Full Set of Board Papers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Item 7: Inverness Royal Academy Associated School Group Overview
The Highland Council Agenda Item City of Inverness Area Committee – 3 June 2014 Report No Inverness Royal Academy Associated School Group Overview Report by Joint Director of Care and Learning Summary This report provides an update of key information in relation to the schools within the Inverness Royal Academy Associated School Group (ASG), and provides useful updated links to further information in relation to these schools. 1.0 ASG PROFILE The primary schools in this area serve over 1340 pupils, with the secondary school serving 926 young people. ASG roll projections can be found at: http://www.highland.gov.uk/yourcouncil/highlandfactsandfigures/schoolrollforecasts. htm There are currently 3 Head Teacher vacancies in the ASG and all schools receive support through the Quality Improvement Team and the Area Office. 1.1 Attainment and Achievement 1.1.1 Inverness Royal Academy School Aim: Inverness Royal Academy strives to bring out the best in all of our pupils. In pursuing this broad aim the school intends to contribute significantly to the preparation of pupils for various adult roles in society, namely continuing education, employment, leisure, parenthood and citizenship. It also hopes to give them a sense of the heritage which stems from their Scottish and, in particular, Highland environment and from the long traditions of the school, whilst at the same time fostering awareness of the place of our society in the wider international community. The school aim is underpinned by the following core values; Respect, Compassion, Responsibility, Commitment and Honesty. Attainment – Performance Summary (Session 2012/13): National Priority Measures Level 7 = Advanced Higher Level 6 = Higher Level 5 = Standard Grade Credit / Intermediate 2 Level 4 = Standard Grade General / Intermediate 1 Level 3 = Standard Grade Foundation / Access 3 There is an increased percentage of pupils gaining English and Maths at Foundation or Access 3 level rising from 94% last year to 99% in 2013. -

Inverness Local Plan Public Local Inquiry Report- Volume 3
TOWN AND COUNTRY PLANNING (SCOTLAND) ACT 1997 REPORT OF PUBLIC LOCAL INQUIRY INTO OBJECTIONS TO THE INVERNESS LOCAL PLAN VOLUME 3 THE HINTERLAND AND THE RURAL DEVELOPMENT AREA Reporter: Janet M McNair MA(Hons) MPhil MRTPI File reference: IQD/2/270/7 Dates of the Inquiry: 14 April 2004 to 20 July 2004 CONTENTS VOLUME 3 Abbreviations The A96 Corridor Chapter 24 Land north and east of Balloch 24.1 Land between Balloch and Balmachree 24.2 Land at Lower Cullernie Farm Chapter 25 Inverness Airport and Dalcross Industrial Estate 25.1 Inverness Airport Economic Development Initiative 25.2 Airport Safeguarding 25.3 Extension to Dalcross Industrial Estate Chapter 26 Former fabrication yard at Ardersier Chapter 27 Morayhill Chapter 28 Lochside The Hinterland Chapter 29 Housing in the Countryside in the Hinterland 29.1 Background and context 29.2 objections to the local plan’s approach to individual and dispersed houses in the countryside in the Hinterland Objections relating to locations listed in Policy 6:1 29.3 Upper Myrtlefield 29.4 Cabrich 29.5 Easter Clunes 29.6 Culburnie 29.7 Ardendrain 29.8 Balnafoich 29.9 Daviot East 29.10 Leanach 29.11 Lentran House 29.12 Nairnside 29.13 Scaniport Objections relating to locations not listed in Policy 6.1 29.14 Blackpark Farm 29.15 Beauly Barnyards 29.16 Achmony, Balchraggan, Balmacaan, Bunloit, Drumbuie and Strone Chapter 30 Objections Regarding Settlement Expansion Rate in the Hinterland Chapter 31 Local centres in the Hinterland 31.1 Beauly 31.2 Drumnadrochit Chapter 32 Key Villages in the Hinterland -

Birchcroft Balnain, Inverness, Iv63
BIRCHCROFT BALNAIN INVERNESS IV63 6TJ Energy performance certificate YouEnergy can use this Performance document to: Certificate (EPC) Scotland Dwellings BIRCHCROFT, BALNAIN, INVERNESS, IV63 6TJ Dwelling type: Detached house Reference number: 2818-6424-5000-0626-2902 Date of assessment: 06 April 2018 Type of assessment: RdSAP, existing dwelling Date of certificate: 11 April 2018 Approved Organisation: Elmhurst Total floor area: 202 m2 Main heating and fuel: Boiler and radiators, oil Primary Energy Indicator: 176 kWh/m2/year You can use this document to: • Compare current ratings of properties to see which are more energy efficient and environmentally friendly • Find out how to save energy and money and also reduce CO2 emissions by improving your home Estimated energy costs for your home for 3 years* £3,723 See your recommendations report for more Over 3 years you could save* £321 information * based upon the cost of energy for heating, hot water, lighting and ventilation, calculated using standard assumptions Very energy efficient - lower running costs Current Potential Energy Efficiency Rating (92 plus) A This graph shows the current efficiency of your home, (81-91) B 90 taking into account both energy efficiency and fuel costs. The higher this rating, the lower your fuel bills (69-80) C are likely to be. 70 (55-68) D Your current rating is band C (70). The average rating for EPCs in Scotland is band D (61). (39-54 E (21-38) The potential rating shows the effect of undertaking all F of the improvement measures listed within your (1-20) G recommendations report. Not energy efficient - higher running costs Very environmentally friendly - lower CO emissions Current Potential 2 Environmental Impact (CO2) Rating (92 plus) A This graph shows the effect of your home on the (81-91) B environment in terms of carbon dioxide (CO2) 83 emissions. -

Gàidhlig (Scottish Gaelic) Local Studies Vol
Gàidhlig (Scottish Gaelic) Local Studies Vol. 22 : Cataibh an Ear & Gallaibh Gàidhlig (Scottish Gaelic) Local Studies 1 Vol. 22: Cataibh an Ear & Gallaibh (East Sutherland & Caithness) Author: Kurt C. Duwe 2nd Edition January, 2012 Executive Summary This publication is part of a series dealing with local communities which were predominantly Gaelic- speaking at the end of the 19 th century. Based mainly (but not exclusively) on local population census information the reports strive to examine the state of the language through the ages from 1881 until to- day. The most relevant information is gathered comprehensively for the smallest geographical unit pos- sible and provided area by area – a very useful reference for people with interest in their own communi- ty. Furthermore the impact of recent developments in education (namely teaching in Gaelic medium and Gaelic as a second language) is analysed for primary school catchments. Gaelic once was the dominant means of conversation in East Sutherland and the western districts of Caithness. Since the end of the 19 th century the language was on a relentless decline caused both by offi- cial ignorance and the low self-confidence of its speakers. A century later Gaelic is only spoken by a very tiny minority of inhabitants, most of them born well before the Second World War. Signs for the future still look not promising. Gaelic is still being sidelined officially in the whole area. Local council- lors even object to bilingual road-signs. Educational provision is either derisory or non-existent. Only constant parental pressure has achieved the introduction of Gaelic medium provision in Thurso and Bonar Bridge. -

St Kilda World Heritage Site Management Plan 2012–17 Title Sub-Title Foreword
ST KILDA World Heritage Site Management Plan 2012–17 TITLE Sub-title FOREWORD We are delighted to be able to present the revised continuing programme of research and conservation. Management Plan for the St Kilda World Heritage Site The management of the World Heritage Site is, for the years 2012-2017. however, a collaborative approach also involving partners from Historic Scotland, Scottish Natural St Kilda is a truly unique place. The spectacular Heritage, Comhairle nan Eilean Siar and the Ministry of scenery and wildlife, both on land and in the seas Defence. As custodians of St Kilda, all of the partners surrounding the islands, the archipelago’s isolation and should be thanked for their excellent work over recent inaccessibility, and the evidence, abundant for all to years, and the new Management Plan will continue to see, of the people that made these islands their home, build on these efforts. make St Kilda truly exceptional. The very nature of St Kilda means that the challenges In this respect, St Kilda showcases Scotland to the are different to those of other World Heritage Sites. world by displaying the most important features of our By identifying and addressing key short and medium heritage, our rich natural and cultural traditions, and our term issues around protection, conservation and awe inspiring landscapes and scenery. management, the Management Plan aims to embrace these challenges, and sets out a thirty year vision for the It is therefore of no surprise that St Kilda has been property, ensuring that the longer-term future of St Kilda designated as a World Heritage Site for both its cultural is properly considered. -
Place-Names of Inverness and Surrounding Area Ainmean-Àite Ann an Sgìre Prìomh Bhaile Na Gàidhealtachd
Place-Names of Inverness and Surrounding Area Ainmean-àite ann an sgìre prìomh bhaile na Gàidhealtachd Roddy Maclean Place-Names of Inverness and Surrounding Area Ainmean-àite ann an sgìre prìomh bhaile na Gàidhealtachd Roddy Maclean Author: Roddy Maclean Photography: all images ©Roddy Maclean except cover photo ©Lorne Gill/NatureScot; p3 & p4 ©Somhairle MacDonald; p21 ©Calum Maclean. Maps: all maps reproduced with the permission of the National Library of Scotland https://maps.nls.uk/ except back cover and inside back cover © Ashworth Maps and Interpretation Ltd 2021. Contains Ordnance Survey data © Crown copyright and database right 2021. Design and Layout: Big Apple Graphics Ltd. Print: J Thomson Colour Printers Ltd. © Roddy Maclean 2021. All rights reserved Gu Aonghas Seumas Moireasdan, le gràdh is gean The place-names highlighted in this book can be viewed on an interactive online map - https://tinyurl.com/ybp6fjco Many thanks to Audrey and Tom Daines for creating it. This book is free but we encourage you to give a donation to the conservation charity Trees for Life towards the development of Gaelic interpretation at their new Dundreggan Rewilding Centre. Please visit the JustGiving page: www.justgiving.com/trees-for-life ISBN 978-1-78391-957-4 Published by NatureScot www.nature.scot Tel: 01738 444177 Cover photograph: The mouth of the River Ness – which [email protected] gives the city its name – as seen from the air. Beyond are www.nature.scot Muirtown Basin, Craig Phadrig and the lands of the Aird. Central Inverness from the air, looking towards the Beauly Firth. Above the Ness Islands, looking south down the Great Glen. -

Draft CCC Minutes SEPT 2016
Draft Minutes for approval CREICH COMMUNITY COUNCIL Minutes of meeting held on Tuesday 20th September 2016 at 7.30pm in Rosehall Village Hall Present: Pete Campbell, Chair, (PC), Ron Boothroyd, Vice Chair (RB), Russell Taylor, Treasurer, Also present: Michael Baird (MB), Norman Vincent (NV), Jennifer Munro (JM) Police Scotland: PC Dave Thompson (DT) and PC Chris Wylie (CW) Apologies: Russell Smith (RS), John White (JW), Norman MacDonald (NM), Brian Coghill (BC) and Highland Councillor George Farlow (GF) Secretary: Mary Goulder (MG) Item 1. Welcome/Apologies (as above)/Police report (See below). Pete Campbell welcomed everyone but recorded that the meeting was not quorate due to the apologies received from elected members. It was agreed to conduct the meeting to the best ability of those members present and that no decisions could be taken without the opinions of the others. An email will be circulated after the meeting with any recommendations made to seek approval/rejection as appropriate. MG Action. Item 2. Minutes of August meeting/matters arising (if not on agenda). The minutes of the August meeting were approved, as a true and accurate record; proposed: Russell Taylor, seconded: Ron Boothroyd. (1) Invitation to THC Roads Manager and Police Scotland Area Commander. This is proposed for the October CC meeting (18th) and invitations will be issued. MG Action. From the floor NV asked to register is complaint that since he raised the traffic issues in Bonar at the June meeting, to date no action has been taken by the CC. Chair advised that had been agreed at the last meeting that the North Area Commander Police Scotland and the Head of Roads at Highland Council would be invited to attend the October meeting. -
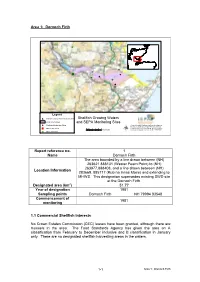
Area 1: Dornoch Firth Shellfish Growing Waters and SEPA Monitoring Sites Report Reference No. 1 Name Dornoch Firth Location
Area 1: Dornoch Firth ^_ ^_ ^_ ^_ ^_ ^_^_ ! ^_ # ^_ # ^_ ^_ Legend # Shellfish Growing Waters Monitoring Sites Shellfish Growing Waters Shellfish Growing Waters and SEPA Monitoring Sites ! Shellfish Production Sites (c) 2004 Scottish Environment Protection Agency. Includes material based upon Ordnance Survey " Marine Fish Farms 00.51 2 3 4 5 mapping with permission of H.M. Stationery Office. Kilometers (c) Crown Copyright. Licence number 100020538. ^_ Major Discharges µ Report reference no. 1 Name Dornoch Firth The area bounded by a line drawn between (NH) 263621 888131 (Wester Fearn Point) to (NH) 263977,888408, and a line drawn between (NH) Location Information 283669, 885717 (Rub na Innse Moire) and extending to MHWS. This designation supersedes existing SWD site at the Dornoch Firth. Designated area (km2) 51.77 Year of designation 1981 Sampling points Dornoch Firth NH 79994 83548 Commencement of 1981 monitoring 1.1 Commercial Shellfish Interests No Crown Estates Commission (CEC) leases have been granted, although there are mussels in the area. The Food Standards Agency has given the area an A classification from February to December inclusive and B classification in January only. There are no designated shellfish harvesting areas in the waters. 1- 1 Area 1: Dornoch Firth 1.2 Bathymetric Information This shellfish water encompasses almost the entire area of the Dornoch Firth. The area is some 22 km long by a maximum of 5.5 km wide. The maximum charted depth (at LAT) is <10 m. Approximately half of the area is <0 m chart depth, ie intertidal area exposed at low tide. -

Ardgay District
ARDGAY & DISTRICT Community Council newsletter Price: £1.00 ISSN (Online) 2514-8400 = Issue No. 36 = SUMMER 2017 = New Hub opening this summer The new Kyle of Sutherland Hub is almost com- plete. Here is a taste of what is to come. THE TEAM HAVE BEEN appointed Ann Renouf, Café Supervisor, and we would like to welcome Emma Mackay, General As- Adele Newlands, Hub Manag- sistant, and Clark Goodison, er; Vicky Karl, Café Manager; Cleaner. (Continue on page 9) The bright red Hub, as seen from Tulloch. THE CURRENT CC WAS FORMED IN FEBRUARy 2016 Achievements and challenges of your Community Council from June 2016 WE REPRODUCE Betty the issues discussed at Wright’s annual report our meetings? Which from our AGM. Our will feature in next year’s Chairperson thanks all agendas? We have cre- who have given freely of ated a map highlighting their time to CC business. the work of your CC in (Pages 4-6) What were 2016-2017. (Page 5). Opening of the Falls of Shin Visitor Attraction. The work of the Kyle of Plans to supply access to Sutherland Development Trust Superfast broadband to all Helen Houston reports on current and future projects What to do if you have been ‘left out’ Page 8 of the Trust (Pages 14-15) Beginning of the works on the Business Barn & Art Shed in Ardgay (Page 11) Know more about East Sutherland Energy Advice Service (Page 17) George Farlow’s farewell message Page 7 All you need Volunteering a to know opportunities 32 pages featuring Letters to the Editor, about horses in your Opening times, on the road area Telephone guide, Bus & Train timetable, Page 10 Page 20 Crosswords, Sudoku.. -

Highland Primary Care Nhs Trust
PHARMACY PRACTICES COMMITTEE MEETING Tuesday, 30 October, 2012 at 1.30 pm Seminar Room, Migdale Hospital, Cherry Grove, Bonar Bridge, IV24 3ER Application by Gareth Dixon of MITCHELLS CHEMIST LTD for the provision of general pharmaceutical services at The Former Bonar Bridge News, Dornoch Road, Bonar Bridge, IV24 3EB PRESENT Okain Maclennan (Chair) Margaret Thomson (Lay Member) Michael Roberts (Lay member) Susan Taylor (GP Sub Committee Nominate) Fiona Thomson (APC Non Contractor Nominate) John McNulty (APC Contractor Nominate) In Attendance Andrew J Green (Area Regulations, Contracts & Controlled Drugs Governance Pharmacist) Helen M MacDonald (Community Pharmacy Business Manager) Gareth Dixon, Mitchells Chemist Ltd, Applicant Donna Gillespie, Mitchells Chemist Ltd, Applicant Support Christopher Mair, GP Sub Committee Andrew Paterson, Area Pharmaceutical Committee Observers Nicola Macdonald (APC Contractor Nominate NHS Highland PPC Member in training) 1. The Chair welcomed everyone to Bonar Bridge. He asked all members to confirm that they had all received the papers for the hearing and had read and considered them. All members affirmed these points. 2. APPLICATION FOR INCLUSION IN THE BOARD’S PHARMACEUTICAL LIST Case No: PPC – Bonar Bridge, Sutherland. Mitchells Chemist Ltd, The former Bonar Bridge News, Dornoch Road, Bonar Bridge, IV24 3EB. The Chair asked each Committee member if there were any interests to declare in relation to the application being heard from Mitchells Chemist Ltd. No interests were declared. 3. The Committee was asked to consider the application submitted by Mitchells Chemist Ltd to provide general pharmaceutical services from premises sited at The former Bonar Bridge News, Dornoch Road, Bonar Bridge, IV24 3EB under Regulation 5(10) of the National Health Service (Pharmaceutical Services) (Scotland) Regulations 2009, as amended. -

2014 2 Friendly Companion January 2014
TThhee Friendly Companion Friendly Companion “The L ORD hath made all things for Himself.” (Proverbs 16. 4.) January 2014 2 Friendly Companion January 2014 Editor: Mr. G.D. Buss, “Bethany,” 7 Laines Head, Chippenham, Wiltshire, SN15 1PH. Tel: 01249 656910. Email: [email protected] All correspondence (except that which relates to subscriptions) to be sent to the Editor. Annual Subscriptions inc. postage: U.K. U.S.A. & Canada Australia Europe (Netherlands) £13.50 $36 A$38 €25.00 All correspondence concerning subscriptions should be addressed to Mr. D. Christian, 5, Roundwood Gardens, Harpenden, Herts. AL5 3AJ. Cheques should be made out to Gospel Standard Publications. For United States and Canada, please send to Mr. G. Tenbroeke, 1725 Plainwood Drive, Sheboygan, Wisconsin 53081, USA. Volume 140 January 2014 CONTENTS Our Monthly Message 3 Our Front Cover Picture 4 Good Wishes 5 For The Very Little Ones: Naomi Returns 6 Colouring Text: Ruth 1. 22. 7 Bible Lessons: The Burial Of Jesus 8 Three ‘B’s For 2014 10 A Dark Episode 12 Naaman 17 Sin 17 The Necessity Of Divine Life 18 Editor’s Postbag 18 Fascinating Flowerpots 19 Bible Study For The Older Ones: Light And Darkness (I) 20 Bible Questions: Washing And Making Clean 22 Poetry: A Conversation Between Two Brothers 24 Friendly Companion January 2014 3 OUR MONTHLY MESSAGE Dear Children and Young People, As you pick up the Friendly Companion this month it will be to read the first issue of another year. How quickly, to those of us who are older, do the years fly past! When you are younger, often time seems to drag, and there is a danger that you might wish your time away faster than God intends. -

An Interim Report on the Results of the Lairg Project 1988 - 1992 R.P.J
AN INTERIM REPORT ON THE RESULTS OF THE LAIRG PROJECT 1988 - 1992 R.P.J. McCullagh Abstract This paper reviews the archaeological fieldwork undertaken at Lairg, Sutherland from 1988 to 1991 and reports on the preliminary results ofpost-excavation analyses. This programme was established at the instigation of regional and national heritage agencies to advise on a route for a proposed upgraded road. Standard and innovatory techniques of archaeological excavation and survey were combined with various environmental approaches in an attempt to map the evolution of the present-day landscape. In particular, the project has sought to identify and analyse the crucial role of land-use in this evolution. Introduction The recent archaeological work at Lairg, in eastern Sutherland, took place within a corridor of land that straddles the A836. This corridor measures 2.2 miles (3.5km) by a maximum of 330yds (O.3km) and runs north from Achinduich farm to about 0.6 miles (lkm) south of the village of Lairg (Fig. 1). The then Highland Regional Roads Authority (HRRA) informed Historic Scotland and sought assistance in achieving a route that would cause the least damage to the archaeological remains in the corridor. The archaeological project that developed from this enquiry has been funded by Highland Regional Council and Historic Scotland. The fieldwork spanned four years: 1988 a topographic survey of upstanding monuments; 1989 a test-pit sampling programme; 1990 a short season of scientific sampling; 1990 an eight week season of excavations; 1991 a further eight week season of excavations. Further fieldwork directed towards the sampling needs of two associated research studentships (see below) has also been undertaken.