Canadian Product Monograph
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Page 1 Note: Within Nine Months from the Publication of the Mention
Europäisches Patentamt (19) European Patent Office & Office européen des brevets (11) EP 1 411 992 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 49/04 (2006.01) A61K 49/18 (2006.01) 13.12.2006 Bulletin 2006/50 (86) International application number: (21) Application number: 02758379.8 PCT/EP2002/008183 (22) Date of filing: 23.07.2002 (87) International publication number: WO 2003/013616 (20.02.2003 Gazette 2003/08) (54) IONIC AND NON-IONIC RADIOGRAPHIC CONTRAST AGENTS FOR USE IN COMBINED X-RAY AND NUCLEAR MAGNETIC RESONANCE DIAGNOSTICS IONISCHES UND NICHT-IONISCHES RADIOGRAPHISCHES KONTRASTMITTEL ZUR VERWENDUNG IN DER KOMBINIERTEN ROENTGEN- UND KERNSPINTOMOGRAPHIEDIAGNOSTIK SUBSTANCES IONIQUES ET NON-IONIQUES DE CONTRASTE RADIOGRAPHIQUE UTILISEES POUR ETABLIR DES DIAGNOSTICS FAISANT APPEL AUX RAYONS X ET A L’IMAGERIE PAR RESONANCE MAGNETIQUE (84) Designated Contracting States: (74) Representative: Minoja, Fabrizio AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Bianchetti Bracco Minoja S.r.l. IE IT LI LU MC NL PT SE SK TR Via Plinio, 63 20129 Milano (IT) (30) Priority: 03.08.2001 IT MI20011706 (56) References cited: (43) Date of publication of application: EP-A- 0 759 785 WO-A-00/75141 28.04.2004 Bulletin 2004/18 US-A- 5 648 536 (73) Proprietor: BRACCO IMAGING S.p.A. • K HERGAN, W. DORINGER, M. LÄNGLE W.OSER: 20134 Milano (IT) "Effects of iodinated contrast agents in MR imaging" EUROPEAN JOURNAL OF (72) Inventors: RADIOLOGY, vol. 21, 1995, pages 11-17, • AIME, Silvio XP002227102 20134 Milano (IT) • K.M. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -
ACR Manual on Contrast Media – Version 9, 2013 Table of Contents / I
ACR Manual on Contrast Media Version 9 2013 ACR Committee on Drugs and Contrast Media ACR Manual on Contrast Media – Version 9, 2013 Table of Contents / i ACR Manual on Contrast Media Version 9 2013 ACR Committee on Drugs and Contrast Media © Copyright 2013 American College of Radiology ISBN: 978-1-55903-012-0 Table of Contents Topic Last Updated Page 1. Preface. V9 – 2013 . 3 2. Introduction . V7 – 2010 . 4 3. Patient Selection And Preparation Strategies . V7 – 2010 . 5 4. Injection of Contrast Media . V7 – 2010 . 13 5. Extravasation Of Contrast Media . V7 – 2010 . 17 6. Allergic-Like And Physiologic Reactions To Intravascular Iodinated Contrast Media . V9 – 2013 . 21 7. Contrast Media Warming . V8 – 2012 . 29 8. Contrast-Induced Nephrotoxicity . V8 – 2012 . 33 9. Metformin . V7 – 2010 . 43 10. Contrast Media In Children . V7 – 2010 . 47 11. Gastrointestinal (GI) Contrast Media In Adults: Indications And Guidelines V9 – 2013 . 55 12. Adverse Reactions To Gadolinium-Based Contrast Media . V7 – 2010 . 77 13. Nephrogenic Systemic Fibrosis . V8 – 2012 . 81 14. Treatment Of Contrast Reactions . V9 – 2013 . 91 15. Administration Of Contrast Media To Pregnant Or Potentially Pregnant Patients . V9 – 2013 . 93 16. Administration Of Contrast Media To Women Who Are Breast-Feeding . V9 – 2013 . 97 Table 1 – Indications for Use of Iodinated Contrast Media . V9 – 2013 . 99 Table 2 – Organ and System-Specific Adverse Effects from the Administration of Iodine-Based or Gadolinium-Based Contrast Agents. V9 – 2013 . 100 Table 3 – Categories of Acute Reactions . V9 – 2013 . 101 Table 4 – Treatment of Acute Reactions to Contrast Media in Children . V9 – 2013 . -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

OPTIRAY® Ioversol Injection
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION OPTIRAY® Ioversol Injection OPTIRAY® 240 Ioversol Injection 51% w/v, 240 mgI/mL OPTIRAY® 300 Ioversol Injection 64% w/v, 300 mgI/mL OPTIRAY® 320 Ioversol Injection 68% w/v, 320 mgI/mL OPTIRAY® 350 Ioversol Injection 74% w/v, 350 mgI/mL Nonionic Iodinated Radiographic Contrast Medium Liebel-Flarsheim Canada Inc. 7500 Trans-Canada Highway Date of Revision: Pointe-Claire, QC, H9R 5H8 November 1, 2017 CANADA Submission Control No: 203281 Page 1 of 55 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................4 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ..................................................................................................13 DRUG INTERACTIONS ..................................................................................................19 DOSAGE AND ADMINISTRATION ..............................................................................19 OVERDOSAGE ................................................................................................................33 ACTION AND CLINICAL PHARMACOLOGY -

Hepatic CT Enhancement: Comparison Between Dimeric And
J Korean Radiol Soc 2003;48:479-483 Hepatic CT Enhancement: Comparison between Dimeric and Monomeric Nonionic Contrast Agents in Rabbits1 Gi Hyeon Kim, M.D., Byung Kook Kwak, M.D., Hyung Jin Shim, M.D., Kyo Nam Kim, M.D.2, Wei Chiang Liu, M.D.3, Seung Hoon Ryu, M.D., Yang Soo Kim, M.D., Jong Beum Lee, M.D., Kun Sang Kim, M.D. Purpose: To determine the hepatic and vascular enhancement profiles with nonionic dimeric, iodixanol, contrast agent in the rabbit and to compare them with nonionic monomeric, ioversol, contrast agent. Materials and Methods: Seven rabbits initially underwent hepatic dynamic CT scan with either iodixanol or ioversol, followed by repeated CT scan with other unused con- trast agent with one week interval between scans. Pre and post contrast attenuation values of hepatic parenchyma, aorta and portal vein were measured sequentially. The mean enhancement of the hepatic parenchyma, aorta and portal vein were compared between two agents. The mean peak enhancement and peak enhancement time of the liver, aorta, and portal vein were also compared. Results: The attenuation values of ioversol showed a greater mean hepatic enhance- ment than iodixanol from 18 seconds to 39 seconds after injection (from late arterial phase to early portal venous phase) with a statistical significance (p<0.05). The mean peak enhancement of hepatic parenchyma, aorta and portal vein was also greater us- ing ioversol than iodixanol, but the mean peak enhancement times of ioversol and iodixanol were nearly identical. Conclusion: Ioversol may have the greater effects than iodixanol on hepatic tumor conspicuity, especially from late arterial phase to early portal veneous phase. -

Injection of Contrast Media V7 – 2010 13 5
ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media © Copyright 2012 American College of Radiology ISBN: 978-1-55903-009-0 Table of Contents Topic Last Updated Page 1. Preface. V8 – 2012 . 3 2. Introduction . V7 – 2010 . 4 3. Patient Selection and Preparation Strategies . V7 – 2010 . 5 4. Injection of Contrast Media . V7 – 2010 . 13 5. Extravasation of Contrast Media . V7 – 2010 . 17 6. Adverse Events After Intravascular Iodinated Contrast Media . V8 – 2012 . 21 Administration 7. Contrast Media Warming . V8 – 2012 . 29 8. Contrast-Induced Nephrotoxicity . V8 – 2012 . 33 9. Metformin . V7 – 2010 . 43 10. Contrast Media in Children . V7 – 2010 . 47 11. Iodinated Gastrointestinal Contrast Media in Adults: Indications . V7 – 2010 . 55 and Guidelines 12. Adverse Reactions to Gadolinium-Based Contrast Media . V7 – 2010 . 59 13. Nephrogenic Systemic Fibrosis (NSF) . V8 – 2012 . 63 14. Treatment of Contrast Reactions . V8 – 2012 . 73 15. Administration of Contrast Media to Pregnant or Potentially . V6 – 2008. 75 Pregnant Patients 16. Administration of Contrast Media to Breast-Feeding Mothers . V6 – 2008 . 79 Table 1 – Indications for Use of Iodinated Contrast Media . V6 – 2008 . 81 Table 2 – Organ or System-Specific Adverse Effects from the Administration . V7 – 2010 . 82 of Iodine-Based or Gadolinium-Based Contrast Agents Table 3 – Categories of Reactions . V7 – 2010 . 83 Table 4 – Management of Acute Reactions in Children . V7 – 2010 . 84 Table 5 – Management of Acute Reactions in Adults . V6 – 2008 . 86 Table 6 – Equipment for Emergency Carts . V6 – 2008 . -

The Risk of Contrast Media-Induced Ventricular Fibrillation Is Low in Canine Coronary Arteriography with Ioxilan
FULL PAPER Surgery The Risk of Contrast Media-Induced Ventricular Fibrillation is Low in Canine Coronary Arteriography with Ioxilan Kazuhiro MISUMI, Oki TATENO, Makoto FUJIKI, Naoki MIURA and Hiroshi SAKAMOTO Department of Veterinary Medicine, Kagoshima University, 21–24 Korimoto 1-chome, Kagoshima 890–0065, Japan (Received 5 August 1999/Accepted 28 December 1999) ABSTRACT. Previous studies have proposed that sodium supplement to nonionic contrast media (CM) can decrease the risk of ventricular fibrillation (VF). This study was designed to compare the occurence of VF induced by ioxilan (containing 9 mmol/LNa+) with other nonionic CMs. After wedging a catheter in the right coronary artery, test solutions including ioxilan, ioversol, iomeprol, and iopromide were infused for 30 sec at the rate of 0.4 ml/sec or until VF occurred. Then, incidence of VF, contact time (i.e. the time required to produce VF), and QTc were measured. Also, the CMs other than ioxilan were investigated at sodium levels adjusted to 9 and 20 mmol/L Na+. The incidence of VF with ioxilan (0% ) was the lowest of all. In the other CMs, the incidence decreased in accordance with increase of sodium. Iomeprol and iopromide showed significant reduction of VF incidence at the sodium level of 20 mmol/L. The higher sodium supplements also prolonged the contact times. The increase of QTc was the greatest in ioxilan. Ioxilan has the least arrythmogenic property among the current low-osmolality nonionic CMs. This property might be attributable to an optimal sodium concentration of 9 mmol/L in the CM.—KEY WORDS: contrast media, coronary arteriography, ioxilan, ventricular fibrillation. -
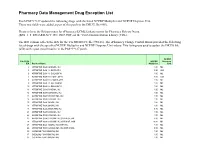
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

Contrast Agents in Pediatric Neuroimaging
Contrast Agents in Pediatric Neuroimaging Sylvester Chuang1 From the Hospital for Sick Children, Toronto, Ontario During the last two decades the development which substitutions are made at the acid group. of contrast agents for myelography, angiography, Examples of common contrast agents used in computed tomography (CT) and magnetic reso North America are listed in Table 1. nance imaging (MR) has been remarkable. What Recent developments have all centered on the follows is a review of contrast agents used in nonionic contrast agents, because these are less neuroradiology-specifically, the ionic and non toxic than the ionics (1); however, the cost of the ionic contrast agents for radiographic/CT proce nonionics is significantly higher than that of the dures, and the paramagnetic contrast agents used ionics. Despite the debate regarding the cost in MR studies. Topics covered are the indications effectiveness of the nonionics (2-9), we routinely for and use of contrast agents, doses and com use nonionic contrast agents for all radiologic parisons, complications and cost benefits, and investigations at the Hospital for Sick Children in what the future of contrast media might hold. Toronto. We do so because of the lower compli cation rate, although there is no convincing evi Iodinated Contrast Agents dence of any decrease in the mortality rate. Nevertheless, when there is extravasation of con The basic structure of iodinated contrast trast into the tissue on IV injection, the morbidity agents is the benzene ring (Fig. 1), with its at is lower. tached iodine atoms. The remaining components Elimination of contrast agents is dependent on are the acid group and organic substitutes which organic substitutions. -

Prescription Medications, Drugs, Herbs & Chemicals Associated With
Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form, or by any means, without the prior written permission of the American Tinnitus Association. ©2013 American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association This document is to be utilized as a conversation tool with your health care provider and is by no means a “complete” listing. Anyone reading this list of ototoxic drugs is strongly advised NOT to discontinue taking any prescribed medication without first contacting the prescribing physician. Just because a drug is listed does not mean that you will automatically get tinnitus, or exacerbate exisiting tinnitus, if you take it. A few will, but many will not. Whether or not you eperience tinnitus after taking one of the listed drugs or herbals, or after being exposed to one of the listed chemicals, depends on many factors ‐ such as your own body chemistry, your sensitivity to drugs, the dose you take, or the length of time you take the drug. It is important to note that there may be drugs NOT listed here that could still cause tinnitus. Although this list is one of the most complete listings of drugs associated with tinnitus, no list of this kind can ever be totally complete – therefore use it as a guide and resource, but do not take it as the final word. The drug brand name is italicized and is followed by the generic drug name in bold. -

Bureau of Prisons Health Services 2018 Summer National Formulary (Part 2)
Bureau of Prisons Health Services 2018 Summer National Formulary (Part 2) IV Refrigeration:N/A Part. GPI Cd: N/A Item Type: N/A MRC Init. Only:No Include NF Use Criteria: Yes DEA Schedule:N/A Project Group: N/A Pill Line Only: No Include Advisory:Yes Include Restrictions:Yes Medi-Span Rt: N/A IV Type: N/A Requires Crushing: No Include. Default Sig: No Unit Dose:No Active Loc.:No Dosage Forms:N/A MLP Requires Cosign:No Form./Non: Formulary Include Look/Sound:No Active: No Changes Since: N/A Include Diagnosis: No MRC Use Only: No Non Substitutable: No Medguide:No Cosign Crush. Active Pill Ln Fmlry Schd. Dose Only Sub. Bulk Req. DEA MLP Loc. Non Unit Doctor Name Item Name Dosage Form GPI Code Abacavir Sulfate (ABC) Oral Soln 20mg/ml Abacavir Sulfate(ABC) Oral Soln 20 MG/ML (240ml) (Ziagen) Sol 12105005102020No 0 Yes No No No N/A No Yes **MLP Requires Cosign** Abacavir Sulfate (ABC) Tablet Abacavir (ABC) 300 MG TAB UD (Ziagen) Tab 12105005100320No 0 Yes No No No N/A Yes Yes Abacavir (ABC) 300 MG TAB (Ziagen) Tab 12105005100320No 0 Yes No No No N/A No Yes **MLP Requires Cosign** Abacavir Sulfate/Lamivudine 600mg/300 mgTablet Abacavir Sulfate/Lamivudine 600MG/300MG TAB (Epzicom) Tab 12109902200340No 0 Yes No No No N/A No Yes Abacavir Sulfate/Lamivudine 600MG/300MG Tab UD (Epzicom) Tab 12109902200340No 0 Yes No No No N/A Yes Yes **MLP Requires Cosign** Abacavir-Lamivudine-Zidovudine Tablet Abacavir-Lamivudine-Zidovud 300-150-300MG TAB UD (Trizivir) Tab 12109903200320No 0 Yes No No No N/A Yes Yes Abacavir-Lamivudine-Zidovudine 300-150-300MG tab