Emerging Roles of Metallothioneins in Beta Cell Pathophysiology: Beyond and Above Metal Homeostasis and Antioxidant Response
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metallothionein Monoclonal Antibody, Clone N11-G
Metallothionein monoclonal antibody, clone N11-G Catalog # : MAB9787 規格 : [ 50 uL ] List All Specification Application Image Product Rabbit monoclonal antibody raised against synthetic peptide of MT1A, Western Blot (Recombinant protein) Description: MT1B, MT1E, MT1F, MT1G, MT1H, MT1IP, MT1L, MT1M, MT2A. Immunogen: A synthetic peptide corresponding to N-terminus of human MT1A, MT1B, MT1E, MT1F, MT1G, MT1H, MT1IP, MT1L, MT1M, MT2A. Host: Rabbit enlarge Reactivity: Human, Mouse Immunoprecipitation Form: Liquid Enzyme-linked Immunoabsorbent Assay Recommend Western Blot (1:1000) Usage: ELISA (1:5000-1:10000) The optimal working dilution should be determined by the end user. Storage Buffer: In 20 mM Tris-HCl, pH 8.0 (10 mg/mL BSA, 0.05% sodium azide) Storage Store at -20°C. Instruction: Note: This product contains sodium azide: a POISONOUS AND HAZARDOUS SUBSTANCE which should be handled by trained staff only. Datasheet: Download Applications Western Blot (Recombinant protein) Western blot analysis of recombinant Metallothionein protein with Metallothionein monoclonal antibody, clone N11-G (Cat # MAB9787). Lane 1: 1 ug. Lane 2: 3 ug. Lane 3: 5 ug. Immunoprecipitation Enzyme-linked Immunoabsorbent Assay ASSP5 MT1A MT1B MT1E MT1F MT1G MT1H MT1M MT1L MT1IP Page 1 of 5 2021/6/2 Gene Information Entrez GeneID: 4489 Protein P04731 (Gene ID : 4489);P07438 (Gene ID : 4490);P04732 (Gene ID : Accession#: 4493);P04733 (Gene ID : 4494);P13640 (Gene ID : 4495);P80294 (Gene ID : 4496);P80295 (Gene ID : 4496);Q8N339 (Gene ID : 4499);Q86YX0 (Gene ID : 4490);Q86YX5 -

CD56+ T-Cells in Relation to Cytomegalovirus in Healthy Subjects and Kidney Transplant Patients
CD56+ T-cells in Relation to Cytomegalovirus in Healthy Subjects and Kidney Transplant Patients Institute of Infection and Global Health Department of Clinical Infection, Microbiology and Immunology Thesis submitted in accordance with the requirements of the University of Liverpool for the degree of Doctor in Philosophy by Mazen Mohammed Almehmadi December 2014 - 1 - Abstract Human T cells expressing CD56 are capable of tumour cell lysis following activation with interleukin-2 but their role in viral immunity has been less well studied. The work described in this thesis aimed to investigate CD56+ T-cells in relation to cytomegalovirus infection in healthy subjects and kidney transplant patients (KTPs). Proportions of CD56+ T cells were found to be highly significantly increased in healthy cytomegalovirus-seropositive (CMV+) compared to cytomegalovirus-seronegative (CMV-) subjects (8.38% ± 0.33 versus 3.29%± 0.33; P < 0.0001). In donor CMV-/recipient CMV- (D-/R-)- KTPs levels of CD56+ T cells were 1.9% ±0.35 versus 5.42% ±1.01 in D+/R- patients and 5.11% ±0.69 in R+ patients (P 0.0247 and < 0.0001 respectively). CD56+ T cells in both healthy CMV+ subjects and KTPs expressed markers of effector memory- RA T-cells (TEMRA) while in healthy CMV- subjects and D-/R- KTPs the phenotype was predominantly that of naïve T-cells. Other surface markers, CD8, CD4, CD58, CD57, CD94 and NKG2C were expressed by a significantly higher proportion of CD56+ T-cells in healthy CMV+ than CMV- subjects. Functional studies showed levels of pro-inflammatory cytokines IFN-γ and TNF-α, as well as granzyme B and CD107a were significantly higher in CD56+ T-cells from CMV+ than CMV- subjects following stimulation with CMV antigens. -

Investigation of Structural Properties of Methylated Human Promoter Regions in Terms of Dna Helical Rise
INVESTIGATION OF STRUCTURAL PROPERTIES OF METHYLATED HUMAN PROMOTER REGIONS IN TERMS OF DNA HELICAL RISE A THESIS SUBMITTED TO THE GRADUATE SCHOOL OF INFORMATICS OF MIDDLE EAST TECHNICAL UNIVERSITY BY BURCU YALDIZ IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN BIOINFORMATICS AUGUST 2014 INVESTIGATION OF STRUCTURAL PROPERTIES OF METHYLATED HUMAN PROMOTER REGIONS IN TERMS OF DNA HELICAL RISE submitted by Burcu YALDIZ in partial fulfillment of the requirements for the degree of Master of Science, Bioinformatics Program, Middle East Technical University by, Prof. Dr. Nazife Baykal _____________________ Director, Informatics Institute Assist. Prof. Dr. Yeşim Aydın Son _____________________ Head of Department, Health Informatics, METU Assist. Prof. Dr. Yeşim Aydın Son Supervisor, Health Informatics, METU _____________________ Examining Committee Members: Assoc. Prof. Dr. Tolga Can _____________________ METU, CENG Assist. Prof. Dr. Yeşim Aydın Son _____________________ METU, Health Informatics Assist. Prof. Dr. Aybar Can Acar _____________________ METU, Health Informatics Assist. Prof. Dr. Özlen Konu _____________________ Bilkent University, Molecular Biology and Genetics Assoc. Prof. Dr. Çağdaş D. Son _____________________ METU, Biology Date: 27.08.2014 I hereby declare that all information in this document has been obtained and presented in accordance with academic rules and ethical conduct. I also declare that, as required by these rules and conduct, I have fully cited and referenced all material and results that are not original to this work. Name, Last name : Burcu Yaldız Signature : iii ABSTRACT INVESTIGATION OF STRUCTURAL PROPERTIES OF METHYLATED HUMAN PROMOTER REGIONS IN TERMS OF DNA HELICAL RISE Yaldız, Burcu M.Sc. Bioinformatics Program Advisor: Assist. Prof. Dr. Yeşim Aydın Son August 2014, 60 pages The infamous double helix structure of DNA was assumed to be a rigid, uniformly observed structure throughout the genomic DNA. -

Identification of 10 Hub Genes Related to the Progression of Colorectal
Identification of 10 Hub genes related to the progression of colorectal cancer by co-expression analysis Jie Meng1,2, Rui Su2, Yun Liao2, Yanyan Li2 and Ling Li2 1 Department of Pharmacy, Anhui University of Chinese Medicine, Hefei, China 2 Department of Pharmacy, Tongren Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China ABSTRACT Background: Colorectal cancer (CRC) is the third most common cancer in the world. The present study is aimed at identifying hub genes associated with the progression of CRC. Method: The data of the patients with CRC were obtained from the Gene Expression Omnibus (GEO) database and assessed by weighted gene co-expression network analysis (WGCNA), Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses performed in R by WGCNA, several hub genes that regulate the mechanism of tumorigenesis in CRC were identified. Differentially expressed genes in the data sets GSE28000 and GSE42284 were used to construct a co-expression network for WGCNA. The yellow, black and blue modules associated with CRC level were filtered. Combining the co-expression network and the PPI network, 15 candidate hub genes were screened. Results: After validation using the TCGA-COAD dataset, a total of 10 hub genes (MT1X, MT1G, MT2A, CXCL8, IL1B, CXCL5, CXCL11, IL10RA, GZMB, KIT) closely related to the progression of CRC were identified. The expressions of MT1G, CXCL8, IL1B, CXCL5, CXCL11 and GZMB in CRC tissues were higher than normal tissues (p-value < 0.05). The expressions of MT1X, MT2A, IL10RA and KIT in CRC tissues were lower than normal tissues (p-value < 0.05). -
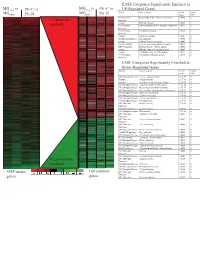
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Role of Phytochemicals in Colon Cancer Prevention: a Nutrigenomics Approach
Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan J van Erk Promotor: Prof. Dr. P.J. van Bladeren Hoogleraar in de Toxicokinetiek en Biotransformatie Wageningen Universiteit Co-promotoren: Dr. Ir. J.M.M.J.G. Aarts Universitair Docent, Sectie Toxicologie Wageningen Universiteit Dr. Ir. B. van Ommen Senior Research Fellow Nutritional Systems Biology TNO Voeding, Zeist Promotiecommissie: Prof. Dr. P. Dolara University of Florence, Italy Prof. Dr. J.A.M. Leunissen Wageningen Universiteit Prof. Dr. J.C. Mathers University of Newcastle, United Kingdom Prof. Dr. M. Müller Wageningen Universiteit Dit onderzoek is uitgevoerd binnen de onderzoekschool VLAG Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan Jolanda van Erk Proefschrift ter verkrijging van graad van doctor op gezag van de rector magnificus van Wageningen Universiteit, Prof.Dr.Ir. L. Speelman, in het openbaar te verdedigen op vrijdag 1 oktober 2004 des namiddags te vier uur in de Aula Title Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Author Marjan Jolanda van Erk Thesis Wageningen University, Wageningen, the Netherlands (2004) with abstract, with references, with summary in Dutch ISBN 90-8504-085-X ABSTRACT Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Specific food compounds, especially from fruits and vegetables, may protect against development of colon cancer. In this thesis effects and mechanisms of various phytochemicals in relation to colon cancer prevention were studied through application of large-scale gene expression profiling. Expression measurement of thousands of genes can yield a more complete and in-depth insight into the mode of action of the compounds. -

WO 2014/135655 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/135655 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12Q 1/68 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/EP2014/054384 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 6 March 2014 (06.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13305253.0 6 March 2013 (06.03.2013) EP (84) Designated States (unless otherwise indicated, for every (71) Applicants: INSTITUT CURIE [FR/FR]; 26 rue d'Ulm, kind of regional protection available): ARIPO (BW, GH, F-75248 Paris cedex 05 (FR). CENTRE NATIONAL DE GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, LA RECHERCHE SCIENTIFIQUE [FR/FR]; 3 rue UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, Michel Ange, F-75016 Paris (FR). -

Investigation of the Underlying Hub Genes and Molexular Pathogensis in Gastric Cancer by Integrated Bioinformatic Analyses
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Investigation of the underlying hub genes and molexular pathogensis in gastric cancer by integrated bioinformatic analyses Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karanataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract The high mortality rate of gastric cancer (GC) is in part due to the absence of initial disclosure of its biomarkers. The recognition of important genes associated in GC is therefore recommended to advance clinical prognosis, diagnosis and and treatment outcomes. The current investigation used the microarray dataset GSE113255 RNA seq data from the Gene Expression Omnibus database to diagnose differentially expressed genes (DEGs). Pathway and gene ontology enrichment analyses were performed, and a proteinprotein interaction network, modules, target genes - miRNA regulatory network and target genes - TF regulatory network were constructed and analyzed. Finally, validation of hub genes was performed. The 1008 DEGs identified consisted of 505 up regulated genes and 503 down regulated genes. -

A Comparative Genomic Study in Schizophrenic and in Bipolar Disorder Patients, Based on Microarray Expression Pro�Ling Meta�Analysis
Hindawi Publishing Corporation e Scienti�c �orld �ournal Volume 2013, Article ID 685917, 14 pages http://dx.doi.org/10.1155/2013/685917 Research Article A Comparative Genomic Study in Schizophrenic and in Bipolar Disorder Patients, Based on Microarray Expression Pro�ling Meta�Analysis Marianthi Logotheti,1, 2, 3 Olga Papadodima,2 Nikolaos Venizelos,1 Aristotelis Chatziioannou,2 and Fragiskos Kolisis3 1 Neuropsychiatric Research Laboratory, Department of Clinical Medicine, Örebro University, 701 82 Örebro, Sweden 2 Metabolic Engineering and Bioinformatics Program, Institute of Biology, Medicinal Chemistry and Biotechnology, National Hellenic Research Foundation, 48 Vassileos Constantinou Avenue, 11635 Athens, Greece 3 Laboratory of Biotechnology, School of Chemical Engineering, National Technical University of Athens, 15780 Athens, Greece Correspondence should be addressed to Aristotelis Chatziioannou; [email protected] and Fragiskos Kolisis; [email protected] Received 2 November 2012; Accepted 27 November 2012 Academic Editors: N. S. T. Hirata, M. A. Kon, and K. Najarian Copyright © 2013 Marianthi Logotheti et al. is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Schizophrenia affecting almost 1 and bipolar disorder affecting almost 3 –5 of the global population constitute two severe mental disorders. e catecholaminergic and the serotonergic pathways have been proved to play an important role in the development of schizophrenia, bipolar% disorder, and other related psychiatric% disorders.% e aim of the study was to perform and interpret the results of a comparative genomic pro�ling study in schizophrenic patients as well as in healthy controls and in patients with bipolar disorder and try to relate and integrate our results with an aberrant amino acid transport through cell membranes. -
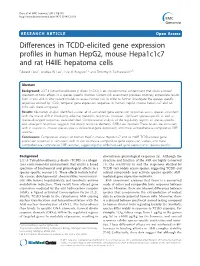
Differences in TCDD-Elicited Gene Expression Profiles in Human
Dere et al. BMC Genomics 2011, 12:193 http://www.biomedcentral.com/1471-2164/12/193 RESEARCHARTICLE Open Access Differences in TCDD-elicited gene expression profiles in human HepG2, mouse Hepa1c1c7 and rat H4IIE hepatoma cells Edward Dere1, Andrea W Lee1, Lyle D Burgoon1,2 and Timothy R Zacharewski1,2* Abstract Background: 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) is an environmental contaminant that elicits a broad spectrum of toxic effects in a species-specific manner. Current risk assessment practices routinely extrapolate results from in vivo and in vitro rodent models to assess human risk. In order to further investigate the species-specific responses elicited by TCDD, temporal gene expression responses in human HepG2, mouse Hepa1c1c7 and rat H4IIE cells were compared. Results: Microarray analysis identified a core set of conserved gene expression responses across species consistent with the role of AhR in mediating adaptive metabolic responses. However, significant species-specific as well as species-divergent responses were identified. Computational analysis of the regulatory regions of species-specific and -divergent responses suggests that dioxin response elements (DREs) are involved. These results are consistent with in vivo rat vs. mouse species-specific differential gene expression, and more comprehensive comparative DRE searches. Conclusions: Comparative analysis of human HepG2, mouse Hepa1c1c7 and rat H4IIE TCDD-elicited gene expression responses is consistent with in vivo rat-mouse comparative gene expression studies, and more comprehensive comparative DRE searches, suggesting that AhR-mediated gene expression is species-specific. Background downstream physiological responses [3]. Although the 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) is a ubiqui- structure and function of the AhR are highly conserved tous environmental contaminant that elicits a broad [4], the sensitivity to and the responses elicited by spectrum of biochemical and physiological effects in a TCDD vary widely across species, suggesting TCDD and species-specific manner [1]. -

Molecular Signatures of Maturing Dendritic Cells
Jin et al. Journal of Translational Medicine 2010, 8:4 http://www.translational-medicine.com/content/8/1/4 RESEARCH Open Access Molecular signatures of maturing dendritic cells: implications for testing the quality of dendritic cell therapies Ping Jin1*†, Tae Hee Han1,2†, Jiaqiang Ren1, Stefanie Saunders1, Ena Wang1, Francesco M Marincola1, David F Stroncek1 Abstract Background: Dendritic cells (DCs) are often produced by granulocyte-macrophage colony-stimulating factor (GM- CSF) and interleukin-4 (IL-4) stimulation of monocytes. To improve the effectiveness of DC adoptive immune cancer therapy, many different agents have been used to mature DCs. We analyzed the kinetics of DC maturation by lipopolysaccharide (LPS) and interferon-g (IFN-g) induction in order to characterize the usefulness of mature DCs (mDCs) for immune therapy and to identify biomarkers for assessing the quality of mDCs. Methods: Peripheral blood mononuclear cells were collected from 6 healthy subjects by apheresis, monocytes were isolated by elutriation, and immature DCs (iDCs) were produced by 3 days of culture with GM-CSF and IL-4. The iDCs were sampled after 4, 8 and 24 hours in culture with LPS and IFN-g and were then assessed by flow cytometry, ELISA, and global gene and microRNA (miRNA) expression analysis. Results: After 24 hours of LPS and IFN-g stimulation, DC surface expression of CD80, CD83, CD86, and HLA Class II antigens were up-regulated. Th1 attractant genes such as CXCL9, CXCL10, CXCL11 and CCL5 were up-regulated during maturation but not Treg attractants such as CCL22 and CXCL12. The expression of classical mDC biomarker genes CD83, CCR7, CCL5, CCL8, SOD2, MT2A, OASL, GBP1 and HES4 were up-regulated throughout maturation while MTIB, MTIE, MTIG, MTIH, GADD45A and LAMP3 were only up-regulated late in maturation. -

WO 2012/174282 A2 20 December 2012 (20.12.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/174282 A2 20 December 2012 (20.12.2012) P O P C T (51) International Patent Classification: David [US/US]; 13539 N . 95th Way, Scottsdale, AZ C12Q 1/68 (2006.01) 85260 (US). (21) International Application Number: (74) Agent: AKHAVAN, Ramin; Caris Science, Inc., 6655 N . PCT/US20 12/0425 19 Macarthur Blvd., Irving, TX 75039 (US). (22) International Filing Date: (81) Designated States (unless otherwise indicated, for every 14 June 2012 (14.06.2012) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, English (25) Filing Language: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, Publication Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (30) Priority Data: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 61/497,895 16 June 201 1 (16.06.201 1) US MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 61/499,138 20 June 201 1 (20.06.201 1) US OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, 61/501,680 27 June 201 1 (27.06.201 1) u s SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, 61/506,019 8 July 201 1(08.07.201 1) u s TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW.