculation levels were used, 1 and 10 CFU/ml (102 and 103 CFU/100 ml). In samples inoculated with 102 CFU/100 ml, C. jejuni was not detectable (.2-log reduction) after storage under the conditions specified above. E. coli O157:H7 was detected on nonselective and selective media at log reductions of 1.08 to 1.25 after storage at 22uC, 1.19 to 1.56 after storage at 4uC, and 1.54 to 1.98 after storage at 218uC. When the higher inoculation level of 103 CFU/100 ml was used, C. jejuni was able to survive at 22 and 4uC, with 2.25- and 2.17-log reductions observed on nonselective media, respectively. -

The Global View of Campylobacteriosis
FOOD SAFETY THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS REPORT OF AN EXPERT CONSULTATION UTRECHT, NETHERLANDS, 9-11 JULY 2012 THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS IN COLLABORATION WITH Food and Agriculture of the United Nations THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS REPORT OF EXPERT CONSULTATION UTRECHT, NETHERLANDS, 9-11 JULY 2012 IN COLLABORATION WITH Food and Agriculture of the United Nations The global view of campylobacteriosis: report of an expert consultation, Utrecht, Netherlands, 9-11 July 2012. 1. Campylobacter. 2. Campylobacter infections – epidemiology. 3. Campylobacter infections – prevention and control. 4. Cost of illness I.World Health Organization. II.Food and Agriculture Organization of the United Nations. III.World Organisation for Animal Health. ISBN 978 92 4 156460 1 _____________________________________________________ (NLM classification: WF 220) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index. html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Bacterial Foodborne and Diarrheal Disease National Case Surveillance
Bacterial Foodborne and Diarrheal Disease National Case Surveillance Annual Report, 2003 Enteric Diseases Epidemiology Branch Division of Foodborne, Bacterial and Mycotic Diseases National Center for Zoonotic, Vectorborne and Enteric Diseases Centers for Disease Control and Prevention The Bacterial Foodborne and Diarrheal Disease National Case Surveillance is published by the Enteric Diseases Epidemiology Branch, Division of Foodborne, Bacterial and Mycotic Diseases, National Center for Zoonotic, Vectorborne and Enteric Diseases, Centers for Disease Control and Prevention, Atlanta, GA 30333 SUGGESTED CITATION Centers for Disease Control and Prevention. Bacterial Foodborne and Diarrheal Disease National Case Surveillance. Annual Report, 2003. Atlanta Centers for Disease Control and Prevention; 2005: pg. Nos - 2 - Contents Executive Summary……………………………………………………………………………… - 4- Expanded Surveillance Summaries of Selected Pathogens and Diseases, 2003………………… -10- Botulism…………………………………………………………………………………. -10- Non-O157 Shiga toxin-producing Escherichia coli………………………………………-18- Salmonella………………………………………………………………………………...-22- Shigella……………………………………………………………………………………-28- Vibrio……………………………………………………………………………………...-33- Surveillance Data Sources and Background……………………………………………………... -40- National Notifiable Diseases Surveillance System and the National Electronic Telecommunications System for Surveillance…………………………………………… -40- Public Health Laboratory Information System…………………………………………... -41- Limitations common to NETSS and PHLIS…………………………………………….. -

Gonorrhea Also Called the "Clap" Or "Drip," Gonorrhea Is a Contagious Disease Transmitted Most Often Through Sexual Contact with an Infected Person
Gonorrhea Also called the "clap" or "drip," gonorrhea is a contagious disease transmitted most often through sexual contact with an infected person. Gonorrhea may also be spread by contact with infected bodily fluids, so that a mother could pass on the infection to her newborn during childbirth. Both men and women can get gonorrhea. The infection is easily spread and occurs most often in people who have many sex partners. What Causes Gonorrhea? Gonorrhea is caused by Neisseria gonorrhoeae, a bacterium that can grow and multiply easily in mucus membranes of the body. Gonorrhea bacteria can grow in the warm, moist areas of the reproductive tract, including the cervix (opening to the womb), uterus (womb), and fallopian tubes (egg canals) in women, and in the urethra (the tube that carries urine from the bladder to outside the body) in women and men. The bacteria can also grow in the mouth, throat, and anus. Gonorrhea symptoms in women ● Greenish yellow or whitish discharge from the vagina ● Lower abdominal or pelvic pain ● Burning when urinating ● Conjunctivitis (red, itchy eyes) ● Bleeding between periods ● Spotting after intercourse ● Swelling of the vulva (vulvitis) Gonorrhea symptoms in men ● Greenish yellow or whitish discharge from the penis ● Burning when urinating ● Burning in the throat (due to oral sex) ● Painful or swollen testicles ● Swollen glands in the throat (due to oral sex) In men, symptoms usually appear two to 14 days after infection. How Is Gonorrhea Treated? To cure a gonorrhea infection, your doctor will give you either an oral or injectable antibiotic. Your partner should also be treated at the same time to prevent reinfection and further spread of the disease. -

Influence of Environmental Conditions on Fatty Acid-Induced Changes in Vibrio Cholerae Persistence and Pathogenicity
University of Tennessee at Chattanooga UTC Scholar Student Research, Creative Works, and Honors Theses Publications 5-2019 Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity Abigail Doyle University of Tennessee at Chattanooga, [email protected] Follow this and additional works at: https://scholar.utc.edu/honors-theses Part of the Environmental Sciences Commons Recommended Citation Doyle, Abigail, "Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity" (2019). Honors Theses. This Theses is brought to you for free and open access by the Student Research, Creative Works, and Publications at UTC Scholar. It has been accepted for inclusion in Honors Theses by an authorized administrator of UTC Scholar. For more information, please contact [email protected]. Influence of environmental conditions on fatty acid-induced changes in Vibrio cholerae persistence and pathogenicity Abigail Lea Doyle Departmental Honors Thesis The University of Tennessee at Chattanooga Department of Civil and Chemical Engineering Examination Date: 08 April 2019 Bradley J. Harris, Ph.D. David Giles, Ph.D. Assistant Professor of Civil and Chemical Assistant Professor of Biology, Geology and Engineering Environmental Science Thesis Director Department Examiner ABSTRACT Vibrio cholerae, a Gram-negative bacterium, is responsible for the acute intestinal infection known as cholera. This illness is due in part to V. cholerae’s ability to sense and adapt to changing environments as it is ingested into the human body from brackish environments. It was shown in recent studies that this bacteria has the ability to uptake exogenous fatty acids, resulting in changes to V. -
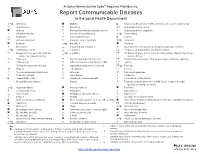
Report Communicable Diseases to the Local Health Department
Arizona Administrative Code Requires Providers to: Report Communicable Diseases to the Local Health Department *O Amebiasis Glanders O Respiratory disease in a health care institution or correctional facility Anaplasmosis Gonorrhea * Rubella (German measles) Anthrax Haemophilus influenzae, invasive disease Rubella syndrome, congenital Arboviral infection Hansen’s disease (Leprosy) *O Salmonellosis Babesiosis Hantavirus infection O Scabies Basidiobolomycosis Hemolytic uremic syndrome *O Shigellosis Botulism *O Hepatitis A Smallpox Brucellosis Hepatitis B and Hepatitis D Spotted fever rickettsiosis (e.g., Rocky Mountain spotted fever) *O Campylobacteriosis Hepatitis C Streptococcal group A infection, invasive disease Chagas infection and related disease *O Hepatitis E Streptococcal group B infection in an infant younger than 90 days of age, (American trypanosomiasis) invasive disease Chancroid HIV infection and related disease Streptococcus pneumoniae infection (pneumococcal invasive disease) Chikungunya Influenza-associated mortality in a child 1 Syphilis Chlamydia trachomatis infection Legionellosis (Legionnaires’ disease) *O Taeniasis * Cholera Leptospirosis Tetanus Coccidioidomycosis (Valley Fever) Listeriosis Toxic shock syndrome Colorado tick fever Lyme disease Trichinosis O Conjunctivitis, acute Lymphocytic choriomeningitis Tuberculosis, active disease Creutzfeldt-Jakob disease Malaria Tuberculosis latent infection in a child 5 years of age or younger (positive screening test result) *O Cryptosporidiosis