Tumor Suppressors in Chronic Lymphocytic Leukemia: from Lost Partners to Active Targets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![USP7 [6His-Tagged] Deubiquitylating Enzyme](https://docslib.b-cdn.net/cover/3097/usp7-6his-tagged-deubiquitylating-enzyme-43097.webp)
USP7 [6His-Tagged] Deubiquitylating Enzyme
USP7 [6His-tagged] Deubiquitylating Enzyme Alternate Names: Herpesvirus-Associated Ubiquitin-Specific Protease, HAUSP VMW110- associated protein Cat. No. 64-0003-050 Quantity: 50 µg Lot. No. 1736 Storage: -70˚C FOR RESEARCH USE ONLY NOT FOR USE IN HUMANS CERTIFICATE OF ANALYSIS Page 1 of 2 Background Physical Characteristics The deubiquitylating enzymes (DUBs) Species: human Protein Sequence: Please see page 2 regulate ubiquitin dependent signaling pathways. The activities of the DUBs Source: E. coli expression include the generation of free ubiquitin from precursor molecules, the recy- Quantity: 50 μg cling of ubiquitin following substrate Concentration: 0.5 mg/ml degradation to maintain cellular ubiq- uitin homeostasis and the removal Formulation: 50 mM HEPES pH 7.5, of ubiquitin or ubiquitin-like proteins 150 mM sodium chloride, 2 mM (UBL) modifications through chain dithiothreitol, 10% glycerol editing to rescue proteins from protea- somal degradation or to influence cell Molecular Weight: ~130 kDa signalling events (Komander et al., 2009). There are two main classes of Purity: >80% by InstantBlue™ SDS-PAGE DUB, cysteine proteases and metallo- Stability/Storage: 12 months at -70˚C; proteases. Ubiquitin specific process- aliquot as required ing protease 7 (USP-7) is a member of the cysteine protease enzyme fam- ily and cloning of the gene in humans Quality Assurance was first described by Everett et al. (1997). Overexpression of p53 and Purity: Protein Identification: USP7 stabilizes p53 through the re- 4-12% gradient SDS-PAGE Confirmed by mass spectrometry. InstantBlue™ staining moval of ubiquitin moieties from polyu- Lane 1: MW markers Deubiquitylating Enzyme Assay: biquitylated p53 (Kon et al., 2010). -

Therapeutic Inhibition of USP7-PTEN Network in Chronic Lymphocytic Leukemia: a Strategy to Overcome TP53 Mutated/ Deleted Clones
www.impactjournals.com/oncotarget/ Oncotarget, 2017, Vol. 8, (No. 22), pp: 35508-35522 Priority Research Paper Therapeutic inhibition of USP7-PTEN network in chronic lymphocytic leukemia: a strategy to overcome TP53 mutated/ deleted clones Giovanna Carrà1, Cristina Panuzzo1, Davide Torti1,2, Guido Parvis2,3, Sabrina Crivellaro1, Ubaldo Familiari4, Marco Volante4,5, Deborah Morena5, Marcello Francesco Lingua5, Mara Brancaccio6, Angelo Guerrasio1, Pier Paolo Pandolfi7, Giuseppe Saglio1,2,3, Riccardo Taulli5 and Alessandro Morotti1 1 Department of Clinical and Biological Sciences, University of Turin, San Luigi Gonzaga Hospital, Orbassano, Italy 2 Division of Internal Medicine - Hematology, San Luigi Gonzaga Hospital, Orbassano, Italy 3 Division of Hematology, Azienda Ospedaliera, Mauriziano, Torino, Italy 4 Division of Pathology, San Luigi Hospital, Orbassano, Italy 5 Department of Oncology, University of Turin, San Luigi Gonzaga Hospital, Orbassano, Italy 6 Department of Molecular Biotechnology and Health Sciences, University of Torino, Torino, Italy 7 Cancer Genetics Program, Beth Israel Deaconess Cancer Center, Department of Medicine and Pathology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA Correspondence to: Alessandro Morotti, email: [email protected] Correspondence to: Riccardo Taulli, email: [email protected] Keywords: chronic lymphocytic leukemia, USP7, PTEN, miR181, miR338 Received: June 14, 2016 Accepted: February 20, 2017 Published: March 17, 2017 Copyright: Carrà et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC-BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT Chronic Lymphocytic Leukemia (CLL) is a lymphoproliferative disorder with either indolent or aggressive clinical course. -

Evolution of Multiple Cell Clones Over a 29-Year Period of a CLL Patient
ARTICLE Received 11 May 2016 | Accepted 1 Nov 2016 | Published 16 Dec 2016 DOI: 10.1038/ncomms13765 OPEN Evolution of multiple cell clones over a 29-year period of a CLL patient Zhikun Zhao1,2,3,*, Lynn Goldin4,*, Shiping Liu1,5,*, Liang Wu1,*, Weiyin Zhou6,*, Hong Lou6,*, Qichao Yu1,7, Shirley X. Tsang8, Miaomiao Jiang1,3, Fuqiang Li1, MaryLou McMaster4, Yang Li1, Xinxin Lin1, Zhifeng Wang1, Liqin Xu1, Gerald Marti9, Guibo Li1,10,KuiWu1,10, Meredith Yeager6, Huanming Yang1,11, Xun Xu1,**, Stephen J. Chanock4,**, Bo Li1,**, Yong Hou1,10,**, Neil Caporaso4,** & Michael Dean1,4,** Chronic lymphocytic leukaemia (CLL) is a frequent B-cell malignancy, characterized by recurrent somatic chromosome alterations and a low level of point mutations. Here we present single-nucleotide polymorphism microarray analyses of a single CLL patient over 29 years of observation and treatment, and transcriptome and whole-genome sequencing at selected time points. We identify chromosome alterations 13q14 À ,6qÀ and 12q þ in early cell clones, elimination of clonal populations following therapy, and subsequent appearance of a clone containing trisomy 12 and chromosome 10 copy-neutral loss of heterogeneity that marks a major population dominant at death. Serial single-cell RNA sequencing reveals an expression pattern with high FOS, JUN and KLF4 at disease acceleration, which resolves following therapy, but reoccurs following relapse and death. Transcriptome evolution indicates complex changes in expression occur over time. In conclusion, CLL can evolve gradually during indolent phases, and undergo rapid changes following therapy. 1 BGI-Shenzhen, Shenzhen 518083, China. 2 State Key Laboratory of Bioelectronics, Southeast University, Nanjing 210096, China. -

Non-Coding Rnas As Cancer Hallmarks in Chronic Lymphocytic Leukemia
International Journal of Molecular Sciences Review Non-Coding RNAs as Cancer Hallmarks in Chronic Lymphocytic Leukemia Linda Fabris 1, Jaroslav Juracek 2 and George Calin 1,* 1 Department of Translational Molecular Pathology, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] 2 Department of Experimental Therapeutics, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] * Correspondence: [email protected] Received: 24 July 2020; Accepted: 10 September 2020; Published: 14 September 2020 Abstract: The discovery of non-coding RNAs (ncRNAs) and their role in tumor onset and progression has revolutionized the way scientists and clinicians study cancers. This discovery opened new layers of complexity in understanding the fine-tuned regulation of cellular processes leading to cancer. NcRNAs represent a heterogeneous group of transcripts, ranging from a few base pairs to several kilobases, that are able to regulate gene networks and intracellular pathways by interacting with DNA, transcripts or proteins. Deregulation of ncRNAs impinge on several cellular responses and can play a major role in each single hallmark of cancer. This review will focus on the most important short and long non-coding RNAs in chronic lymphocytic leukemia (CLL), highlighting their implications as potential biomarkers and therapeutic targets as they relate to the well-established hallmarks of cancer. The key molecular events in the onset of CLL will be contextualized, taking into account the role of the “dark matter” of the genome. Keywords: chronic lymphocytic leukemia; lncRNA; miRNA; hallmarks 1. Introduction: Current Status of Chronic Lymphocytic Leukemia Research Chronic lymphocytic leukemia (CLL) is the most common leukemia in adults in the Western world, representing more than 30% of all leukemia cases [1]. -

A Cell Line P53 Mutation Type UM
A Cell line p53 mutation Type UM-SCC 1 wt UM-SCC5 Exon 5, 157 GTC --> TTC Missense mutation by transversion (Valine --> Phenylalanine UM-SCC6 wt UM-SCC9 wt UM-SCC11A wt UM-SCC11B Exon 7, 242 TGC --> TCC Missense mutation by transversion (Cysteine --> Serine) UM-SCC22A Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC22B Exon 6, 220 TAT --> TGT Missense mutation by transition (Tyrosine --> Cysteine) UM-SCC38 Exon 5, 132 AAG --> AAT Missense mutation by transversion (Lysine --> Asparagine) UM-SCC46 Exon 8, 278 CCT --> CGT Missense mutation by transversion (Proline --> Alanine) B 1 Supplementary Methods Cell Lines and Cell Culture A panel of ten established HNSCC cell lines from the University of Michigan series (UM-SCC) was obtained from Dr. T. E. Carey at the University of Michigan, Ann Arbor, MI. The UM-SCC cell lines were derived from eight patients with SCC of the upper aerodigestive tract (supplemental Table 1). Patient age at tumor diagnosis ranged from 37 to 72 years. The cell lines selected were obtained from patients with stage I-IV tumors, distributed among oral, pharyngeal and laryngeal sites. All the patients had aggressive disease, with early recurrence and death within two years of therapy. Cell lines established from single isolates of a patient specimen are designated by a numeric designation, and where isolates from two time points or anatomical sites were obtained, the designation includes an alphabetical suffix (i.e., "A" or "B"). The cell lines were maintained in Eagle's minimal essential media supplemented with 10% fetal bovine serum and penicillin/streptomycin. -

Targeting Mdm2 and Mdmx in Cancer Therapy: Better Living Through Medicinal Chemistry?
Subject Review Targeting Mdm2 and Mdmx in Cancer Therapy: Better Living through Medicinal Chemistry? Mark Wade and Geoffrey M.Wahl Gene Expression Laboratory, Salk Institute for Biological Studies, La Jolla, California Abstract In the second model, Mdm2 and Mdmx are proposed to form Genomic and proteomic profiling of human tumor a complex that is more effective at inhibiting p53 transactiva- samples and tumor-derived cell lines are essential for tion or enhancing p53 turnover. Although the former possibility the realization of personalized therapy in oncology. has not been excluded, several studies indicate that Mdm2 Identification of the changes required for tumor initiation and Mdmx function as a heterodimeric pair to augment p53 or maintenance will likely provide new targets for degradation. Mdm2 is a member of the RING E3 ubiquitin small-molecule and biological therapeutics.For ligase family and promotes proteasome-dependent degradation example, inactivation of the p53 tumor suppressor of p53. By binding to the target substrate and to an E2 ubiquitin- pathway occurs in most human cancers.Although this conjugating enzyme, RING E3s facilitate E2-to-substrate can be due to frank p53 gene mutation, almost half of all ubiquitin transfer (5). Similar to other RING E3s, it does not cancers retain the wild-type p53 allele, indicating that seem that Mdm2 forms a covalent link with ubiquitin during the pathway is disabled by other means.Alternate the reaction. Thus, Mdm2 does not have a ‘‘classic’’ catalytic mechanisms include deletion or epigenetic inactivation site but acts as a molecular scaffold that presumably positions of the p53-positive regulator arf, methylation of the p53 p53 for E2-dependent ubiquitination (Fig. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

USP7 Couples DNA Replication Termination to Mitotic Entry
bioRxiv preprint doi: https://doi.org/10.1101/305318; this version posted April 20, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. USP7 couples DNA replication termination to mitotic entry Antonio Galarreta1*, Emilio Lecona1*, Pablo Valledor1, Patricia Ubieto1,2, Vanesa Lafarga1, Julia Specks1 & Oscar Fernandez-Capetillo1,3 1Genomic Instability Group, Spanish National Cancer Research Centre (CNIO), Madrid 28029, Spain 2Current Address: DNA Replication Group, Spanish National Cancer Research Centre (CNIO), Madrid 28029, Spain 3Science for Life Laboratory, Division of Genome Biology, Department of Medical Biochemistry and Biophysics, Karolinska Institute, S-171 21 Stockholm, Sweden *Co-first authors Correspondence: E.L. ([email protected]) or O.F. ([email protected]) Lead Contact: Oscar Fernandez-Capetillo Spanish National Cancer Research Centre (CNIO) Melchor Fernandez Almagro, 3 Madrid 28029, Spain Tel.: +34.91.732.8000 Ext: 3480 Fax: +34.91.732.8028 Email: [email protected] KEYWORDS: USP7; CDK1; DNA REPLICATION; MITOSIS; S/M TRANSITION. bioRxiv preprint doi: https://doi.org/10.1101/305318; this version posted April 20, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. USP7 coordinates the S/M transition 2 SUMMARY To ensure a faithful segregation of chromosomes, DNA must be fully replicated before mitotic entry. However, how cells sense the completion of DNA replication and to what extent this is linked to the activation of the mitotic machinery remains poorly understood. We previously showed that USP7 is a replisome-associated deubiquitinase with an essential role in DNA replication. -
Supplement 1 Microarray Studies
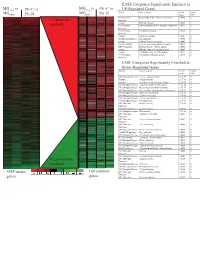
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Gain-Of-Function Genetic Alterations of G9a Drive Oncogenesis
Published OnlineFirst April 8, 2020; DOI: 10.1158/2159-8290.CD-19-0532 RESEARCH ARTICLE Gain-of-Function Genetic Alterations of G9a Drive Oncogenesis Shinichiro Kato 1 , Qing Yu Weng 1 , Megan L. Insco 2 , 3 , 4 , Kevin Y. Chen 2 , 3 , 4 , Sathya Muralidhar 5 , Joanna Pozniak 5 , Joey Mark S. Diaz5 , Yotam Drier 6 , 7 , 8 , Nhu Nguyen 1 , Jennifer A. Lo 1 , Ellen van Rooijen 2 , 3 , Lajos V. Kemeny 1 , Yao Zhan1 , Yang Feng 1 , Whitney Silkworth 1 , C. Thomas Powell 1 , Brian B. Liau 9 , Yan Xiong 10 , Jian Jin 10 , Julia Newton-Bishop5 , Leonard I. Zon 2 , 3 , Bradley E. Bernstein 6 , 7 , 8 , and David E. Fisher 1 . Downloaded from cancerdiscovery.aacrjournals.org on September 25, 2021. © 2020 American Association for Cancer Research. Published OnlineFirst April 8, 2020; DOI: 10.1158/2159-8290.CD-19-0532 ABSTRACT Epigenetic regulators, when genomically altered, may become driver oncogenes that mediate otherwise unexplained pro-oncogenic changes lacking a clear genetic stimulus, such as activation of the WNT/β -catenin pathway in melanoma. This study identifi es previ- ously unrecognized recurrent activating mutations in the G9a histone methyltransferase gene, as well as G9a genomic copy gains in approximately 26% of human melanomas, which collectively drive tumor growth and an immunologically sterile microenvironment beyond melanoma. Furthermore, the WNT pathway is identifi ed as a key tumorigenic target of G9a gain-of-function, via suppression of the WNT antagonist DKK1. Importantly, genetic or pharmacologic suppression of mutated or amplifi ed G9a using multiple in vitro and in vivo models demonstrates that G9a is a druggable target for therapeutic intervention in melanoma and other cancers harboring G9a genomic aberrations. -

The Role of Ubiquitination in NF-Κb Signaling During Virus Infection
viruses Review The Role of Ubiquitination in NF-κB Signaling during Virus Infection Kun Song and Shitao Li * Department of Microbiology and Immunology, Tulane University, New Orleans, LA 70112, USA; [email protected] * Correspondence: [email protected] Abstract: The nuclear factor κB (NF-κB) family are the master transcription factors that control cell proliferation, apoptosis, the expression of interferons and proinflammatory factors, and viral infection. During viral infection, host innate immune system senses viral products, such as viral nucleic acids, to activate innate defense pathways, including the NF-κB signaling axis, thereby inhibiting viral infection. In these NF-κB signaling pathways, diverse types of ubiquitination have been shown to participate in different steps of the signal cascades. Recent advances find that viruses also modulate the ubiquitination in NF-κB signaling pathways to activate viral gene expression or inhibit host NF-κB activation and inflammation, thereby facilitating viral infection. Understanding the role of ubiquitination in NF-κB signaling during viral infection will advance our knowledge of regulatory mechanisms of NF-κB signaling and pave the avenue for potential antiviral therapeutics. Thus, here we systematically review the ubiquitination in NF-κB signaling, delineate how viruses modulate the NF-κB signaling via ubiquitination and discuss the potential future directions. Keywords: NF-κB; polyubiquitination; linear ubiquitination; inflammation; host defense; viral infection Citation: Song, K.; Li, S. The Role of 1. Introduction Ubiquitination in NF-κB Signaling The nuclear factor κB (NF-κB) is a small family of five transcription factors, including during Virus Infection. Viruses 2021, RelA (also known as p65), RelB, c-Rel, p50 and p52 [1]. -

Structural Insight Into the Mechanisms of Activation and Substrate
University of Connecticut OpenCommons@UConn Doctoral Dissertations University of Connecticut Graduate School 12-12-2016 Structural Insight into the Mechanisms of Activation and Substrate Specificity of Human Deubiquitinating Enzyme USP7 Alexandra Pozhidaeva University of Connecticut, [email protected] Follow this and additional works at: https://opencommons.uconn.edu/dissertations Recommended Citation Pozhidaeva, Alexandra, "Structural Insight into the Mechanisms of Activation and Substrate Specificity of Human Deubiquitinating Enzyme USP7" (2016). Doctoral Dissertations. 1287. https://opencommons.uconn.edu/dissertations/1287 Structural Insight into the Mechanisms of Activation and Substrate Specificity of Human Deubiquitinating Enzyme USP7 Alexandra Pozhidaeva, PhD University of Connecticut, 2016 The major part of this thesis describes studies of human ubiquitin-specific protease 7 (USP7), a deubiquitinating enzyme that regulates cellular levels of key oncoproteins and tumor suppressors. Inactivation of USP7 has recently emerged as a new approach to treatment of malignancies. However, design of potent and specific small-molecule compounds requires detailed understanding of the molecular mechanisms of USP7 substrate recognition and regulation of its catalytic activity. The goal of this work was to explore these mechanisms using solution nuclear magnetic resonance spectroscopy in combination with other methods. In our studies of USP7 substrate recognition, we structurally characterized its interaction with ICP0 protein from Herpes Simplex virus 1 and identified a novel USP7 substrate-binding site harbored within its C-terminal region. To address the question of USP7 activity regulation, we investigated its interaction with ubiquitin, which was believed to cause structural rearrangement of USP7 active site from an unproductive to a catalytically competent conformation. Surprisingly, we showed that in solution USP7 – ubiquitin interaction alone is not sufficient for activation of the enzyme as was previously postulated.