June 2017 Routine Pulse Oximetry Screening To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Evolution of Hospitals from Antiquity to the Renaissance
Acta Theologica Supplementum 7 2005 THE EVOLUTION OF HOSPITALS FROM ANTIQUITY TO THE RENAISSANCE ABSTRACT There is some evidence that a kind of hospital already existed towards the end of the 2nd millennium BC in ancient Mesopotamia. In India the monastic system created by the Buddhist religion led to institutionalised health care facilities as early as the 5th century BC, and with the spread of Buddhism to the east, nursing facilities, the nature and function of which are not known to us, also appeared in Sri Lanka, China and South East Asia. One would expect to find the origin of the hospital in the modern sense of the word in Greece, the birthplace of rational medicine in the 4th century BC, but the Hippocratic doctors paid house-calls, and the temples of Asclepius were vi- sited for incubation sleep and magico-religious treatment. In Roman times the military and slave hospitals were built for a specialised group and not for the public, and were therefore not precursors of the modern hospital. It is to the Christians that one must turn for the origin of the modern hospital. Hospices, originally called xenodochia, ini- tially built to shelter pilgrims and messengers between various bishops, were under Christian control developed into hospitals in the modern sense of the word. In Rome itself, the first hospital was built in the 4th century AD by a wealthy penitent widow, Fabiola. In the early Middle Ages (6th to 10th century), under the influence of the Be- nedictine Order, an infirmary became an established part of every monastery. -

The New York City Standards for Respectful Care at Birth (NYC Standards)
Implementation Toolkit Practice Guidance The New York City Standards for Respectful Care at Birth (NYC Standards) Purpose: This document is intended to support MCH professionals to implement a practice found in the Implementation Toolkits. This resource provides the information needed to replicate the practice and is divided into two sections: the first section provides a high-level overview of the practice while the second section describes how to implement the practice. For additional information on any of the content provided below, please reach out to the practice contact located at the bottom of this document. Section I: Resource Overview Practice Description The New York City Standards for Respectful Care at Birth (NYC Standards) were co-created by the Sexual and Reproductive Justice Community Engagement Group (SRJ-CEG) and the New York City Department of Health and Mental Hygiene (NYC DOHMH) to inform, educate and support pregnant, birthing, and parenting people with regard to their human rights, and encourage them to be active decision-makers in their healthcare experiences. The 29 NYC Standards are organized into 7 overarching categories: Education, Quality of Care, Informed Consent, Decision- Making, Dignity and Nondiscrimination and Support. In July 2015, the NYC DOHMH convened the SRJ-CEG in order to co-create respectful, equitable, culturally grounded, and community-driven means of promoting sexual and reproductive health and justice in NYC. Drafting, publishing and promoting the NYC Standards was one success of SRJ-CEG’s Birth Justice campaign, which aimed to 1) support community members and providers to advocate for respectful care at birth, 2) increase application of best practices for respectful care at birth within health care institutions, and 3) mobilizing stakeholders and changing institutional policies and practices to support the use of the sexual and reproductive justice framework and community-led initiatives and accountability. -

Health Care Facilities Hospitals Report on Training Visit
SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA FACULTY OF ARCHITECTURE INSTITUTE OF HOUSING AND CIVIC STRUCTURES HEALTH CARE FACILITIES HOSPITALS REPORT ON TRAINING VISIT In the frame work of the project No. SAMRS 2010/12/10 “Development of human resource capacity of Kabul polytechnic university” Funded by UÜtà|áÄtät ECDC cÜÉA Wtâw f{t{ YtÜâÖ December, 14, 2010 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 Acknowledgement: I Daud Shah Faruq professor of Kabul Poly Technic University The author of this article would like to express my appreciation for the Scientific Training Program to the Faculty of Architecture of the Slovak University of Technology and Slovak Aid program for financial support of this project. I would like to say my hearth thanks to Professor Arch. Mrs. Veronika Katradyova PhD, and professor Arch. Mr. stanislav majcher for their guidance and assistance during the all time of my training visit. My thank belongs also to Ing. Juma Haydary, PhD. the coordinator of the project SMARS/2010/10/01 in the frame work of which my visit was realized. Besides of this I would like to appreciate all professors and personnel of the faculty of Architecture for their good behaves and hospitality. Best regards cÜÉyA Wtâw ft{t{ YtÜâÖ December, 14, 2010 2 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 VISITING REPORT FROM FACULTY OF ARCHITECTURE OF SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA This visit was organized for exchanging knowledge views and advices between us (professor of Kabul Poly Technic University and professors of this faculty). My visit was especially organized to the departments of Public Buildings and Interior design. -

Table 3: 1960 - 2017 Historic Hospital List by CODE
Table 3: 1960 - 2017 Historic Hospital List by CODE County Code Hospital Name Address City Zip 1 001 ALAMEDA HOSPITAL 2070 CLINTON AVE ALAMEDA 94501 1 002 ALTA BATES HOSPITAL AT ALBANY 1247 MARIN AVENUE ALBANY 94706 1 003 ALTA BATES MEDICAL CENTER 2450 ASHBY AVENUE BERKELEY 94705 1 004 BOOTH MEMORIAL HOSPITAL 2794 GARDEN STREET OAKLAND 94701 1 005 CHILDREN'S HOSPITAL 51ST & GROVE STREETS OAKLAND 94609 1 006 CIVIC CENTER HOSPITAL FOUNDATION 390 40TH STREET OAKLAND 94609 1 007 SAN LEANDRO HOSPITAL 13855 E 14TH STREET SAN LEANDRO 94578 1 008 EDEN MEDICAL CENTER 20103 LAKE CHABOT RD CASTRO VALLEY 94546 1 009 ESKATON DOCTORS HOSPITAL OAKLAND 4600 E FAIRFAX AVENUE OAKLAND 94601 1 010 FAIRMONT HOSPITAL 15400 FOOTHILL BOULEVARD SAN LEANDRO 94578 1 011 HAYWARD HOSPITAL 770 'A' STREET HAYWARD 94541 1 012 HERRICK MEMORIAL HOSPITAL 2001 DWIGHT WAY BERKELEY 94704 1 013 ACMC-HIGHLAND CAMPUS 1411 E. 31ST ST OAKLAND 94602 1 014 KAISER HOSPITAL: SAN LEANDRO 2500 MERCED STREET SAN LEANDRO 94577 1 015 KAISER HOSPITAL: OAKLAND 275 W. MACARTHUR BLVD OAKLAND 94611 1 016 SUMMIT MEDICAL CENTER - HAWTHORNE 350 HAWTHORNE AVENUE OAKLAND 94609 1 017 NAVAL HOSPITAL: OAKLAND 8750 MOUNTAIN BOULEVARD OAKLAND 94627 1 018 OAKLAND HOSPITAL CORPORATION 2648 EAST 14TH STREET OAKLAND 94601 1 019 OGORMAN INFANT 2587 - 35TH AVENUE OAKLAND 94601 1 020 PERALTA HOSPITAL 450 - 30TH STREET OAKLAND 94609 1 021 SUMMIT MEDICAL CENTER 3100 SUMMIT STREET OAKLAND 94623 1 022 ST. ROSE HOSPITAL 27200 CALAROGA AVE HAYWARD 94540 1 023 ST. PAUL'S HOSPITAL 813 J STREET LIVERMORE 94550 1 024 VALLEYCARE MEDICAL CENTER 5555 W. -

Psychiatric Induced Births in Jamaica: Homicide and Death Effects On
rensic An o th F f ro o p l Bourne and Hudson-Davis, J Forensic Anthropol 2016, 1:1 o a l n o r g Journal of Forensic u y o J Anthropology Research Article Open Access Psychiatric Induced Births in Jamaica: Homicide and Death Effects on Pregnancy Paul Andrew Bourne1* and Angela Hudson-Davis2 1Director, Socio-Medical Research Institute, Kingston, Jamaica 2Angela Hudson-Davis, Capella University, USA Abstract For this paper, the researchers have narrowed the gap in the health literature by addressing the following objectives: 1) evaluate the role of homicide on admissions to a maternity hospital (or on pregnancy); 2) assess whether or not deaths can induce pregnancy or birth; 3) determine the responsivity of hospitalization at a mental health facility among pregnant women; and 4) calculated the responsivity of hospitalization to a maternity institution based on changes in homicide or deaths. The data for this study were taken from a Jamaica Government Publication. Data were also obtained from the Ministry of Health (2005-2015) on admissions to a national mental health public hospital in Jamaica, which is the Bellevue Hospital. The period for this work is from 2005 through to 2015. Homicide has an effect on admissions to Victoria Jubilee hospital, using the positive elasticities, especially those greater than one. Keywords: Induced birth; Postpartum psychosis engines did not turn up a single research on the aforementioned issues. Another rationale for this study is based on the comments of Valenca Introduction and de Moraes “There is a scarcity of studies in the literature that Jamaica is the largest English-Speaking Caribbean nation and deal with the relationship between mental disorders and homicide in the third largest Caribbean island with an estimated population of developing countries” (S67) [13]. -

Table 2: 1960 - 2017 Historic Hospital List by COUNTY
Table 2: 1960 - 2017 Historic Hospital List by COUNTY County Code Hospital Name/Address City Zip ALAMEDA 1 013 ACMC-HIGHLAND CAMPUS 1411 E. 31ST ST OAKLAND 94602 1 001 ALAMEDA HOSPITAL 2070 CLINTON AVE ALAMEDA 94501 1 002 ALTA BATES HOSPITAL AT ALBANY 1247 MARIN AVENUE ALBANY 94706 1 003 ALTA BATES MEDICAL CENTER 2450 ASHBY AVENUE BERKELEY 94705 1 004 BOOTH MEMORIAL HOSPITAL 2794 GARDEN STREET OAKLAND 94701 1 005 CHILDREN'S HOSPITAL 51ST & GROVE STREETS OAKLAND 94609 1 006 CIVIC CENTER HOSPITAL FOUNDATION 390 40TH STREET OAKLAND 94609 1 008 EDEN MEDICAL CENTER 20103 LAKE CHABOT RD CASTRO VALLEY 94546 1 009 ESKATON DOCTORS HOSPITAL OAKLAND 4600 E FAIRFAX AVENUE OAKLAND 94601 1 010 FAIRMONT HOSPITAL 15400 FOOTHILL BOULEVARD SAN LEANDRO 94578 1 011 HAYWARD HOSPITAL 770 'A' STREET HAYWARD 94541 1 012 HERRICK MEMORIAL HOSPITAL 2001 DWIGHT WAY BERKELEY 94704 1 015 KAISER HOSPITAL: OAKLAND 275 W. MACARTHUR BLVD OAKLAND 94611 1 014 KAISER HOSPITAL: SAN LEANDRO 2500 MERCED STREET SAN LEANDRO 94577 1 017 NAVAL HOSPITAL: OAKLAND 8750 MOUNTAIN BOULEVARD OAKLAND 94627 1 018 OAKLAND HOSPITAL CORPORATION 2648 EAST 14TH STREET OAKLAND 94601 1 019 OGORMAN INFANT 2587 - 35TH AVENUE OAKLAND 94601 1 020 PERALTA HOSPITAL 450 - 30TH STREET OAKLAND 94609 1 025 PHYSICIANS COMMUNITY HOSPITAL 2800 BENEDICT DRIVE SAN LEANDRO 94577 1 007 SAN LEANDRO HOSPITAL 13855 E 14TH STREET SAN LEANDRO 94578 1 023 ST. PAUL'S HOSPITAL 813 J STREET LIVERMORE 94550 1 022 ST. ROSE HOSPITAL 27200 CALAROGA AVE HAYWARD 94540 1 021 SUMMIT MEDICAL CENTER 3100 SUMMIT STREET OAKLAND 94623 1 016 SUMMIT MEDICAL CENTER - HAWTHORNE 350 HAWTHORNE AVENUE OAKLAND 94609 1 781 THE BIRTH HOME 4441 RAILROAD AVE PLEASANTON 94566 1 024 VALLEYCARE MEDICAL CENTER 5555 W. -
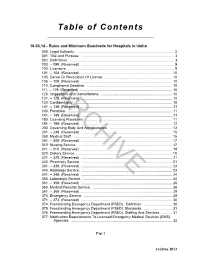
Rules and Minimum Standards for Hospitals in Idaho 000
Table of Contents 16.03.14 - Rules and Minimum Standards for Hospitals in Idaho 000. Legal Authority. ................................................................................................. 3 001. Title And Purpose. ............................................................................................ 3 002. Definitions. ........................................................................................................ 3 003. -- 099. (Reserved) ............................................................................................. 9 100. Licensure. ......................................................................................................... 9 101. -- 104. (Reserved) ........................................................................................... 10 105. Denial Or Revocation Of License. ................................................................... 10 106. -- 109. (Reserved) ........................................................................................... 10 110. Compliance Deadline. ..................................................................................... 10 111. -- 119. (Reserved) ............................................................................................ 10 120. Inspections And Consultations. ....................................................................... 10 121. -- 129.ARCHIVE (Reserved) ........................................................................................... 10 130. Confidentiality. ............................................................................................... -
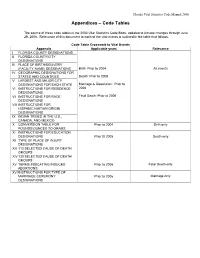
Appendices – Code Tables
Florida Vital Statistics Code Manual 2000 Appendices – Code Tables The source of these code tables is the 2003 Vital Statistics Code Book, updated to include changes through June 29, 2006. Relevance of this document to each of the vital events is outlined in the table that follows. Code Table Crosswalk to Vital Events Appendix Applicable years Relevance I FLORIDA COUNTY DESIGNATIONS II FLORIDA COUNTY/CITY DESIGNATIONS III PLACE OF BIRTH/DELIVERY (FACILITY NAME) DESIGNATIONS Birth: Prior to 2004 All events IV GEOGRAPHIC DESIGNATIONS FOR STATES AND COUNTRIES Death: Prior to 2005 V LARGEST AND MAJOR CITY DESIGNATIONS FOR EACH STATE Marriage & Dissolution: Prior to VI INSTRUCTIONS FOR RESIDENCE 2006 DESIGNATIONS VII INSTRUCTIONS FOR RACE Fetal Death: Prior to 2006 DESIGNATIONS VIII INSTRUCTIONS FOR HISPANIC/HAITIAN ORIGIN DESIGNATIONS IX INDIAN TRIBES IN THE U.S., CANADA, AND MEXICO X CONVERSION TABLE FOR Prior to 2004 Birth only POUNDS/OUNCES TO GRAMS XI INSTRUCTIONS FOR EDUCATION DESIGNATIONS Prior t0 2005 Death only XII TYPE OF PLACE OF INJURY DESIGNATIONS XIII 113 SELECTED CAUSE OF DEATH GROUPS XIV 130 SELECTED CAUSE OF DEATH GROUPS XV TERMS INDICATING INDUCED Prior to 2006 Fetal Death only ABORTIONS XVI INSTRUCTIONS FOR TYPE OF MARRIAGE CEREMONY Prior to 2006 Marriage only DESIGNATIONS FLORIDA VITAL STATISTICS APPENDICES - CODE TABLES APPENDIX I: FLORIDA COUNTY DESIGNATIONS COUNTY CODE COUNTY NAME COUNTY CODE COUNTY NAME 11 Alachua 45 Lake 12 Baker 46 Lee 13 Bay 47 Leon 14 Bradford 48 Levy 15 Brevard 49 Liberty 16 Broward 50 Madison 17 Calhoun 51 Manatee 18 Charlotte 52 Marion 19 Citrus 53 Martin 20 Clay 54 Monroe 21 Collier 55 Nassau 22 Columbia 56 Okaloosa 23 Miami-Dade 57 Okeechobee 24 Desoto 58 Orange 25 Dixie 59 Osceola 26 Duval 60 Palm Beach 27 Escambia 61 Pasco 28 Flagler 62 Pinellas 29 Franklin 63 Polk 30 Gadsden 64 Putnam 31 Gilchrist 65 St. -
What Is a Mother & Baby Unit (MBU)?
What is a Mother & Baby Unit (MBU)? What is a Mother & Baby Unit (MBU)? About this Leaflet: Disclaimer: This webpage provides information, not advice. You should read our full disclaimer before reading further. © October 2019 Health Service Executive (Ireland) & November 2018 Royal College of Psychiatrists. Note: there are no MBUs available in Ireland at present (2020). Planning for Irelands first MBU, to be located on St. Vincent’s Hospital Campus, Dublin is currently underway. This is in line with recommendations made in the Specialist Perinatal Mental Health Model of Care for Ireland. This leaflet outlines: • The important role the planned National Mother and Baby Unit will play in providing specialist care for women who require admission in an acute mental health unit during late pregnancy or within a year of giving birth. The leaflet covers: • What a Mother and Baby Unit is • When and why you might be referred to a Mother and Baby Unit • The professionals who work in a Mother and Baby Unit • The treatment and support available in a Mother and Baby Unit 2 © OCTOBER 2019 HEALTH SERVICE EXECUTIVE (IRELAND) & NOVEMBER 2018 ROYAL COLLEGE OF PSYCHIATRISTS. What is a Mother and Baby Unit (MBU)? It is a specialist in-patient unit for some women with mental health problems during pregnancy or after the birth of their child. If you have a more severe mental health problem, you might need to come into hospital. This should be a specialist psychiatric Mother and Baby Unit (MBU) where you, and your baby, can be admitted together. However, there are no MBUs available in Ireland at present though the development of an MBU is underway, so currently women are admitted to a general acute mental health unit. -

Obstetric Aspects of the Early Discharge of Maternity Patients
520 26 August 1967 Discharge of Maternity Patients-Arthurton and Bamford MBJ2RRL early discharge, and long-stay hospital patients is recorded; REFERENCES it has shown that mothers confined in hospital begin to feed Brit. med. ,, 1964, 2, 70. their babies and become established breast-feeders more often College of General Practitioners, Bradford Group (1966). Lancet, 1, Br Med J: first published as 10.1136/bmj.3.5564.520 on 26 August 1967. Downloaded from than do women delivered at home. 536. Craig, G. A., and Muirhead, J. M. B. (1967). Brit. med. 7., 3, 520. Douglas, J., Edgar, W., and Home, K. (1961). Med. Offr, 106, 333. We wish to thank Dr. A. P. Roberts for permission to review Hellman, L. MA, Kohl, S. G., and Palmer, J. (1962). Lancet, 1, 227. cases in his care; Miss G. Clayton, Matron of St. Luke's Maternity Ministry of Health (1958). Repon of the Matertity Services Committee Hospital, and Miss E. R. Entwhistle, Supervisor of Midwives, for (Cranbrook Report). H.M.S.O., London. their invaluable help on numerous occasions; and Dr. G. Hill for Pinker, G. D., and Fraser, A. C. (1964). Brit. med. 7., 2, 99. statistical advice. We wish to pay tribute to a very loyal junior Theobald, G. W. (1959). Ibid., 2, 1364. staff. - (1962). Lancet, 1, 735. Obstetric Aspects of the Early Discharge of Maternity Patients G. A. CRAIG,* M.B.E., F.R.C.S., F.R.C.O.G.; J. M. B. MUIRHEAD,* M.B., B.CH., M.R.C.O.G. Brit. med. J., 1967, 3, 520-522 It is now nine years since planned early discharge of the normal women in each parity group is shown in Table II. -

QTD 050426 West Anaheim Medical Center.Xlsx
Quality Transparency Dashboard Sepsis 30-day Outcome Measures: CLABSI Colon SSI NTSV Mortality Readmission West Anaheim Medical Center 2.64 0.00 Not Available 13.66 14.40 California Level 0.67 0.86 22.90 14.30 15.48 National Level 0.69 0.87 25.60 25.00 15.60 Measure Period 01/01/2019-12/31/2019 01/01/2019-12/31/2019 01/01/2019-12/31/2019 01/01/2019-12/31/2019 07/01/2018-06/30/2019 Notes : "Not Available" indicates that not enough data were available to calcualte the measure. For CLABSI and Colon SSI this usually means the expected number of infections was less than 1.0. For NTSV, Sepsis Mortality, and Readmission this means the number of eligible cases was less than 1.0. Program Status Measures: This hospital has a Maternity Safety Program in place. A maternity safety program provides a coordinated approach and emergency Yes No Not a maternity hospital response to risks associated with pregnancy and childbirth. This hospital has a Sepsis Protocol in place. A sepsis protocol provides guidance for a coordinated approach to identification and treatment of an Yes No infection and inflammatory response which is present throughout the body. This hospital has a Respiratory Monitoring program in place. Respiratory monitoring provides guidance for assessment of risk of respiratory Yes No depression, and includes continuous monitoring of breathing and functioning of the lungs and circulatory system when indicated. Outcome Measure Definitions: CLABSI - Central line-Associated Blood Stream Infection: A serious infection that occurs when germs enter the bloodstream through a central line. -

The Maternity Hospital Law and Requirements for Licensure for Maternity Hospitals Maternity Divisions in General Hospitals and Maternity Homes
THE MATERNITY HOSPITAL LAW AND REQUIREMENTS FOR LICENSURE FOR MATERNITY HOSPITALS MATERNITY DIVISIONS IN GENERAL HOSPITALS AND MATERNITY HOMES STATE OF ILLINOIS HENRY HORNER, Governor THE DEPARTMENT OF PUBLIC HEALTH January I, 1940 TABLE OF CONTENTS Page 3. Maternity Hospital Law 5 2. General Requirements 7 3. Maternity Home Requirements 11 4. Minimum Equipment 14 5. The Ophthalmia Law 16 6. The Prenatal Bloodtest Law 18 7. Sanitary Regulations 19 8. Index 29 STATE OF ILLINOIS nmm HOm ER. Governor THE DEPARTMENT OF PUBLIC HEALTH MATERNITY HOSPITAL LAW An Act for the licensing, inspection and regulation of maternity hospitals, lying-in homes, or other places, public or private, for the confinement of women and to provide a penalty for violation thereof. Approved June 24, in force July 1, 1915. Section 1. All persons, societies, associations, organizations or corporations desirous of conducting, maintaining or carrying on any maternity or lying-in hospital or other place, public or private, where females may be received, cared for or treated during pregnancy or during or after delivery, whether they are now existing and licensed by the State Department of Public Welfare or not, shall apply for and obtain a license therefor from the State Department of Public Health. Applications shall be made upon the blanks prescribed by said depart- ment, and shall be endorsed by six or more persons of good moral character who are regular taxpayers of the county where such mater- nity or lying-in hospital is located and who shall certify to the re- spectability of the applicant. If, in the opinion of said department, such hospital possesses the equipment necessary for its purpose, the conditions of the hospital are safe and sanitary, and the persons con- nected therewith are proper and suitable persons to conduct such hospital, then a license shall be issued.