Ciliary Muscle Thickness Changes Are Associated with Age THESIS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Distribution of Immune Cells in the Uveal Tract of the Normal Eye
THE DISTRIBUTION OF IMMUNE CELLS IN THE UVEAL TRACT OF THE NORMAL EYE PAUL G. McMENAMIN Perth, Western Australia SUMMARY function of these cells in the normal iris, ciliary body Inflammatory and immune-mediated diseases of the and choroid. The role of such cell types in ocular eye are not purely the consequence of infiltrating inflammation, which will be discussed by other inflammatory cells but may be initiated or propagated authors in this issue, is not the major focus of this by immune cells which are resident or trafficking review; however, a few issues will be briefly through the normal eye. The uveal tract in particular considered where appropriate. is the major site of many such cells, including resident tissue macro phages, dendritic cells and mast cells. This MACRO PHAGES review considers the distribution and location of these and other cells in the iris, ciliary body and choroid in Mononuclear phagocytes arise from bone marrow the normal eye. The uveal tract contains rich networks precursors and after a brief journey in the blood as of both resident macrophages and MHe class 11+ monocytes immigrate into tissues to become macro dendritic cells. The latter appear strategically located to phages. In their mature form they are widely act as sentinels for capturing and sampling blood-borne distributed throughout the body. Macrophages are and intraocular antigens. Large numbers of mast cells professional phagocytes and play a pivotal role as are present in the choroid of most species but are effector cells in cell-mediated immunity and inflam virtually absent from the anterior uvea in many mation.1 In addition, due to their active secretion of a laboratory animals; however, the human iris does range of important biologically active molecules such contain mast cells. -

Ciliary Zonule Sclera (Suspensory Choroid Ligament)
ACTIVITIES Complete Diagrams PNS 18 and 19 Complete PNS 23 Worksheet 3 #1 only Complete PNS 24 Practice Quiz THE SPECIAL SENSES Introduction Vision RECEPTORS Structures designed to respond to stimuli Variable complexity GENERAL PROPERTIES OF RECEPTORS Transducers Receptor potential Generator potential GENERAL PROPERTIES OF RECEPTORS Stimulus causing receptor potentials Generator potential in afferent neuron Nerve impulse SENSATION AND PERCEPTION Stimulatory input Conscious level = perception Awareness = sensation GENERAL PROPERTIES OF RECEPTORS Information conveyed by receptors . Modality . Location . Intensity . Duration ADAPTATION Reduction in rate of impulse transmission when stimulus is prolonged CLASSIFICATION OF RECEPTORS Stimulus Modality . Chemoreceptors . Thermoreceptors . Nociceptors . Mechanoreceptors . Photoreceptors CLASSIFICATION OF RECEPTORS Origin of stimuli . Exteroceptors . Interoceptors . Proprioceptors SPECIAL SENSES Vision Hearing Olfaction Gustation VISION INTRODUCTION 70% of all sensory receptors are in the eye Nearly half of the cerebral cortex is involved in processing visual information Optic nerve is one of body’s largest nerve tracts VISION INTRODUCTION The eye is a photoreceptor organ Refraction Conversion (transduction) of light into AP’s Information is interpreted in cerebral cortex Eyebrow Eyelid Eyelashes Site where conjunctiva merges with cornea Palpebral fissure Lateral commissure Eyelid Medial commissure (a) Surface anatomy of the right eye Figure 15.1a Orbicularis oculi muscle -

Microscopic Anatomy of the Eye Dog Cat Horse Rabbit Monkey Richard R Dubielzig Mammalian Globes Mammalian Phylogeny General Anatomy Dog
Microscopic Anatomy of the eye Dog Cat Horse Rabbit Monkey Richard R Dubielzig Mammalian globes Mammalian Phylogeny General Anatomy Dog Arterial Blood Vessels of the Orbit General Anatomy Dog * Horizontal section Long Posterior Ciliary a. Blood enters the globe Short Post. Ciliary a Long Post. Ciliary a. Anterior Ciliary a. Blood Supply General Anatomy Dog Major arterial circle of the iris Orbital Anatomy Dog Brain Levator Dorsal rectus Ventral rectus Zygomatic Lymph node Orbital Anatomy Dog Orbital Anatomy Dog Cartilaginous trochlea and the tendon of the dorsal oblique m. Orbital Anatomy Dog Rabbit Orbital Anatomy Dog Zygomatic salivary gland mucinous gland Orbital Anatomy Dog Gland of the Third Eyelid Eye lids (dog) Eye lids (dog) Meibomian glands at the lid margin Holocrine secretion Eye lids (primate) Upper tarsal plate Lower tarsal plate Eye lids (rabbit) The Globe The Globe Dog Cat Orangutan Diurnal Horse Diurnal Cornea Epithelium Stromal lamellae Bowman’s layer Dolphin Descemet’s m Endothelium TEM of surface epithelium Cornea Doubling of Descemet’s Vimentin + endothelium Iris Walls: The vertebrate eye Iris Sphincter m. Dilator m Blue-eye, GFAP stain Iris Collagen Iris Cat Sphinctor m. Dilator m. Iris Cat Phyomelanocytes Iris Equine Corpora nigra (Granula iridica) seen in ungulates living without shade Ciliary body Pars plicata Ciliary muscle Pars plana Ciliary body Zonular ligaments Ciliary body Primarily made of fibrillin A major component of elastin Ciliary body Alcian Blue staining acid mucopolysaccharides: Hyaluronic acid Ciliary -

Post-Miosis Changes in the Anterior Chamber Structures in Primary and Lens-Induced Secondary Chronic Angle- Closure Glaucoma
Int J Ophthalmol, Vol. 12, No. 4, Apr.18, 2019 www.ijo.cn Tel: 8629-82245172 8629-82210956 Email: [email protected] ·Brief Report· Post-miosis changes in the anterior chamber structures in primary and lens-induced secondary chronic angle- closure glaucoma Mu Li1, Xiao-Qin Yan1, Gai-Yun Li1,2, Hong Zhang1 1Department of Ophthalmology, Tongji Hospital, Tongji INTRODUCTION Medical College, Huazhong University of Science and laucoma was a leading cause of irreversible blindness Technology, Wuhan 430030, Hubei Province, China G worldwide[1-2], and could be categorized into two types: 2Retinal Department, Shanxi Eye Hospital, Taiyuan 030002, angle-closure glaucoma (ACG) and open angle glaucoma. In Shanxi Province, China Asian, ACG is more prevalent than open angle glaucoma[3-5]. In Co-first authors: Mu Li and Xiao-Qin Yan terms of ACG, it could be divided into primary and secondary Correspondence to: Gai-Yun Li. No.100, Fudong Street, types. For the pathogenesis of primary ACG, besides the Taiyuan 030002, Shanxi Province, China. [email protected]; non-pupillary block mechanisms[6-11], the major mechanism Hong Zhang. No.1095, Jiefang Road, Wuhan 430030, Hubei was pupillary block[12-13]. As an initial option for primary Province, China. [email protected] ACG treatment, miotics could induce the contraction of the Received: 2018-04-13 Accepted: 2018-12-05 sphincter pupillae, which could then pull the peripheral iris away from the trabecular meshwork and therefore reopen Abstract the angle, and finally decrease intraocular pressure (IOP) and ● To evaluate post-miosis changes in the anterior chamber control the progression of glaucoma. -

Affections of Uvea Affections of Uvea
AFFECTIONS OF UVEA AFFECTIONS OF UVEA Anatomy and physiology: • Uvea is the vascular coat of the eye lying beneath the sclera. • It consists of the uvea and uveal tract. • It consists of 3 parts: Iris, the anterior portion; Ciliary body, the middle part; Choroid, the third and the posterior most part. • All the parts of uvea are intimately associated. Iris • It is spongy having the connective tissue stroma, muscular fibers and abundance of vessels and nerves. • It is lined anteriorly by endothelium and posteriorly by a pigmented epithelium. • Its color is because of amount of melanin pigment. Mostly it is brown or golden yellow. • Iris has two muscles; the sphincter which encircles the pupil and has parasympathetic innervation; the dilator which extends from near the sphincter and has sympathetic innervation. • Iris regulates the amount of light admitted to the interior through pupil. • The iris separates the anterior chamber from the posterior chamber of the eye. Ciliary Body: • It extends backward from the base of the iris to the anterior part of the choroid. • It has ciliary muscle and the ciliary processes (70 to 80 in number) which are covered by ciliary epithelium. Choroid: • It is located between the sclera and the retina. • It extends from the ciliaris retinae to the opening of the optic nerve. • It is composed mainly of blood vessels and the pigmented tissue., The pupil • It is circular and regular opening formed by the iris and is larger in dogs in comparison to man. • It contracts or dilates depending upon the light source, due the sphincter and dilator muscles of the iris, respectively. -

Passport to Success
The following terms and other boldface terms in the chapter are defined in the Glossary accommodation choroid After careful study of this chapter, you should be able to: cochlea conjunctiva 1. Describe the function of the sensory system convergence 2. Differentiate between the special and general senses and give examples of each cornea 3. Describe the structure of the eye gustation 4. List and describe the structures that protect the eye lacrimal apparatus 5. Define refraction and list the refractive parts of the eye lens (crystalline lens) 6. Differentiate between the rods and the cones of the eye olfaction 7. Compare the functions of the extrinsic and intrinsic muscles of organ of Corti the eye ossicle 8. Describe the nerve supply to the eye proprioceptor 9. Describe the three divisions of the ear refraction 10. Describe the receptor for hearing and explain how it functions retina 11. Compare static and dynamic equilibrium and describe the sclera location and function of these receptors semicircular canal 12. Explain the function of proprioceptors sensory adaptation 13. List several methods for treatment of pain sensory receptor 14. Describe sensory adaptation and explain its value tympanic membrane 15. Show how word parts are used to build words related to the vestibule sensory system (see Word Anatomy at the end of the chapter) vitreous body PASSport to Success Visit thePoint or see the Student Resource CD in the back of this book for definitions and pronun- ciations of key terms as well as a pretest for this chapter. ® Paul’s Second Case: Seeing More of the Sun’s Effects aul glanced once again at the postcard condition, and it does have a hereditary fac- sitting on his entranceway table as he ar- tor.” The doctor dilated Paul’s eyes with drops Prived home in the evening. -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Ultrasound Biomicroscopy of the Peripheral Retina and the Ciliary Body in Degenerative Retinoschisis Associated with Pars Plana Cysts
976 Br J Ophthalmol 2001;85:976–982 Ultrasound biomicroscopy of the peripheral retina and the ciliary body in degenerative retinoschisis associated with pars plana cysts Giuseppe Mannino, Romualdo Malagola, Solmaz Abdolrahimzadeh, Gianfrancesco M Villani, Santi M Recupero Abstract pathogenetic mechanism has been attributed Aim—To evaluate the ciliary body and to circulatory disturbances, the motility of peripheral retina in degenerative retino- accommodation, vitreous traction, holes in the schisis associated with pars plana cysts inner lamina, autolysis of retinal cells in the using ultrasound biomicroscopy (UBM). peripheral retina, osmotic procedures, and Methods—18 eyes of 12 patients with transudate from the choriocapillaris.17 Histo- degenerative retinoschisis associated with chemical studies have shown that the content pars plana cysts were selected through of the cystoid spaces and schisis of the periph- binocular indirect ophthalmoscopy and eral retina is hyaluronic acid.18 The same mate- Goldmann three mirror lens examination, rial had been found in pars plana cysts,18–20 both with scleral depression. These pa- where it would accumulate owing to an active tients were studied in detail with UBM. secretion from the non-pigment epithelium of Results—Study of the ciliary body with the ciliary body and especially of the pars UBM showed pars plana cysts of diVerent plana.19 Subsequent splitting of the ciliary pig- size and uneven shape. In cross sections ment and non-pigment epithelial layers would the morphology of pars plana cysts in lead to pars plana cyst formation. Once the detail and the close relation of the cysts similarity of the content of pars plana cysts and with the oral region and the peripheral of cystoid degeneration and retinoschisis of the retina, where areas of cystoid degenera- peripheral retina had been disclosed, the tion and retinoschisis were present, were hypothesis that retinoschisis also was caused by observed. -

Ciliary Body
Ciliary body S.Karmakar HOD Introduction • Ciliary body is the middle part of the uveal tract . It is a ring (slightly eccentric ) shaped structure which projects posteriorly from the scleral spur, with a meridional width varying from 5.5 to 6.5 mm. • It is brown in colour due to melanin pigment. Anteriorly it is confluent with the periphery of the iris (iris root) and anterior part of the ciliary body bounds a part of the anterior chamber angle. Introduction • Posteriorly ciliary body has a crenated or scalloped periphery, known as ora serrata, where it is continuous with the choroid and retina. The ora serrata exhibits forward extensions,known as dentate process, which are well defined on the nasal side and less so temporally. • Ciliary body has a width of approximately 5.9 mm on the nasal side and 6.7 mm on the temporal side. Extension of the ciliary body On the outside of the eyeball, the ciliary body extends from a point about 1.5 mm posterior to the corneal limbus to a point 6.5 to 7.5 mm posterior to this point on the temporal side and 6.5 mm posterior on the nasal side. Parts of ciliary body • Ciliary body, in cross section, is a triangular structure ( in diagram it can be compared as ∆ AOI). Outer side of the triangle (O) is attached with the sclera with suprachoroidal space in between. Anterior side of the triangle (A) forms part of the anterior & posterior chamber. In its middle, the iris is attached. The inner side of the triangle (I) is divided into two parts. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
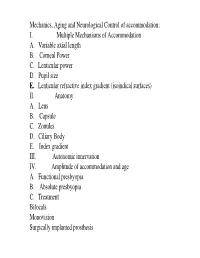
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Eye External Anatomy of Eye Accessory Structures
4/22/16 Eye Bio 40B Dr. Kandula External Anatomy of Eye Accessory Structures l Eyebrows l Levator Palpebrae Superioris - opens eye l Eyelashes l Ciliary glands – modified sweat glands l Small sebaceous glands l Sty is inflamed ciliary glands or small sebaceous glands 1 4/22/16 Terms: Lacrimal gland and duct Surface of eye Lacrimal puncta Lacrimal sac Nasolacrimal duct Nasal cavity Tears / Lacrimal fluid l a watery physiologic saline, with a plasma-like consistency, l contains the bactericidal enzyme lysozyme; l it moistens the conjunctiva and cornea, l provides nutrients and dissolved O2 to the cornea. Extrinsic Muscles of the Eye: Lateral/medial rectus Important to know Superior/inferior rectus actions and nerve Superior/inferior oblique supply in table 2 4/22/16 Extrinsic Eye Muscles • Eye movements controlled by six extrinsic eye muscles Four recti muscles § Superior rectus – moves eyeball superiorly supplied by Cranial Nerve III § Inferior rectus - moves eyeball inferiorly supplied by Cranial Nerve III § Lateral rectus - moves eyeball laterally supplied by Cranial Nerve VI § Medial rectus - moves eyeball medially supplied by Cranial Nerve III Extrinsic Eye Muscles Two oblique muscles rotate eyeball on its axis § Superior oblique rotates eyeball inferiorly and laterally and is supplied by Cranial Nerve IV § Inferior oblique rotates superiorly and laterally and is supplied by Cranial Nerve III Convergence of the Eyes l Binocular vision in humans has both eyes looking at the same object l As you look at an object close to your face,