Snakebite Management in Nepal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Snake Bite Protocol
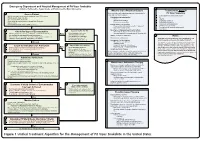
Lavonas et al. BMC Emergency Medicine 2011, 11:2 Page 4 of 15 http://www.biomedcentral.com/1471-227X/11/2 and other Rocky Mountain Poison and Drug Center treatment of patients bitten by coral snakes (family Ela- staff. The antivenom manufacturer provided funding pidae), nor by snakes that are not indigenous to the US. support. Sponsor representatives were not present dur- At the time this algorithm was developed, the only ing the webinar or panel discussions. Sponsor represen- antivenom commercially available for the treatment of tatives reviewed the final manuscript before publication pit viper envenomation in the US is Crotalidae Polyva- ® for the sole purpose of identifying proprietary informa- lent Immune Fab (ovine) (CroFab , Protherics, Nash- tion. No modifications of the manuscript were requested ville, TN). All treatment recommendations and dosing by the manufacturer. apply to this antivenom. This algorithm does not con- sider treatment with whole IgG antivenom (Antivenin Results (Crotalidae) Polyvalent, equine origin (Wyeth-Ayerst, Final unified treatment algorithm Marietta, Pennsylvania, USA)), because production of The unified treatment algorithm is shown in Figure 1. that antivenom has been discontinued and all extant The final version was endorsed unanimously. Specific lots have expired. This antivenom also does not consider considerations endorsed by the panelists are as follows: treatment with other antivenom products under devel- opment. Because the panel members are all hospital- Role of the unified treatment algorithm -

Use of Molecular Diagnostic Tools for the Identification of Species Responsible for Snakebite in Nepal: a Pilot Study
RESEARCH ARTICLE Use of Molecular Diagnostic Tools for the Identification of Species Responsible for Snakebite in Nepal: A Pilot Study Sanjib Kumar Sharma1, Ulrich Kuch2, Patrick Höde2, Laura Bruhse2, Deb P. Pandey3,4, Anup Ghimire1, François Chappuis5, Emilie Alirol5,6* 1 B.P. Koirala Institute of Health Sciences, Dharan, Nepal, 2 Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe University, Frankfurt am Main, Germany, 3 Senckenberg Biodiversity and Climate Research Centre (BiK-F), Frankfurt am Main, Germany, 4 Senckenberg Forschungsinstitut, Frankfurt am Main, Germany, 5 Division of Tropical and Humanitarian Medicine, a11111 University Hospitals of Geneva, Geneva, Switzerland, 6 Médecins Sans Frontières UK, London, United Kingdom * [email protected] Abstract OPEN ACCESS Snakebite is an important medical emergency in rural Nepal. Correct identification of the bit- Citation: Sharma SK, Kuch U, Höde P, Bruhse L, ing species is crucial for clinicians to choose appropriate treatment and anticipate complica- Pandey DP, Ghimire A, et al. (2016) Use of Molecular tions. This is particularly important for neurotoxic envenoming which, depending on the Diagnostic Tools for the Identification of Species Responsible for Snakebite in Nepal: A Pilot Study. snake species involved, may not respond to available antivenoms. Adequate species identi- PLoS Negl Trop Dis 10(4): e0004620. doi:10.1371/ fication tools are lacking. This study used a combination of morphological and molecular journal.pntd.0004620 approaches (PCR-aided DNA sequencing from swabs of bite sites) to determine the contri- Editor: H Janaka de Silva, University of Kelaniya, bution of venomous and non-venomous species to the snakebite burden in southern Nepal. -

WHO Guidance on Management of Snakebites
GUIDELINES FOR THE MANAGEMENT OF SNAKEBITES 2nd Edition GUIDELINES FOR THE MANAGEMENT OF SNAKEBITES 2nd Edition 1. 2. 3. 4. ISBN 978-92-9022- © World Health Organization 2016 2nd Edition All rights reserved. Requests for publications, or for permission to reproduce or translate WHO publications, whether for sale or for noncommercial distribution, can be obtained from Publishing and Sales, World Health Organization, Regional Office for South-East Asia, Indraprastha Estate, Mahatma Gandhi Marg, New Delhi-110 002, India (fax: +91-11-23370197; e-mail: publications@ searo.who.int). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. -

The Distribution of Reptiles and Amphibians in the Annapurna-Dhaulagiri Region (Nepal)
THE DISTRIBUTION OF REPTILES AND AMPHIBIANS IN THE ANNAPURNA-DHAULAGIRI REGION (NEPAL) by LURLY M.R. NANHOE and PAUL E. OUBOTER L.M.R. Nanhoe & P.E. Ouboter: The distribution of reptiles and amphibians in the Annapurna-Dhaulagiri region (Nepal). Zool. Verh. Leiden 240, 12-viii-1987: 1-105, figs. 1-16, tables 1-5, app. I-II. — ISSN 0024-1652. Key words: reptiles; amphibians; keys; Annapurna region; Dhaulagiri region; Nepal; altitudinal distribution; zoogeography. The reptiles and amphibians of the Annapurna-Dhaulagiri region in Nepal are keyed and described. Their distribution is recorded, based on both personal observations and literature data. The ecology of the species is discussed. The zoogeography and the altitudinal distribution are analysed. All in all 32 species-group taxa of reptiles and 21 species-group taxa of amphibians are treated. L.M.R. Nanhoe & P.E. Ouboter, c/o Rijksmuseum van Natuurlijke Historie Raamsteeg 2, Postbus 9517, 2300 RA Leiden, The Netherlands. CONTENTS Introduction 5 Study area 7 Climate and vegetation 9 Material and methods 12 Reptilia 13 Sauria 13 Gekkonidae 13 Hemidactylus brookii 14 Hemidactylus flaviviridis 14 Hemidactylus garnotii 15 Agamidae 15 Agama tuberculata 16 Calotes versicolor 18 Japalura major 19 Japalura tricarinata 20 Phrynocephalus theobaldi 22 Scincidae 24 Scincella capitanea 25 Scincella ladacensis ladacensis 26 3 4 ZOOLOGISCHE VERHANDELINGEN 240 (1987) Scincella ladacensis himalayana 27 2g Scincella sikimmensis ^ Sphenomorphus maculatus ^ Serpentes ^ Colubridae ^ Amphiesma platyceps ^ -

Long-Term Effects of Snake Envenoming
toxins Review Long-Term Effects of Snake Envenoming Subodha Waiddyanatha 1,2, Anjana Silva 1,2 , Sisira Siribaddana 1 and Geoffrey K. Isbister 2,3,* 1 Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Saliyapura 50008, Sri Lanka; [email protected] (S.W.); [email protected] (A.S.); [email protected] (S.S.) 2 South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, University of Peradeniya, Peradeniya 20400, Sri Lanka 3 Clinical Toxicology Research Group, University of Newcastle, Callaghan, NSW 2308, Australia * Correspondence: [email protected] or [email protected]; Tel.: +612-4921-1211 Received: 14 March 2019; Accepted: 29 March 2019; Published: 31 March 2019 Abstract: Long-term effects of envenoming compromise the quality of life of the survivors of snakebite. We searched MEDLINE (from 1946) and EMBASE (from 1947) until October 2018 for clinical literature on the long-term effects of snake envenoming using different combinations of search terms. We classified conditions that last or appear more than six weeks following envenoming as long term or delayed effects of envenoming. Of 257 records identified, 51 articles describe the long-term effects of snake envenoming and were reviewed. Disability due to amputations, deformities, contracture formation, and chronic ulceration, rarely with malignant change, have resulted from local necrosis due to bites mainly from African and Asian cobras, and Central and South American Pit-vipers. Progression of acute kidney injury into chronic renal failure in Russell’s viper bites has been reported in several studies from India and Sri Lanka. Neuromuscular toxicity does not appear to result in long-term effects. -

Venomous Snakes
Venomous Snakes - By Kedar Bhide Kedar Bhide is a snake expert from Mumbai. A postgraduate from Mumbai's Haffkine Institute, his work has resulted into first records of 2 snake species for India, Barta (Kaulback's Pit Viper) from Arunachal Pradesh and the Sind Awl-headed snake from Rajasthan. “ Moments after being bitten, the man feels a live fire germinating in the wound as if red hot tongs contorted his flesh; that which was mortified enlarges to monstrosity, and lividness invades him. The unfortunate victim witnesses his body becoming corpse piece by piece; a chill of death invades all his being, and soon bloody threads fall from his gums; and his eyes, without intending to, will also cry blood, until, beaten by suffering and anguish, he loses the sense of reality. If we then ask the unlucky man something, he may see us through blurred eyes, but we get no response; and perhaps a final sweat of red pearls or a mouthful of blackish blood warns of impending” (This is an introduction of a book written in 1931 by a Costa Rican Biologists and snakebite expert Clodomiro Picado.) INTRODUCTION Human fear of snakes is caused almost entirely by those species that can deliver a venomous bite. It is somewhat ironic that such a minority group, like venomous snakes has endangered the whole kingdom of snakes. Let us start by correcting a frequent misnomer. People often refer to poisonous snakes, and indeed by directory definition, this is not incorrect. But as a student of herpetology we should be more specific in our terminology. -

Snakebite: the World's Biggest Hidden Health Crisis
Snakebite: The world's biggest hidden health crisis Snakebite is a potentially life-threatening neglected tropical disease (NTD) that is responsible for immense suffering among some 5.8 billion people who are at risk of encountering a venomous snake. The human cost of snakebite Snakebite Treatment Timeline Each year, approximately 5.4 million people are bitten by a snake, of whom 2.7 million are injected with venom. The first snake antivenom This leads to 400,000 people being permanently dis- produced, against the Indian Cobra. abled and between 83,000-138,000 deaths annually, Immunotherapy with animal- mostly in sub-Saharan Africa and South Asia. 1895 derived antivenom has continued to be the main treatment for snakebite evenoming for 120 years Snakebite: both a consequence and a cause of tropical poverty The Fav-Afrique antivenom, 2014 produced by Sanofi Pasteur (France) Survivors of untreated envenoming may be left with permanently discontinued amputation, blindness, mental health issues, and other forms of disability that severely affect their productivity. World Health Organization Most victims are agricultural workers and children in 2018 (WHO) lists snakebite envenoming the poorest parts of Africa and Asia. The economic as a neglected tropical disease cost of treating snakebite envenoming is unimaginable in most communities and puts families and communi- ties at risk of economic peril just to pay for treatment. WHO launches a strategy to prevent and control snakebite envenoming, including a program targeting affected communities and their health systems Global antivenom crisis 2019 The world produces less than half of the antivenom it The Scientific Research Partnership needs, and this only covers 57% of the world’s species for Neglected Tropical Snakbites of venomous snake. -

Bitis Arietans) Venom, and Their Neutralization by Antivenom
Toxins 2014, 6, 1586-1597; doi:10.3390/toxins6051586 OPEN ACCESS toxins ISSN 2072-6651 www.mdpi.com/journal/toxins Article In Vitro Toxic Effects of Puff Adder (Bitis arietans) Venom, and Their Neutralization by Antivenom Steven Fernandez 1, Wayne Hodgson 1, Janeyuth Chaisakul 2, Rachelle Kornhauser 1, Nicki Konstantakopoulos 1, Alexander Ian Smith 3 and Sanjaya Kuruppu 3,* 1 Department of Pharmacology, Monash University, Building 13E, Wellington Road, Clayton, Vic 3800, Australia; E-Mails: [email protected] (S.F.); [email protected] (W.H.); [email protected] (R.K.); [email protected] (N.K.) 2 Department of Pharmacology, Phramongkutklao College of Medicine, Bangkok 10400, Thailand; E-Mail: [email protected] 3 Department of Biochemistry & Molecular Biology, Monash University, Building 77, Wellington Road, Clayton, Vic 3800, Australia; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel: +61-3-9902-9372; Fax: + 61-3-9902-9500. Received: 24 November 2013; in revised form: 6 April 2014 / Accepted: 4 May 2014 / Published: 19 May 2014 Abstract: This study investigated the in vitro toxic effects of Bitis arietans venom and the ability of antivenom produced by the South African Institute of Medical Research (SAIMR) to neutralize these effects. The venom (50 µg/mL) reduced nerve-mediated twitches of the chick biventer muscle to 19% ± 2% of initial magnitude (n = 4) within 2 h. This inhibitory effect of the venom was significantly attenuated by prior incubation of tissues with SAIMR antivenom (0.864 µg/µL; 67% ± 4%; P < 0.05; n = 3–5, unpaired t-test). -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -

Bridging Livelihoods and Forest Conservation in Protected Areas: Exploring the Role and Scope of Non-Timber Forest Products
Bridging Livelihoods and Forest Conservation in Protected Areas: Exploring the role and scope of non-timber forest products Field experience from Satchari National Park, Habiganj, Bangladesh A dissertation paper submitted for the partial fulfillment of B.Sc. (Honors) in Forestry Submitted by Sharif Ahmed Mukul Registration no: 2001631031 Bridging Livelihoods and Forest Conservation in Protected Areas: Exploring the role and scope of non-timber forest products Field experience from Satchari National Park, Habiganj, Bangladesh Research Paper Prepared and Submitted by Sharif Ahmed Mukul Registration no. 2001631031 Department of Forestry School of Agriculture and Mineral Sciences Shahjalal University of Science and Technology May, 2007 ii Certification This is to certify that this paper entitled, ‘Bridging Livelihoods and Forest Conservation in Protected Areas: Exploring the role and scope for non-timber forest products’ is an original paper prepared by Registration no. 2001631031 (Session 2001- 02) based on his field study at Satchari National Park, Habiganj, Bangladesh for the partial fulfillment of his B.Sc. (Hons.) in Forestry degree at Shahjalal University of Science and Technology, Sylhet, Bangladesh. He has completed the work under my supervision and I do hereby approve the style and contents of this paper. A.Z.M. Manzoor Rashid Assistant Professor Department of Forestry iii Declaration This is to declare that, it is an original paper prepared by myself based on my one year field investigations at Satchari National Park, Habiganj, Bangladesh; to submit as a requirement for the partial fulfillment of B. Sc. (Hons.) degree in the Department of Forestry at School of Agriculture and Mineral Sciences of Shahjalal University of Science and Technology, Sylhet, Bangladesh. -

Epidemiology and Clinical Outcomes of Snakebite in the Elderly: a Toxic Database Study
Clinical Toxicology ISSN: 1556-3650 (Print) 1556-9519 (Online) Journal homepage: http://www.tandfonline.com/loi/ictx20 Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones To cite this article: Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones (2018) Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study, Clinical Toxicology, 56:2, 108-112, DOI: 10.1080/15563650.2017.1342829 To link to this article: https://doi.org/10.1080/15563650.2017.1342829 Published online: 13 Jul 2017. Submit your article to this journal Article views: 120 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx20 CLINICAL TOXICOLOGY, 2018 VOL. 56, NO. 2, 108–112 https://doi.org/10.1080/15563650.2017.1342829 CLINICAL RESEARCH Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC Ã database study Meghan B. Spyresa, Anne-Michelle Ruhab, Kurt Kleinschmidtc, Rais Vohrad, Eric Smithc and Angela Padilla-Jonesb aDepartment of Emergency Medicine, Division of Medical Toxicology, University of Southern California, Los Angeles, CA, USA; bDepartment of Medical Toxicology, Banner-University Medical Center Phoenix, Phoenix, AZ, USA; cDepartment of Emergency Medicine, Univesity of Texas Southwestern Medical Center, Dallas, TX, USA; dDepartment of Emergency Medicine, UCSF Fresno Medical Center, Fresno, CA, USA ABSTRACT ARTICLE HISTORY Introduction: Epidemiologic studies of snakebites in the United States report typical victims to be Received 23 February 2017 young men. -

On the Occurrences of Japalura Kumaonensis and Japalura Tricarinata (Reptilia: Sauria: Draconinae) in China
Herpetologica, 74(2), 2018, 181–190 Ó 2018 by The Herpetologists’ League, Inc. On the Occurrences of Japalura kumaonensis and Japalura tricarinata (Reptilia: Sauria: Draconinae) in China 1,2 3,4 5 6 7 3,4 1 KAI WANG ,KE JIANG ,V.DEEPAK ,DAS ABHIJIT ,MIAN HOU ,JING CHE , AND CAMERON D. SILER 1 Sam Noble Oklahoma Museum of Natural History and Department of Biology, University of Oklahoma, Norman, OK 73072, USA 3 Kunming Institute of Zoology, Chinese Academy of Sciences, Kunming, Yunnan 650223, China 4 Southeast Asia Biodiversity Research Institute, Chinese Academy of Sciences, Menglun, Yunnan 666303, China 5 Center for Ecological Sciences, Indian Institute of Science, Bangalore, Karnataka 560012, India 6 Wildlife Institute of India, Chandrabani, Dehradun 248002, India 7 Academy of Continuing Education, Sichuan Normal University, Chengdu, Sichuan 610068, China ABSTRACT: Although the recognized distribution of Japalura kumaonensis is restricted largely to western Himalaya, a single, isolated outlier population was reported in eastern Himalaya at the China-Nepal border in southeastern Tibet, China in Zhangmu, Nyalam County. Interestingly, subsequent studies have recognized another morphologically similar species, J. tricarinata, from the same locality in Tibet based on photographic evidence only. Despite these reports, no studies have examined the referred specimens for either record to confirm their taxonomic identifications with robust comparisons to congener species. Here, we examine the referred specimen of the record of J. kumaonensis from southeastern Tibet, China; recently collected specimens from the same locality in southeastern Tibet; type specimens; and topotypic specimens of both J. kumaonensis and J. tricarinata, to clarify the taxonomic identity of the focal population from southeastern Tibet, China.