Use of Acetazolamide in Lithium-Induced Nephrogenic Diabetes Insipidus: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eslicarbazepine Acetate Longer Procedure No
European Medicines Agency London, 19 February 2009 Doc. Ref.: EMEA/135697/2009 CHMP ASSESSMENT REPORT FOR authorised Exalief International Nonproprietary Name: eslicarbazepine acetate longer Procedure No. EMEA/H/C/000987 no Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. product Medicinal 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1. Submission of the dossier ...................................................................................................... 3 1.2. Steps taken for the assessment of the product..................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1. Introduction............................................................................................................................ 4 2.2. Quality aspects ....................................................................................................................... 5 2.3. Non-clinical aspects................................................................................................................ 8 2.4. Clinical aspects.................................................................................................................... -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
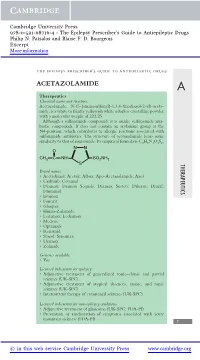
Acetazolamide
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. -

Topiramate Is More Effective Than Acetazolamide at Lowering
University of Birmingham Topiramate is more effective than acetazolamide at lowering intracranial pressure Scotton, William J; Botfield, Hannah F; Westgate, Connar Sj; Mitchell, James L; Yiangou, Andreas; Uldall, Maria S; Jensen, Rigmor H; Sinclair, Alex J DOI: 10.1177/0333102418776455 License: Creative Commons: Attribution (CC BY) Document Version Publisher's PDF, also known as Version of record Citation for published version (Harvard): Scotton, WJ, Botfield, HF, Westgate, CS, Mitchell, JL, Yiangou, A, Uldall, MS, Jensen, RH & Sinclair, AJ 2018, 'Topiramate is more effective than acetazolamide at lowering intracranial pressure', Cephalalgia. https://doi.org/10.1177/0333102418776455 Link to publication on Research at Birmingham portal Publisher Rights Statement: William J Scotton, Hannah F Botfield, Connar SJ Westgate, James L Mitchell, Andreas Yiangou, Maria S Uldall, Rigmor H Jensen, and Alex J Sinclair, Topiramate is more effective than acetazolamide at lowering intracranial pressure, Cephalalgia, First Published June 13, 2018; https://doi.org/10.1177/0333102418776455. Checked 02/07/2018. General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain. -

Approach to Managing Patients with Sulfa Allergy Use of Antibiotic and Nonantibiotic Sulfonamides
CME Approach to managing patients with sulfa allergy Use of antibiotic and nonantibiotic sulfonamides David Ponka, MD, CCFP(EM) ABSTRACT OBJECTIVE To present an approach to use of sulfonamide-based (sulfa) medications for patients with sulfa allergy and to explore whether sulfa medications are contraindicated for patients who require them but are allergic to them. SOURCES OF INFORMATION A search of current pharmacology textbooks and of MEDLINE from 1966 to the present using the MeSH key words “sulfonamide” and “drug sensitivity” revealed review articles, case reports, one observational study (level II evidence), and reports of consensus opinion (level III evidence). MAIN MESSAGE Cross-reactivity between sulfa antibiotics and nonantibiotics is rare, but on occasion it can affect the pharmacologic and clinical management of patients with sulfa allergy. CONCLUSION How a physician approaches using sulfa medications for patients with sulfa allergy depends on the certainty and severity of the initial allergy, on whether alternatives are available, and on whether the contemplated agent belongs to the same category of sulfa medications (ie, antibiotic or nonantibiotic) as the initial offending agent. RÉSUMÉ OBJECTIF Proposer une façon d’utiliser les médicaments à base de sulfamides (sulfas) chez les patients allergiques aux sulfas et vérifier si ces médicaments sont contre-indiqués pour ces patients. SOURCES DE L’INFORMATION Une consultation des récents ouvrages de pharmacologie et de MEDLINE entre 1966 et aujourd’hui à l’aide des mots clés MeSH «sulfonamide» et «drug sensitivity» a permis de repérer plusieurs articles de revue et études de cas, une étude d’observation et des rapports d’opinion consensuelles (preuves de niveau III). -

Diamox/Aldactone to Increase the Urinary Excretion of Sodium: an Investigational Study in Congestive Heart Failure
Official Title: Diamox/Aldactone to Increase the URinary Excretion of Sodium: an Investigational Study in Congestive Heart Failure NCT01973335 Date: August 27, 2015 DIURESIS-CHF – Study protocol version August 27, 2015 1 1. Background Aging of the population and prolongation of the lives of cardiac patients by modern therapeutic innovations have led to an increased incidence of congestive heart failure (CHF).1 During the last two decades, important progress has been made in the treatment of ambulatory CHF patients with reduced ejection fraction. Renin-angiotensin system blockers, β-blockers, mineralocorticoid receptor antagonists (MRA), ivabradine and cardiac resynchronization therapy have all demonstrated to reduce morbidity and/or mortality in ambulatory CHF patients.2-17 Despite these important advances, many patients are still hospitalized frequently with signs and symptoms of systemic congestion, which is associated with worse outcome.18 Treatment in these cases mainly focuses on symptomatic relief through administration of diuretics, although clear evidence on the optimal agent, dosing schedule, and administration route is lacking. Coexisting renal dysfunction often complicates decongestive treatment and worsening renal function (WRF), often defined as a 0.3 mg/dL rise in serum creatinine (Cr), is a common finding in this context.19 However, the prognostic impact of WRF, defined as Cr change is unsure as it might be associated with worse, neutral or even better outcome.20-22 In contrast, persistent congestion, as a reflection of the inability of the kidneys to preserve sodium homeostasis, has been more consistently associated with higher mortality and more frequent readmissions in CHF.23 This suggests that achieving a negative sodium balance might be an attractive treatment target in heart failure. -

Which Diuretics Are Safe and Effective for Patients with a Sulfa Allergy?
From the CLINIcAL InQUiRiES Family Physicians Inquiries Network Ron Healy, MD University of Washington, Which diuretics are safe Seattle; Alaska Family Medicine Residency, Anchorage and effective for patients Terry Ann Jankowski, MLS University of Washington, Seattle with a sulfa allergy? Evidence-based answer Diuretics that do not contain a sulfonamide subsequent allergic reactions to commonly group (eg, amiloride hydrochloride, used sulfonamide-containing diuretics eplerenone, ethacrynic acid, spironolactone, (eg, carbonic anhydrase inhibitors, loop and triamterene) are safe for patients with an diuretics, and thiazides) (strength of allergy to sulfa. The evidence is contradictory recommendation: C, based on case series ® as to whether a history Dowdenof allergy to Healthand poor Media quality case-control and cohort sulfonamide antibiotics increases the risk of studies). Copyright Clinical commentaryFor personal use only Are all sulfa drugs created equal? agents and off-patent, with no company Historical bromides commonly fall by the to take up their cause, no one has been FAST TRACK wayside as better evidence becomes willing to challenge outdated package Reasonable available. Who would have thought 15 insert warnings. years ago that we would be promoting As clinicians who regularly work evidence supports beta-blockers for patients with congestive without a net, we are accustomed to what many of us heart failure? prescribing medications in less than ideal are doing: Using Likewise, with closer inspection, we circumstances. Thankfully, reasonable cheap thiazides have learned that not all sulfa drugs are evidence is available to support what many created equal. The stereospecificity due of us are already doing—using cheap for patients to the absence of aromatic amines in thiazides for patients despite a history of with a history common diuretics means they are safe sulfa allergy. -

Using Medications, Cosmetics, Or Eating Certain Foods Can Increase Sensitivity to Ultraviolet Radiation
USING MEDICATIONS, COSMETICS, OR EATING CERTAIN FOODS CAN INCREASE SENSITIVITY TO ULTRAVIOLET RADIATION. INDIVIDUALS SHOULD CONSULT A PHYSICIAN BEFORE USING A SUNLAMP, IF THEY ARE TAKING MEDICATIONS. THE ITEMS LISTED ARE POTENTIAL PHOTOSENSITIZING AGENTS THAT MAY INCREASE SENSITIVITY TO ULTRAVIOLET LIGHT THAT MAY RESULT IN A PHOTOTOXIC OR PHOTOALLERGIC RESPONSES. PHOTOSENSITIZING MEDICATIONS Acetazolamide Amiloride+Hydrochlorothizide Amiodarone Amitriptyline Amoxapine Astemizole Atenolol+Chlorthalidone Auranofin Azatadine (Optimine) Azatidine+Pseudoephedrine Bendroflumethiazide Benzthiazide Bromodiphenhydramine Bromopheniramine Captopril Captopril+Hydrochlorothiazide Carbaamazepine Chlordiazepoxide+Amitriptyline Chlorothiazide Chlorpheniramine Chlorpheniramin+DPseudoephedrine Chlorpromazine Chlorpheniramine+Phenylopropanolamine Chlorpropamide Chlorprothixene Chlorthalidone Chlorthalidone+Reserpine Ciprofloxacin Clemastine Clofazime ClonidineChlorthalisone+Coal Tar Coal Tar Contraceptive (oral) Cyclobenzaprine Cyproheptadine Dacarcazine Danazol Demeclocycline Desipramine Dexchlorpheniramine Diclofenac Diflunisal Ditiazem Diphenhydramine Diphenylpyraline Doxepin Doxycycline Doxycycline Hyclate Enalapril Enalapril+Hydrochlorothiazide Erythromycin Ethylsuccinate+Sulfisoxazole Estrogens Estrogens Ethionamide Etretinate Floxuridine Flucytosine Fluorouracil Fluphenazine Flubiprofen Flutamide Gentamicin Glipizide Glyburide Gold Salts (compounds) Gold Sodium Thiomalate Griseofulvin Griseofulvin Ultramicrosize Griseofulvin+Hydrochlorothiazide Haloperidol -

Acetazolamide Attenuates Lithium-Induced Nephrogenic Diabetes Insipidus
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2016 Acetazolamide Attenuates Lithium-Induced Nephrogenic Diabetes Insipidus de Groot, Theun ; Sinke, Anne P ; Kortenoeven, Marleen L A ; Alsady, Mohammad ; Baumgarten, Ruben ; Devuyst, Olivier ; Loffing, Johannes ; Wetzels, Jack F ; Deen, Peter MT Abstract: To reduce lithium-induced nephrogenic diabetes insipidus (lithium-NDI), patients with bipo- lar disorder are treated with thiazide and amiloride, which are thought to induce antidiuresis by a compensatory increase in prourine uptake in proximal tubules. However, thiazides induced antidiure- sis and alkalinized the urine in lithium-NDI mice lacking the sodium-chloride cotransporter, suggesting that inhibition of carbonic anhydrases (CAs) confers the beneficial thiazide effect. Therefore, we tested the effect of the CA-specific blocker acetazolamide in lithium-NDI. In collecting duct (mpkCCD) cells, acetazolamide reduced the cellular lithium content and attenuated lithium-induced downregulation of aquaporin-2 through a mechanism different from that of amiloride. Treatment of lithium-NDI mice with acetazolamide or thiazide/amiloride induced similar antidiuresis and increased urine osmolality and aquaporin-2 abundance. Thiazide/amiloride-treated mice showed hyponatremia, hyperkalemia, hypercal- cemia, metabolic acidosis, and increased serum lithium concentrations, adverse effects previously observed in patients but not in acetazolamide-treated mice in this study. Furthermore, acetazolamide treatment reduced inulin clearance and cortical expression of sodium/hydrogen exchanger 3 and attenuated the increased expression of urinary PGE2 observed in lithium-NDI mice. These results show that the antid- iuresis with acetazolamide was partially caused by a tubular-glomerular feedback response and reduced GFR. -

Utah Medicaid Pharmacy & Therapeutics Committee
Utah Medicaid Pharmacy & Therapeutics Committee Drug Class Review: Older Anticonvulsants Barbiturates, Anticonvulsants 28:12.04 Primidone (Mysoline®) Hydantoins 28:12.12 Ethotoin (Peganone®) Phenytoin (Dilantin-125®, Dilantin®, Dilantin® Infatabs®, Dilantin® Kapseals®, Phenytek® and generics) Succinimides 28:12:20 Ethosuximide (Zarontin®, Zarontin® Syrup) Methsuximide (Celontin® Kapseals®) Anticonvulsants, Miscellaneous 28:12.92 Carbamazepine (Carbatrol®, Epitrol®, Tegretol®, Tegretol® XR) Valproate Sodium, Valproic Acid, Divalproex Sodium (Depacon®, Depakene®, Depakote®, Depakote® ER, Depakote® Sprinkle, Stavzor®) Anticonvulsants, Miscellaneous 28:12.92 and 54:40.12 Carbonic Anhydrase Inhibitor Acetazolamide (Diamox®) Barbiturates 28:24.04 Pentobarbital (Nembutal® Sodium Solution) Phenobarbital (Luminal® Sodium and generic) Final Report October 2016 Prepared by: Vicki Frydrych BS, PharmD, Clinical Pharmacist University of Utah College of Pharmacy Copyright © 2016 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved 1 Table of Contents Executive Summary ...................................................................................................................................................... 3 Introduction ................................................................................................................................................................... 8 Table 1: Product Comparison ................................................................................................................................ -

Evaluation of Adverse Events in Self-Reported Sulfa-Allergic Patients Using Topical Carbonic Anhydrase Inhibitors
JOURNAL OF OCULAR PHARMACOLOGY AND THERAPEUTICS Volume 29, Number 5, 2013 ª Mary Ann Liebert, Inc. DOI: 10.1089/jop.2012.0123 Evaluation of Adverse Events in Self-Reported Sulfa-Allergic Patients Using Topical Carbonic Anhydrase Inhibitors Guilherme B. Guedes,1 Abraar Karan,1 Hylton R. Mayer,2 and M. Bruce Shields1 Abstract Purpose: To investigate whether a self-reported history of allergy to sulfa-based drugs is a predictor for sub- sequent adverse reactions to topical carbonic anhydrase inhibitors (CAIs). Methods: A retrospective case-controlled cohort study via chart review was performed on 1,287 patients with a diagnosis of glaucoma. The outcome measure was the development of an adverse reaction (either ocular, systemic, or both) within at least 30 days after receipt of 1 of 4 classes of topical glaucoma medications: CAIs (dorzolamide and brinzolamide), prostaglandin analogues, beta-adrenergic blockers, and alpha2-adrenergic agonists. Results: Patients with a self-reported history of sulfa allergy had significantly more ocular adverse reactions after the initiation of any of the topical antiglaucoma medications when compared to those patients with no reported allergies. Patients with a self-reported sulfa allergy and patients who self-reported other, nonsulfa-related al- lergies had similar rates of adverse reactions to most of the topical medications. The patients reporting a sulfa allergy who used topical CAIs did not have more adverse reactions compared with patients who reported having other, nonsulfa-related allergies who used topical CAIs. Self-reported sulfa-allergic patients had similar rates of adverse reactions to topical CAIs compared with topical prostaglandin analogues. Conclusion: It may be safe to use a topical CAI in patients who report a history of a sulfa allergy. -

Ambetter 90-Day-Maintenance Drug List- 2020
Ambetter 90-Day-Maintenance Drug List Guide to this list: What is Ambetter 90‐Day‐Maintenance Drug List? Ambetter 90‐Day‐Supply Maintenance Drug List is a list of maintenance medications that are available for 90 day supply through mail order or through our Extended Day Supply Network. How do I find a pharmacy that is participating in Extended Day Supply Network? To find a retail pharmacy that is participating in our Extended Day Supply Network please consult information available under Pharmacy Resources tab on our webpage. Alternatively, you can utilize our mail order pharmacy. Information on mail order pharmacy is available in Pharmacy Resources tab on our webpage. Are all formulary drugs covered for 90 day supply? No, certain specialty and non‐specialty drugs are excluded from 90 day supply. Please consult 90‐Day‐ Supply Maintenance Drug List for information if your drug is included. A Amlodipine Besylate-Atorvastatin Calcium Acamprosate Calcium Amlodipine Besylate-Benazepril HCl Acarbose Amlodipine Besylate-Olmesartan Medoxomil Acebutolol HCl Amlodipine Besylate-Valsartan Acetazolamide Amlodipine-Valsartan-Hydrochlorothiazide Albuterol Sulfate Amoxapine Alendronate Sodium Amphetamine-Dextroamphetamine Alendronate Sodium-Cholecalciferol Anagrelide HCl Alfuzosin HCl Anastrozole Aliskiren Fumarate Apixaban Allopurinol Arformoterol Tartrate Alogliptin Benzoate Aripiprazole Alosetron HCl Armodafinil Amantadine HCl Asenapine Maleate Amiloride & Hydrochlorothiazide Aspirin-Dipyridamole Amiloride HCl Atenolol Amiodarone HCl Atenolol & Chlorthalidone