Passport to Success
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

12 Retina Gabriele K
299 12 Retina Gabriele K. Lang and Gerhard K. Lang 12.1 Basic Knowledge The retina is the innermost of three successive layers of the globe. It comprises two parts: ❖ A photoreceptive part (pars optica retinae), comprising the first nine of the 10 layers listed below. ❖ A nonreceptive part (pars caeca retinae) forming the epithelium of the cil- iary body and iris. The pars optica retinae merges with the pars ceca retinae at the ora serrata. Embryology: The retina develops from a diverticulum of the forebrain (proen- cephalon). Optic vesicles develop which then invaginate to form a double- walled bowl, the optic cup. The outer wall becomes the pigment epithelium, and the inner wall later differentiates into the nine layers of the retina. The retina remains linked to the forebrain throughout life through a structure known as the retinohypothalamic tract. Thickness of the retina (Fig. 12.1) Layers of the retina: Moving inward along the path of incident light, the individual layers of the retina are as follows (Fig. 12.2): 1. Inner limiting membrane (glial cell fibers separating the retina from the vitreous body). 2. Layer of optic nerve fibers (axons of the third neuron). 3. Layer of ganglion cells (cell nuclei of the multipolar ganglion cells of the third neuron; “data acquisition system”). 4. Inner plexiform layer (synapses between the axons of the second neuron and dendrites of the third neuron). 5. Inner nuclear layer (cell nuclei of the bipolar nerve cells of the second neuron, horizontal cells, and amacrine cells). 6. Outer plexiform layer (synapses between the axons of the first neuron and dendrites of the second neuron). -

Current Trends in Ophthalmology Autonomic Regulation of The
Review Article Current Trends in Ophthalmology Autonomic Regulation of the Function of the Vitreous Body and Retina Lychkova AE1*, Severin AE2, Torshin VI2, Starshinov YP2, Sdobnikova SV3, Ashrafov RA4, Ashrafova SR4, Golubev YY5 Golubeva GY6 and Puzikov AM1 1Department of Health, Moscow’s Clinical Research Center, Moscow, Russia 2Russian People’s Friendship University, Moscow, Russia 3Research Institute of Eye Diseases, Moscow, Russia 4Center for Laser Surgery, Moscow, Russia 5Russian National Research Medical University, Moscow, Russia 6City Clinical Hospital, Moscow, Russia *Correspondence: Lychkova Alla Edward, Department Head of the Moscow’s Clinical Research Center, DZM, Shosse Enthusiasts 86, 111123, 11-1-53, Amundsen 129343, Moscow, Russia, Tel: (+7) 962-965-4923; E-mail: [email protected] Received: May 08, 2018; Accepted: June 25, 2018; Published: June 29, 2018 Abstract The data of the literature on the structure and physiology of the vitreous body and the retina in normal and pathological conditions are presented. The mechanism of vitreous detachment and its role in the development of vitreoretinal proliferation are described. Described adren-choline-peptide and NO-ergic mechanisms in signal transduction of the vitreous body and retina. Pharmacological and surgical methods of treatment of vitreoretinal proliferation are briefly described. Keywords: Vitreous body; Retina; Detachment; Vitreoretinal proliferation Introduction density of collagen fibers and a greater concentration of hyaluronic acid as compared to the central part. Cortical Vitreous Body (VB) is a transparent, colourless, gel- gel is comparatively more stable and more resistant to like mass containing water with an admixture of salts, age-related changes [1]. The VB contains two channels sugars, hyaluronic acid, a network of collagen fibers II, IX, (optociliary and lenticular) and three rows of cisterns, a XI types and few cells (mainly phagocytes, contributing to bursa premacularis and a precapillary space [1,3-5]. -

Affections of Uvea Affections of Uvea
AFFECTIONS OF UVEA AFFECTIONS OF UVEA Anatomy and physiology: • Uvea is the vascular coat of the eye lying beneath the sclera. • It consists of the uvea and uveal tract. • It consists of 3 parts: Iris, the anterior portion; Ciliary body, the middle part; Choroid, the third and the posterior most part. • All the parts of uvea are intimately associated. Iris • It is spongy having the connective tissue stroma, muscular fibers and abundance of vessels and nerves. • It is lined anteriorly by endothelium and posteriorly by a pigmented epithelium. • Its color is because of amount of melanin pigment. Mostly it is brown or golden yellow. • Iris has two muscles; the sphincter which encircles the pupil and has parasympathetic innervation; the dilator which extends from near the sphincter and has sympathetic innervation. • Iris regulates the amount of light admitted to the interior through pupil. • The iris separates the anterior chamber from the posterior chamber of the eye. Ciliary Body: • It extends backward from the base of the iris to the anterior part of the choroid. • It has ciliary muscle and the ciliary processes (70 to 80 in number) which are covered by ciliary epithelium. Choroid: • It is located between the sclera and the retina. • It extends from the ciliaris retinae to the opening of the optic nerve. • It is composed mainly of blood vessels and the pigmented tissue., The pupil • It is circular and regular opening formed by the iris and is larger in dogs in comparison to man. • It contracts or dilates depending upon the light source, due the sphincter and dilator muscles of the iris, respectively. -

Vitreous and Developmental Vitreoretinopathies Kevin R
CHAPTER 3 Vitreous and Developmental Vitreoretinopathies Kevin R. Tozer, Kenneth M. P. Yee, and J. Sebag Invisible (Fig. 3.1) by design, vitreous was long unseen the central vitreous and adjacent to the anterior cortical as important in the physiology and pathology of the eye. gel. HA molecules have a different distribution from col- Recent studies have determined that vitreous plays a sig- lagen, being most abundant in the posterior cortical gel nificant role in ocular health (1) and disease (1,2), includ- with a gradient of decreasing concentration centrally ing a number of important vitreoretinal disorders that and anteriorly (6,7). arise from abnormal embryogenesis and development. Both collagen and HA are synthesized during child- Vitreous embryology is presented in detail in Chapter 1. hood. Total collagen content in the vitreous gel remains Notable is that primary vitreous is filled with blood ves- at about 0.05 mg until the third decade (8). As collagen sels during the first trimester (Fig. 3.2). During the second does not appreciably increase during this time but the trimester, these vessels begin to disappear as the second- size of the vitreous does increase with growth, the den- ary vitreous is formed, ultimately resulting in an exqui- sity of collagen fibrils effectively decreases. This could sitely clear gel (Fig. 3.1). The following will review vitreous potentially weaken the collagen network and destabilize development and the congenital disorders that arise from the gel. However, since there is active synthesis of HA abnormalities in hyaloid vessel formation and regression during this time, the dramatic increase in HA concentra- during the primary vitreous stage and biochemical abnor- tion may stabilize the thinning collagen network (9). -

To See the Invisible: the Quest of Imaging Vitreous J
DOP42005.qxd 4/15/08 11:34 AM Page 5 Meyer CH (ed): Vital Dyes in Vitreoretinal Surgery. Dev Ophthalmol. Basel, Karger, 2008, vol 42, pp 5–28 To See the Invisible: The Quest of Imaging Vitreous J. Sebag VMR Institute, University of Southern California, Los Angeles, Calif., USA Abstract Purpose: Imaging vitreous has long been a quest to view what is, by design, invisible. This chapter will review important historical aspects, past and present imaging methodologies, and new technologies that are currently in development for future research and clinical applications. Methods: Classic and modern histologic techniques, dark-field slit microscopy, clinical slit lamp biomicroscopy, standard and scanning laser ophthalmoscopy (SLO), ultrasonography, optical coherence tomography (OCT), com- bined OCT-SLO, magnetic resonance and Raman spectroscopies, and dynamic light scattering method- ologies are presented. Results: The best available histologic techniques for imaging vitreous are those that avoid rapid dehydration of vitreous specimens. Dark-field slit microscopy enables in vitro imaging without dehydration or tissue fixatives. OCT enables better in vivo visualization of the vitreoretinal inter- face than SLO and ultrasonography, but does not adequately image the vitreous body. The combination of OCT with SLO has provided useful new imaging capabilities, but only at the vitreoretinal interface. Dynamic light scattering can evaluate the vitreous body by determining the average sizes of vitreous macromolecules in aging, disease, and as a means to assess the effects of pharmacologic vitreolysis. Raman spectroscopy can detect altered vitreous molecules, such as glycated collagen and other pro- teins in diabetic vitreopathy and possibly other diseases. Conclusions: A better understanding of normal vitreous physiology and structure and how these change in aging and disease is needed to develop more effective therapies and prevention. -

Embryology, Anatomy, and Physiology of the Afferent Visual Pathway
CHAPTER 1 Embryology, Anatomy, and Physiology of the Afferent Visual Pathway Joseph F. Rizzo III RETINA Physiology Embryology of the Eye and Retina Blood Supply Basic Anatomy and Physiology POSTGENICULATE VISUAL SENSORY PATHWAYS Overview of Retinal Outflow: Parallel Pathways Embryology OPTIC NERVE Anatomy of the Optic Radiations Embryology Blood Supply General Anatomy CORTICAL VISUAL AREAS Optic Nerve Blood Supply Cortical Area V1 Optic Nerve Sheaths Cortical Area V2 Optic Nerve Axons Cortical Areas V3 and V3A OPTIC CHIASM Dorsal and Ventral Visual Streams Embryology Cortical Area V5 Gross Anatomy of the Chiasm and Perichiasmal Region Cortical Area V4 Organization of Nerve Fibers within the Optic Chiasm Area TE Blood Supply Cortical Area V6 OPTIC TRACT OTHER CEREBRAL AREASCONTRIBUTING TO VISUAL LATERAL GENICULATE NUCLEUSPERCEPTION Anatomic and Functional Organization The brain devotes more cells and connections to vision lular, magnocellular, and koniocellular pathways—each of than any other sense or motor function. This chapter presents which contributes to visual processing at the primary visual an overview of the development, anatomy, and physiology cortex. Beyond the primary visual cortex, two streams of of this extremely complex but fascinating system. Of neces- information flow develop: the dorsal stream, primarily for sity, the subject matter is greatly abridged, although special detection of where objects are and for motion perception, attention is given to principles that relate to clinical neuro- and the ventral stream, primarily for detection of what ophthalmology. objects are (including their color, depth, and form). At Light initiates a cascade of cellular responses in the retina every level of the visual system, however, information that begins as a slow, graded response of the photoreceptors among these ‘‘parallel’’ pathways is shared by intercellular, and transforms into a volley of coordinated action potentials thalamic-cortical, and intercortical connections. -

Anatomy and Physiology of the Afferent Visual System
Handbook of Clinical Neurology, Vol. 102 (3rd series) Neuro-ophthalmology C. Kennard and R.J. Leigh, Editors # 2011 Elsevier B.V. All rights reserved Chapter 1 Anatomy and physiology of the afferent visual system SASHANK PRASAD 1* AND STEVEN L. GALETTA 2 1Division of Neuro-ophthalmology, Department of Neurology, Brigham and Womens Hospital, Harvard Medical School, Boston, MA, USA 2Neuro-ophthalmology Division, Department of Neurology, Hospital of the University of Pennsylvania, Philadelphia, PA, USA INTRODUCTION light without distortion (Maurice, 1970). The tear–air interface and cornea contribute more to the focusing Visual processing poses an enormous computational of light than the lens does; unlike the lens, however, the challenge for the brain, which has evolved highly focusing power of the cornea is fixed. The ciliary mus- organized and efficient neural systems to meet these cles dynamically adjust the shape of the lens in order demands. In primates, approximately 55% of the cortex to focus light optimally from varying distances upon is specialized for visual processing (compared to 3% for the retina (accommodation). The total amount of light auditory processing and 11% for somatosensory pro- reaching the retina is controlled by regulation of the cessing) (Felleman and Van Essen, 1991). Over the past pupil aperture. Ultimately, the visual image becomes several decades there has been an explosion in scientific projected upside-down and backwards on to the retina understanding of these complex pathways and net- (Fishman, 1973). works. Detailed knowledge of the anatomy of the visual The majority of the blood supply to structures of the system, in combination with skilled examination, allows eye arrives via the ophthalmic artery, which is the first precise localization of neuropathological processes. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
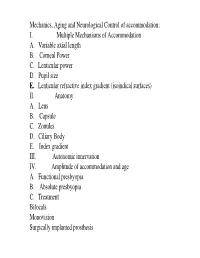
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

From Biochemistry to Clinical Relevance Search J
Chapter 16 Vitreous: From Biochemistry to Clinical Relevance Search J. SEBAG and KENNETH M. P. YEE Main Menu Table Of Contents VITREOUS BIOCHEMISTRY VITREOUS ANATOMY AGE-RELATED VITREOUS DEGENERATION VITREOUS PATHOLOGY PHARMACOLOGIC VITREOLYSIS REFERENCES Although vitreous is the largest structure within the eye, comprising 80% of its volume, our knowledge of vitreous structure and function is perhaps the least of all ocular tissues. Historically, investigations of vitreous structure have been hampered by two fundamental difficulties: first, any attempts to define vitreous morphology are attempts to visualize a tissue that is invisible by design (Fig. 1).1 Considerable barriers must be overcome to adequately study the structure of an invisible tissue. Second, the various techniques that were used previously to define vitreous structure were fraught with artifacts that biased the results of these investigations. Thus, as noted by Baurmann2 and Redslob,3 histologic studies performed during the nineteenth and early twentieth centuries were flawed by the use of tissue fixatives that caused the precipitation of what we recognize today as the glycosaminoglycan (GAG) hyaluronan (HA; formerly called hyaluronic acid). Fig. 1. Vitreous from a 9-month-old child. The sclera, choroid, and retina were dissected off the vitreous, which remains attached to the anterior segment. Because of the young age of the donor, the vitreous is almost entirely gel. Thus, the structure is solid and maintains its shape, although situated on a surgical towel exposed to room air. A band of gray tissue can be seen posterior to the ora serrata. This is peripheral retina that was firmly adherent to the vitreous base and could not be dissected away without disrupting the vitreous base. -

Eye External Anatomy of Eye Accessory Structures
4/22/16 Eye Bio 40B Dr. Kandula External Anatomy of Eye Accessory Structures l Eyebrows l Levator Palpebrae Superioris - opens eye l Eyelashes l Ciliary glands – modified sweat glands l Small sebaceous glands l Sty is inflamed ciliary glands or small sebaceous glands 1 4/22/16 Terms: Lacrimal gland and duct Surface of eye Lacrimal puncta Lacrimal sac Nasolacrimal duct Nasal cavity Tears / Lacrimal fluid l a watery physiologic saline, with a plasma-like consistency, l contains the bactericidal enzyme lysozyme; l it moistens the conjunctiva and cornea, l provides nutrients and dissolved O2 to the cornea. Extrinsic Muscles of the Eye: Lateral/medial rectus Important to know Superior/inferior rectus actions and nerve Superior/inferior oblique supply in table 2 4/22/16 Extrinsic Eye Muscles • Eye movements controlled by six extrinsic eye muscles Four recti muscles § Superior rectus – moves eyeball superiorly supplied by Cranial Nerve III § Inferior rectus - moves eyeball inferiorly supplied by Cranial Nerve III § Lateral rectus - moves eyeball laterally supplied by Cranial Nerve VI § Medial rectus - moves eyeball medially supplied by Cranial Nerve III Extrinsic Eye Muscles Two oblique muscles rotate eyeball on its axis § Superior oblique rotates eyeball inferiorly and laterally and is supplied by Cranial Nerve IV § Inferior oblique rotates superiorly and laterally and is supplied by Cranial Nerve III Convergence of the Eyes l Binocular vision in humans has both eyes looking at the same object l As you look at an object close to your face, -

Basic Anatomy & Physiology Instruction Manual
B>ÈV A˜>Ìœ“Þ >˜` *…ÞÈœ•IA˜ ˆ˜ÌÀœ Basic Anatomy & Physiology Li Ài«Àœ`ÕVi`] >`>«Ìi` ˜œÀ ÌÀ>˜ÃviÀÀi` Ìœ >˜œÌ…iÀ «>ÀÌÞ œr «>À̈ià ܈̅œÕÌ «ÀˆœÀ ÜÀˆÌÌi˜ «iÀ“ˆÃÈœ˜ œv Instruction Manual the Halth & Social Care Information Centre. An introduction for clinical coders For more information please Clinical Classifications Service contact ([email protected]) Website www.systems.hscic.gov.uk/data/clinicalcoding Reference number 3811 © Health and Social Care Information Centre Date of issue August 2014 Anatomical illustrations © Health and Social Care Information Centre and Peak Dean Associates. They may not be reproduced, adapted nor transferred to another party or parties without written permission of Health and Social Care Information Centre. 1 Foreword This manual is intended to be used as a basic instruction tool, rather than a comprehensive course of study or a reference book. It will help promote an understanding of diseases and operations described in casenotes by providing information on body systems, how they work together, and the terminology used to describe them. The intended result is that those responsible for clinical coding will be better able to translate these concepts into the appropriate clinical codes. Contents Section 1..................................................................................................................................................................................................................................................... 5 Introduction to Medical Terminology, Anatomy