The Class II Tumor-Suppressor Gene RARRES3 Is Expressed in B Cell
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Cell Line P53 Mutation Type UM
A Cell line p53 mutation Type UM-SCC 1 wt UM-SCC5 Exon 5, 157 GTC --> TTC Missense mutation by transversion (Valine --> Phenylalanine UM-SCC6 wt UM-SCC9 wt UM-SCC11A wt UM-SCC11B Exon 7, 242 TGC --> TCC Missense mutation by transversion (Cysteine --> Serine) UM-SCC22A Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC22B Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC38 Exon 5, 132 AAG --> AAT Missense mutation by transversion (Lysine --> Asparagine) UM-SCC46 Exon 8, 278 CCT --> CGT Missense mutation by transversion (Proline --> Alanine) B 1 Supplementary Methods Cell Lines and Cell Culture A panel of ten established HNSCC cell lines from the University of Michigan series (UM-SCC) was obtained from Dr. T. E. Carey at the University of Michigan, Ann Arbor, MI. The UM-SCC cell lines were derived from eight patients with SCC of the upper aerodigestive tract (supplemental Table 1). Patient age at tumor diagnosis ranged from 37 to 72 years. The cell lines selected were obtained from patients with stage I-IV tumors, distributed among oral, pharyngeal and laryngeal sites. All the patients had aggressive disease, with early recurrence and death within two years of therapy. Cell lines established from single isolates of a patient specimen are designated by a numeric designation, and where isolates from two time points or anatomical sites were obtained, the designation includes an alphabetical suffix (i.e., "A" or "B"). The cell lines were maintained in Eagle's minimal essential media supplemented with 10% fetal bovine serum and penicillin/streptomycin. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
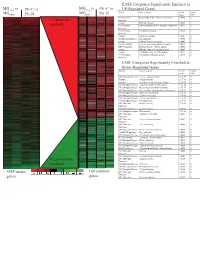
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Gain-Of-Function Genetic Alterations of G9a Drive Oncogenesis
Published OnlineFirst April 8, 2020; DOI: 10.1158/2159-8290.CD-19-0532 RESEARCH ARTICLE Gain-of-Function Genetic Alterations of G9a Drive Oncogenesis Shinichiro Kato 1 , Qing Yu Weng 1 , Megan L. Insco 2 , 3 , 4 , Kevin Y. Chen 2 , 3 , 4 , Sathya Muralidhar 5 , Joanna Pozniak 5 , Joey Mark S. Diaz5 , Yotam Drier 6 , 7 , 8 , Nhu Nguyen 1 , Jennifer A. Lo 1 , Ellen van Rooijen 2 , 3 , Lajos V. Kemeny 1 , Yao Zhan1 , Yang Feng 1 , Whitney Silkworth 1 , C. Thomas Powell 1 , Brian B. Liau 9 , Yan Xiong 10 , Jian Jin 10 , Julia Newton-Bishop5 , Leonard I. Zon 2 , 3 , Bradley E. Bernstein 6 , 7 , 8 , and David E. Fisher 1 . Downloaded from cancerdiscovery.aacrjournals.org on September 25, 2021. © 2020 American Association for Cancer Research. Published OnlineFirst April 8, 2020; DOI: 10.1158/2159-8290.CD-19-0532 ABSTRACT Epigenetic regulators, when genomically altered, may become driver oncogenes that mediate otherwise unexplained pro-oncogenic changes lacking a clear genetic stimulus, such as activation of the WNT/β -catenin pathway in melanoma. This study identifi es previ- ously unrecognized recurrent activating mutations in the G9a histone methyltransferase gene, as well as G9a genomic copy gains in approximately 26% of human melanomas, which collectively drive tumor growth and an immunologically sterile microenvironment beyond melanoma. Furthermore, the WNT pathway is identifi ed as a key tumorigenic target of G9a gain-of-function, via suppression of the WNT antagonist DKK1. Importantly, genetic or pharmacologic suppression of mutated or amplifi ed G9a using multiple in vitro and in vivo models demonstrates that G9a is a druggable target for therapeutic intervention in melanoma and other cancers harboring G9a genomic aberrations. -

Tumor Suppressors in Chronic Lymphocytic Leukemia: from Lost Partners to Active Targets
cancers Review Tumor Suppressors in Chronic Lymphocytic Leukemia: From Lost Partners to Active Targets 1, 1, 2 1 Giacomo Andreani y , Giovanna Carrà y , Marcello Francesco Lingua , Beatrice Maffeo , 3 2, 1, , Mara Brancaccio , Riccardo Taulli y and Alessandro Morotti * y 1 Department of Clinical and Biological Sciences, University of Torino, 10043 Orbassano, Italy; [email protected] (G.A.); [email protected] (G.C.); beatrice.maff[email protected] (B.M.) 2 Department of Oncology, University of Torino, 10043 Orbassano, Italy; [email protected] (M.F.L.); [email protected] (R.T.) 3 Department of Molecular Biotechnology and Health Sciences, University of Torino, 10126 Turin, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-011-9026305 These authors equally contributed to the work. y Received: 21 January 2020; Accepted: 4 March 2020; Published: 9 March 2020 Abstract: Tumor suppressors play an important role in cancer pathogenesis and in the modulation of resistance to treatments. Loss of function of the proteins encoded by tumor suppressors, through genomic inactivation of the gene, disable all the controls that balance growth, survival, and apoptosis, promoting cancer transformation. Parallel to genetic impairments, tumor suppressor products may also be functionally inactivated in the absence of mutations/deletions upon post-transcriptional and post-translational modifications. Because restoring tumor suppressor functions remains the most effective and selective approach to induce apoptosis in cancer, the dissection of mechanisms of tumor suppressor inactivation is advisable in order to further augment targeted strategies. This review will summarize the role of tumor suppressors in chronic lymphocytic leukemia and attempt to describe how tumor suppressors can represent new hopes in our arsenal against chronic lymphocytic leukemia (CLL). -

(BPA) Exposure Biomarkers in Ovarian Cancer
Journal of Clinical Medicine Article Identification of Potential Bisphenol A (BPA) Exposure Biomarkers in Ovarian Cancer Aeman Zahra 1, Qiduo Dong 1, Marcia Hall 1,2 , Jeyarooban Jeyaneethi 1, Elisabete Silva 1, Emmanouil Karteris 1,* and Cristina Sisu 1,* 1 Biosciences, College of Health, Medicine and Life Sciences, Brunel University London, Uxbridge UB8 3PH, UK; [email protected] (A.Z.); [email protected] (Q.D.); [email protected] (M.H.); [email protected] (J.J.); [email protected] (E.S.) 2 Mount Vernon Cancer Centre, Northwood HA6 2RN, UK * Correspondence: [email protected] (E.K.); [email protected] (C.S.) Abstract: Endocrine-disrupting chemicals (EDCs) can exert multiple deleterious effects and have been implicated in carcinogenesis. The xenoestrogen Bisphenol A (BPA) that is found in various consumer products has been involved in the dysregulation of numerous signalling pathways. In this paper, we present the analysis of a set of 94 genes that have been shown to be dysregulated in presence of BPA in ovarian cancer cell lines since we hypothesised that these genes might be of biomarker potential. This study sought to identify biomarkers of disease and biomarkers of disease- associated exposure. In silico analyses took place using gene expression data extracted from The Cancer Genome Atlas (TCGA) and the Genotype-Tissue Expression (GTEx) databases. Differential expression was further validated at protein level using immunohistochemistry on an ovarian cancer tissue microarray. We found that 14 out of 94 genes are solely dysregulated in the presence of BPA, while the remaining 80 genes are already dysregulated (p-value < 0.05) in their expression pattern Citation: Zahra, A.; Dong, Q.; Hall, as a consequence of the disease. -

Clinically Annotated Breast, Ovarian and Pancreatic Cancer
www.nature.com/scientificreports OPEN MetaGxData: Clinically Annotated Breast, Ovarian and Pancreatic Cancer Datasets and their Use in Received: 19 November 2018 Accepted: 31 May 2019 Generating a Multi-Cancer Gene Published: xx xx xxxx Signature Deena M. A. Gendoo 1, Michael Zon2,4, Vandana Sandhu2, Venkata S. K. Manem2,3,5, Natchar Ratanasirigulchai2, Gregory M. Chen2, Levi Waldron 6 & Benjamin Haibe- Kains2,3,7,8,9 A wealth of transcriptomic and clinical data on solid tumours are under-utilized due to unharmonized data storage and format. We have developed the MetaGxData package compendium, which includes manually-curated and standardized clinical, pathological, survival, and treatment metadata across breast, ovarian, and pancreatic cancer data. MetaGxData is the largest compendium of curated transcriptomic data for these cancer types to date, spanning 86 datasets and encompassing 15,249 samples. Open access to standardized metadata across cancer types promotes use of their transcriptomic and clinical data in a variety of cross-tumour analyses, including identifcation of common biomarkers, and assessing the validity of prognostic signatures. Here, we demonstrate that MetaGxData is a fexible framework that facilitates meta-analyses by using it to identify common prognostic genes in ovarian and breast cancer. Furthermore, we use the data compendium to create the frst gene signature that is prognostic in a meta-analysis across 3 cancer types. These fndings demonstrate the potential of MetaGxData to serve as an important resource in oncology research, and provide a foundation for future development of cancer-specifc compendia. Ovarian, breast and pancreatic cancers are among the leading causes of cancer deaths among women, and recent studies have identifed biological and molecular commonalities between them1–4. -

A Bacterial Protein Targets the BAHD1 Chromatin Complex to Stimulate Type III Interferon Response
A bacterial protein targets the BAHD1 chromatin complex to stimulate type III interferon response Alice Lebreton, Goran Lakisic, Viviana Job, Lauriane Fritsch, To Nam Tham, Ana Camejo, Pierre-Jean Matteï, Béatrice Regnault, Marie-Anne Nahori, Didier Cabanes, et al. To cite this version: Alice Lebreton, Goran Lakisic, Viviana Job, Lauriane Fritsch, To Nam Tham, et al.. A bacterial protein targets the BAHD1 chromatin complex to stimulate type III interferon response. Science, American Association for the Advancement of Science, 2011, 331 (6022), pp.1319-21. 10.1126/sci- ence.1200120. cea-00819299 HAL Id: cea-00819299 https://hal-cea.archives-ouvertes.fr/cea-00819299 Submitted on 26 Jul 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Lebreton et al. Science 2011 doi:10.1126/science.1200120 A Bacterial Protein Targets the BAHD1 Chromatin Complex to Stimulate Type III Interferon Response Alice Lebreton1,2,3, Goran Lakisic4, Viviana Job5, Lauriane Fritsch6, To Nam Tham1,2,3, Ana Camejo7, Pierre-Jean Matteï5, Béatrice Regnault8, Marie-Anne Nahori1,2,3, Didier Cabanes7, Alexis Gautreau4, Slimane Ait-Si-Ali6, Andréa Dessen5, Pascale Cossart1,2,3* and Hélène Bierne1,2,3* 1. -

Integrating Structure to Protein-Protein Interaction Networks That Drive Metastasis to Brain and Lung in Breast Cancer
Integrating Structure to Protein-Protein Interaction Networks That Drive Metastasis to Brain and Lung in Breast Cancer H. Billur Engin1, Emre Guney2, Ozlem Keskin1, Baldo Oliva2, Attila Gursoy1* 1 Center for Computational Biology and Bioinformatics and College of Engineering, Koc University, Istanbul, Turkey, 2 Structural Bioinformatics Group (GRIB), Universitat Pompeu Fabra Abstract Blocking specific protein interactions can lead to human diseases. Accordingly, protein interactions and the structural knowledge on interacting surfaces of proteins (interfaces) have an important role in predicting the genotype- phenotype relationship. We have built the phenotype specific sub-networks of protein-protein interactions (PPIs) involving the relevant genes responsible for lung and brain metastasis from primary tumor in breast cancer. First, we selected the PPIs most relevant to metastasis causing genes (seed genes), by using the “guilt-by-association” principle. Then, we modeled structures of the interactions whose complex forms are not available in Protein Databank (PDB). Finally, we mapped mutations to interface structures (real and modeled), in order to spot the interactions that might be manipulated by these mutations. Functional analyses performed on these sub-networks revealed the potential relationship between immune system-infectious diseases and lung metastasis progression, but this connection was not observed significantly in the brain metastasis. Besides, structural analyses showed that some PPI interfaces in both metastasis sub-networks are originating from microbial proteins, which in turn were mostly related with cell adhesion. Cell adhesion is a key mechanism in metastasis, therefore these PPIs may be involved in similar molecular pathways that are shared by infectious disease and metastasis. Finally, by mapping the mutations and amino acid variations on the interface regions of the proteins in the metastasis sub-networks we found evidence for some mutations to be involved in the mechanisms differentiating the type of the metastasis. -

Downregulation of SNRPG Induces Cell Cycle Arrest and Sensitizes Human Glioblastoma Cells to Temozolomide by Targeting Myc Through a P53-Dependent Signaling Pathway
Cancer Biol Med 2020. doi: 10.20892/j.issn.2095-3941.2019.0164 ORIGINAL ARTICLE Downregulation of SNRPG induces cell cycle arrest and sensitizes human glioblastoma cells to temozolomide by targeting Myc through a p53-dependent signaling pathway Yulong Lan1,2*, Jiacheng Lou2*, Jiliang Hu1, Zhikuan Yu1, Wen Lyu1, Bo Zhang1,2 1Department of Neurosurgery, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, The First Affiliated Hospital of Southern University of Science and Technology, Shenzhen 518020, China;2 Department of Neurosurgery, The Second Affiliated Hospital of Dalian Medical University, Dalian 116023, China ABSTRACT Objective: Temozolomide (TMZ) is commonly used for glioblastoma multiforme (GBM) chemotherapy. However, drug resistance limits its therapeutic effect in GBM treatment. RNA-binding proteins (RBPs) have vital roles in posttranscriptional events. While disturbance of RBP-RNA network activity is potentially associated with cancer development, the precise mechanisms are not fully known. The SNRPG gene, encoding small nuclear ribonucleoprotein polypeptide G, was recently found to be related to cancer incidence, but its exact function has yet to be elucidated. Methods: SNRPG knockdown was achieved via short hairpin RNAs. Gene expression profiling and Western blot analyses were used to identify potential glioma cell growth signaling pathways affected by SNRPG. Xenograft tumors were examined to determine the carcinogenic effects of SNRPG on glioma tissues. Results: The SNRPG-mediated inhibitory effect on glioma cells might be due to the targeted prevention of Myc and p53. In addition, the effects of SNRPG loss on p53 levels and cell cycle progression were found to be Myc-dependent. Furthermore, SNRPG was increased in TMZ-resistant GBM cells, and downregulation of SNRPG potentially sensitized resistant cells to TMZ, suggesting that SNRPG deficiency decreases the chemoresistance of GBM cells to TMZ via the p53 signaling pathway. -

Ncounter® Human Autoimmune Profiling Panel
nCounter® Human AutoImmune Profiling Panel - Gene and Probe Details Official Symbol Accession Alias / Previous Symbol Official Full Name Other targets or Isoform Information ACE NM_000789.2 DCP1;angiotensin I converting enzyme (peptidyl-dipeptidase A) 1 angiotensin I converting enzyme ACIN1 NM_001164815.1 ACINUS;apoptotic chromatin condensation inducer in the nucleus apoptotic chromatin condensation inducer 1 ACP5 NM_001611.3 acid phosphatase 5, tartrate resistant CTRN2;ARP1 (actin-related protein 1, yeast) homolog B (centractin beta),ARP1 actin-related ACTR1B NM_005735.3 protein 1 homolog B, centractin beta ARP1 actin related protein 1 homolog B ADAM17 NM_003183.4 TACE;tumor necrosis factor, alpha, converting enzyme ADAM metallopeptidase domain 17 ADAR NM_001111.3 IFI4,G1P1;interferon-induced protein 4 adenosine deaminase, RNA specific ADORA2A NM_000675.3 ADORA2 adenosine A2a receptor AGER NM_001136.3 advanced glycosylation end-product specific receptor AGT NM_000029.3 SERPINA8;serpin peptidase inhibitor, clade A, member 8 angiotensinogen AHR NM_001621.3 aryl hydrocarbon receptor AICDA NM_020661.2 activation-induced cytidine deaminase activation induced cytidine deaminase AIM2 NM_004833.1 absent in melanoma 2 APECED;autoimmune regulator (autoimmune polyendocrinopathy candidiasis ectodermal AIRE NM_000383.2 dystrophy) autoimmune regulator AKT1 NM_001014432.1 v-akt murine thymoma viral oncogene homolog 1 AKT serine/threonine kinase 1 AKT2 NM_001626.4 v-akt murine thymoma viral oncogene homolog 2 AKT serine/threonine kinase 2 AKT3 NM_005465.4 -

Regulation of Cancer Stemness in Breast Ductal Carcinoma in Situ by Vitamin D Compounds
Author Manuscript Published OnlineFirst on May 28, 2020; DOI: 10.1158/1940-6207.CAPR-19-0566 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Analysis of the Transcriptome: Regulation of Cancer Stemness in Breast Ductal Carcinoma In Situ by Vitamin D Compounds Naing Lin Shan1, Audrey Minden1,5, Philip Furmanski1,5, Min Ji Bak1, Li Cai2,5, Roman Wernyj1, Davit Sargsyan3, David Cheng3, Renyi Wu3, Hsiao-Chen D. Kuo3, Shanyi N. Li3, Mingzhu Fang4, Hubert Maehr1, Ah-Ng Kong3,5, Nanjoo Suh1,5 1Department of Chemical Biology, Ernest Mario School of Pharmacy; 2Department of Biomedical Engineering, School of Engineering; 3Department of Pharmaceutics, Ernest Mario School of Pharmacy; 4Environmental and Occupational Health Sciences Institute and School of Public Health, 5Rutgers Cancer Institute of New Jersey, New Brunswick; Rutgers, The State University of New Jersey, NJ, USA Running title: Regulation of cancer stemness by vitamin D compounds Key words: Breast cancer, cancer stemness, gene expression, DCIS, vitamin D compounds Financial Support: This research was supported by the National Institutes of Health grant R01 AT007036, R01 AT009152, ES005022, Charles and Johanna Busch Memorial Fund at Rutgers University and the New Jersey Health Foundation. Corresponding author: Dr. Nanjoo Suh, Department of Chemical Biology, Ernest Mario School of Pharmacy, Rutgers, The State University of New Jersey, 164 Frelinghuysen Road, Piscataway, New Jersey 08854. Tel: 848-445-8030, Fax: 732-445-0687; e-mail: [email protected] Disclosure of Conflict of Interest: “The authors declare no potential conflicts of interest” 1 Downloaded from cancerpreventionresearch.aacrjournals.org on October 1, 2021.