J Venom Anim Toxins Incl Trop Dis, 2019, E20190017 Page 2 of 15
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Abacca Mosaic Virus
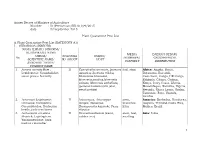
Annex Decree of Ministry of Agriculture Number : 51/Permentan/KR.010/9/2015 date : 23 September 2015 Plant Quarantine Pest List A. Plant Quarantine Pest List (KATEGORY A1) I. SERANGGA (INSECTS) NAMA ILMIAH/ SINONIM/ KLASIFIKASI/ NAMA MEDIA DAERAH SEBAR/ UMUM/ GOLONGA INANG/ No PEMBAWA/ GEOGRAPHICAL SCIENTIFIC NAME/ N/ GROUP HOST PATHWAY DISTRIBUTION SYNONIM/ TAXON/ COMMON NAME 1. Acraea acerata Hew.; II Convolvulus arvensis, Ipomoea leaf, stem Africa: Angola, Benin, Lepidoptera: Nymphalidae; aquatica, Ipomoea triloba, Botswana, Burundi, sweet potato butterfly Merremiae bracteata, Cameroon, Congo, DR Congo, Merremia pacifica,Merremia Ethiopia, Ghana, Guinea, peltata, Merremia umbellata, Kenya, Ivory Coast, Liberia, Ipomoea batatas (ubi jalar, Mozambique, Namibia, Nigeria, sweet potato) Rwanda, Sierra Leone, Sudan, Tanzania, Togo. Uganda, Zambia 2. Ac rocinus longimanus II Artocarpus, Artocarpus stem, America: Barbados, Honduras, Linnaeus; Coleoptera: integra, Moraceae, branches, Guyana, Trinidad,Costa Rica, Cerambycidae; Herlequin Broussonetia kazinoki, Ficus litter Mexico, Brazil beetle, jack-tree borer elastica 3. Aetherastis circulata II Hevea brasiliensis (karet, stem, leaf, Asia: India Meyrick; Lepidoptera: rubber tree) seedling Yponomeutidae; bark feeding caterpillar 1 4. Agrilus mali Matsumura; II Malus domestica (apel, apple) buds, stem, Asia: China, Korea DPR (North Coleoptera: Buprestidae; seedling, Korea), Republic of Korea apple borer, apple rhizome (South Korea) buprestid Europe: Russia 5. Agrilus planipennis II Fraxinus americana, -
CGC 21 (1998) Cucurbit Genetics Cooperative
CGC 21 (1998) Cucurbit Genetics Cooperative Report No. 21 July 1998 Table of Contents (article titles linked to html files) Introduction Comments from the CGC Coordinating Committee Comments from the CGC Gene List Committee Comments from the CGC Gene Curators Cucurbitaceae '98: Evaluation and Enhancement of Cucurbit Germplasm 1997 Annual CGC Business Meeting 1998 Annual CGC Business Meeting Cucurbit Crops Germplasm Committee Update 18th Annual Meeting of the Watermelon Research and Development Group Upcoming Meetings of Interest to Cucurbit Researchers Cucumber (Cucumis sativus) 1. Relationships among Putative Botanical Varieties in Cucumber Jinsheng Liu (P.R. China) and Jack E. Staub (USA) CGC 21:1-5 (1998) 2. Paternal Inheritance of Mitochondrial DNA in Cucumber: Confirmation by PCR Method S. Matsuura, H. Mizusawa and K. Kadowaki (Japan) CGC 21:6-7 (1998) 3. Effects of Copper Seedcoat Agent on Cucumber Germination and Seedling Growth Meng Huanwen, Cui Hongwen, Cheng Zhihui and He Danrao (P.R. China) CGC 21:8-10 (1998) 4. The Relationship Between Low-temperature Germination and Chilling Tolerance in Cucumber Jianguo Li, Hongwen Cui and Meng Zhang (P.R. China) CGC 21:11-13 (1998) 5. Ethylene Production and the Evaluation of Tolerance to Low-temperature in Cucumber (Cucumis sativus L.) Yu Shuancang and Cui Hongwen (P.R. China) CGC 21:14-15 (1998) 6. Free Proline Contents and Catalase Activity in Cucumber Leaves at Elevated Temperatures Meng Zhang, Hongwen Cui and Sheng Zhao (P.R. China) CGC 21:16-17 (1998) 7. Stand Correction Methods for Cucumber Fruit Yield Christopher S. Cramer and Todd C. Wehner (USA) CGC 21:18-20 (1998) 8. -

The Dynamics of Medicinal Plants Utilization Practice Nexus Its Health and Economic Role in Ethiopia: a Review Paper
Vol. 11(1), pp. 31-47, January 2019 DOI: 10.5897/IJBC2018.1201 Article Number: 414D9D059783 ISSN 2141-243X Copyright © 2019 International Journal of Biodiversity and Author(s) retain the copyright of this article http://www.academicjournals.org/IJBC Conservation Review The dynamics of medicinal plants utilization practice nexus its health and economic role in Ethiopia: A review paper Yebirzaf Yeshiwas1*, Esubalew Tadele2 and Workinesh Tiruneh3 1Department of Horticulture, Faculty of College Substitutes, Debre Markos University College of Agriculture and Natural Resources P. O. Box 269, Ethiopia. 2Department of Agricultural Economics, Debre Markos University College of Agriculture and Natural Resources P. O. Box 269, Ethiopia. 3Department of Animal Science, Debre Markos University College of Agriculture and Natural Resources, P. O. Box 269, Ethiopia. Received 24 May, 2018; Accepted 11 October, 2018 Medicinal plants play important roles in human and animals disease treatment. 1000 medicinal plant species are identified and reported in the Ethiopian Flora. They contribute and is more preferable for new drug development. Ethiopia has the potential to become an important source country, given the diversity of plants and the rich traditional knowledge regarding their use. The main sources of medicinal plants for utilizers are the wild forests. There is also cultivation practice of medicinal plants in home garden. About 80% of human and 90% of livestock population in Ethiopia depends on utilization of medicinal plants for primary health care. The knowledge transfer of medicinal plants in Ethiopia is largely oral. Most parts of medicinal plants commonly used are leaves and roots. Utilization of leaves for drug preparation is important for conservation of medicinal plants since harvesting leaves may not cause detrimental effect on the plants compared to the root or whole plant collections. -

Oromia Region Administrative Map(As of 27 March 2013)
ETHIOPIA: Oromia Region Administrative Map (as of 27 March 2013) Amhara Gundo Meskel ! Amuru Dera Kelo ! Agemsa BENISHANGUL ! Jangir Ibantu ! ! Filikilik Hidabu GUMUZ Kiremu ! ! Wara AMHARA Haro ! Obera Jarte Gosha Dire ! ! Abote ! Tsiyon Jars!o ! Ejere Limu Ayana ! Kiremu Alibo ! Jardega Hose Tulu Miki Haro ! ! Kokofe Ababo Mana Mendi ! Gebre ! Gida ! Guracha ! ! Degem AFAR ! Gelila SomHbo oro Abay ! ! Sibu Kiltu Kewo Kere ! Biriti Degem DIRE DAWA Ayana ! ! Fiche Benguwa Chomen Dobi Abuna Ali ! K! ara ! Kuyu Debre Tsige ! Toba Guduru Dedu ! Doro ! ! Achane G/Be!ret Minare Debre ! Mendida Shambu Daleti ! Libanos Weberi Abe Chulute! Jemo ! Abichuna Kombolcha West Limu Hor!o ! Meta Yaya Gota Dongoro Kombolcha Ginde Kachisi Lefo ! Muke Turi Melka Chinaksen ! Gne'a ! N!ejo Fincha!-a Kembolcha R!obi ! Adda Gulele Rafu Jarso ! ! ! Wuchale ! Nopa ! Beret Mekoda Muger ! ! Wellega Nejo ! Goro Kulubi ! ! Funyan Debeka Boji Shikute Berga Jida ! Kombolcha Kober Guto Guduru ! !Duber Water Kersa Haro Jarso ! ! Debra ! ! Bira Gudetu ! Bila Seyo Chobi Kembibit Gutu Che!lenko ! ! Welenkombi Gorfo ! ! Begi Jarso Dirmeji Gida Bila Jimma ! Ketket Mulo ! Kersa Maya Bila Gola ! ! ! Sheno ! Kobo Alem Kondole ! ! Bicho ! Deder Gursum Muklemi Hena Sibu ! Chancho Wenoda ! Mieso Doba Kurfa Maya Beg!i Deboko ! Rare Mida ! Goja Shino Inchini Sululta Aleltu Babile Jimma Mulo ! Meta Guliso Golo Sire Hunde! Deder Chele ! Tobi Lalo ! Mekenejo Bitile ! Kegn Aleltu ! Tulo ! Harawacha ! ! ! ! Rob G! obu Genete ! Ifata Jeldu Lafto Girawa ! Gawo Inango ! Sendafa Mieso Hirna -

Administrative Region, Zone and Woreda Map of Oromia a M Tigray a Afar M H U Amhara a Uz N M
35°0'0"E 40°0'0"E Administrative Region, Zone and Woreda Map of Oromia A m Tigray A Afar m h u Amhara a uz N m Dera u N u u G " / m r B u l t Dire Dawa " r a e 0 g G n Hareri 0 ' r u u Addis Ababa ' n i H a 0 Gambela m s Somali 0 ° b a K Oromia Ü a I ° o A Hidabu 0 u Wara o r a n SNNPR 0 h a b s o a 1 u r Abote r z 1 d Jarte a Jarso a b s a b i m J i i L i b K Jardega e r L S u G i g n o G A a e m e r b r a u / K e t m uyu D b e n i u l u o Abay B M G i Ginde e a r n L e o e D l o Chomen e M K Beret a a Abe r s Chinaksen B H e t h Yaya Abichuna Gne'a r a c Nejo Dongoro t u Kombolcha a o Gulele R W Gudetu Kondole b Jimma Genete ru J u Adda a a Boji Dirmeji a d o Jida Goro Gutu i Jarso t Gu J o Kembibit b a g B d e Berga l Kersa Bila Seyo e i l t S d D e a i l u u r b Gursum G i e M Haro Maya B b u B o Boji Chekorsa a l d Lalo Asabi g Jimma Rare Mida M Aleltu a D G e e i o u e u Kurfa Chele t r i r Mieso m s Kegn r Gobu Seyo Ifata A f o F a S Ayira Guliso e Tulo b u S e G j a e i S n Gawo Kebe h i a r a Bako F o d G a l e i r y E l i Ambo i Chiro Zuria r Wayu e e e i l d Gaji Tibe d lm a a s Diga e Toke n Jimma Horo Zuria s e Dale Wabera n a w Tuka B Haru h e N Gimbichu t Kutaye e Yubdo W B Chwaka C a Goba Koricha a Leka a Gidami Boneya Boshe D M A Dale Sadi l Gemechis J I e Sayo Nole Dulecha lu k Nole Kaba i Tikur Alem o l D Lalo Kile Wama Hagalo o b r Yama Logi Welel Akaki a a a Enchini i Dawo ' b Meko n Gena e U Anchar a Midega Tola h a G Dabo a t t M Babile o Jimma Nunu c W e H l d m i K S i s a Kersana o f Hana Arjo D n Becho A o t -

The Role of Community Radio for Integrated and Sustainable Development in Ethiopia: a Critical Review on the Holistic Approach D
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 10 December 2020 doi:10.20944/preprints202012.0260.v1 The Role of Community Radio for Integrated and Sustainable Development in Ethiopia: A Critical Review on the Holistic Approach Destaw Bayable Yemer Guna Tana Integrated Field Research & Development Center, Debre Tabor University, Ethiopia Email: [email protected] Abstract Community radios play a paramount role in the development of the community. Community radio stations have been highly engaged in addressing social, economic, cultural, educational, health, environmental, sanitation, and disaster issues effectively and strategically using local languages in context. Community radios are also used to express, and share indigenous views, thoughts, ideas, problems, and perspectives of local people. The purpose of this analysis is to explore the role of community radio for integrated and sustainable development in Ethiopia. It used a systematic narrative review. Nine research works and five assessments report were selected purposively and analyzed in a quantitative approach. Currently, in Ethiopia, there are 50 community radio stations that received broadcast licenses from Ethiopian Broadcast Authority with four types of licensing and broadcasting in 29 local languages. Community radio helps the community to identify their common goals, create holistic plans, monitor the progress of their developmental activities, and guide on sustainable development. It contributes to integrated and sustainable development in a collaborative and creative process that cultivates the social, economic, and political conditions needed for the community to succeed which aimed to improve and sustain the livelihoods of the community. However, the media can’t achieve its target goal to support the development activities and bring holistic development of the community. -

Ethnobotanical Study of Traditional Medicinal Plants in and Around Fiche District, Central Ethiopia
Current Research Journal of Biological Sciences 6(4): 154-167, 2014 ISSN: 2041-076X, e-ISSN: 2041-0778 © Maxwell Scientific Organization, 2014 Submitted: December 13, 2013 Accepted: December 20, 2013 Published: July 20, 2014 Ethnobotanical Study of Traditional Medicinal Plants in and Around Fiche District, Central Ethiopia 1Abiyu Enyew, 2Zemede Asfaw, 2Ensermu Kelbessa and 1Raja Nagappan 1Department of Biology, College of Natural and Computational Sciences, University of Gondar, Post Box 196, Gondar, 2Department of Plant Biology and Biodiversity Management, College of Natural Sciences, Addis Ababa University, Post Box 3434, Addis Ababa, Ethiopia Abstract: An ethnobotanical study of medicinal plants was conducted in and around Fiche District, North Shewa Zone of Oromia Region, Ethiopia from September 2011 to January 2012. Ten kebeles were selected from North to South and East to West directions of Fiche District and its surroundings by purposive sampling method. Six informants including one key informant were selected from each kebele for data collection by using printed data collection sheets containing, semi-structured interview questions, group discussion and guided field walk. The plant specimens were identified by using taxonomic keys in the Floras of Ethiopia and Eritrea. The data were analysed using descriptive statistics; informant consensus factor and fidelity level using MS-Excel 2010. Totally, 155 medicinal plants belonging to 128 genera and 65 families were recorded. Most medicinal plants (72.9%) were used for human healthcare in which Lamiaceae was dominant (11%) in which Ocimum lamiifolium, Otostegia integrifolia and Leonotis ocymifolia were the most common species. Herbs were dominant (43.87%) flora followed by shrubs (35.48%). -

Ethiopia: Administrative Map (August 2017)
Ethiopia: Administrative map (August 2017) ERITREA National capital P Erob Tahtay Adiyabo Regional capital Gulomekeda Laelay Adiyabo Mereb Leke Ahferom Red Sea Humera Adigrat ! ! Dalul ! Adwa Ganta Afeshum Aksum Saesie Tsaedaemba Shire Indasilase ! Zonal Capital ! North West TigrayTahtay KoraroTahtay Maychew Eastern Tigray Kafta Humera Laelay Maychew Werei Leke TIGRAY Asgede Tsimbila Central Tigray Hawzen Medebay Zana Koneba Naeder Adet Berahile Region boundary Atsbi Wenberta Western Tigray Kelete Awelallo Welkait Kola Temben Tselemti Degua Temben Mekele Zone boundary Tanqua Abergele P Zone 2 (Kilbet Rasu) Tsegede Tselemt Mekele Town Special Enderta Afdera Addi Arekay South East Ab Ala Tsegede Mirab Armacho Beyeda Woreda boundary Debark Erebti SUDAN Hintalo Wejirat Saharti Samre Tach Armacho Abergele Sanja ! Dabat Janamora Megale Bidu Alaje Sahla Addis Ababa Ziquala Maychew ! Wegera Metema Lay Armacho Wag Himra Endamehoni Raya Azebo North Gondar Gonder ! Sekota Teru Afar Chilga Southern Tigray Gonder City Adm. Yalo East Belesa Ofla West Belesa Kurri Dehana Dembia Gonder Zuria Alamata Gaz Gibla Zone 4 (Fantana Rasu ) Elidar Amhara Gelegu Quara ! Takusa Ebenat Gulina Bugna Awra Libo Kemkem Kobo Gidan Lasta Benishangul Gumuz North Wello AFAR Alfa Zone 1(Awsi Rasu) Debre Tabor Ewa ! Fogera Farta Lay Gayint Semera Meket Guba Lafto DPubti DJIBOUTI Jawi South Gondar Dire Dawa Semen Achefer East Esite Chifra Bahir Dar Wadla Delanta Habru Asayita P Tach Gayint ! Bahir Dar City Adm. Aysaita Guba AMHARA Dera Ambasel Debub Achefer Bahirdar Zuria Dawunt Worebabu Gambela Dangura West Esite Gulf of Aden Mecha Adaa'r Mile Pawe Special Simada Thehulederie Kutaber Dangila Yilmana Densa Afambo Mekdela Tenta Awi Dessie Bati Hulet Ej Enese ! Hareri Sayint Dessie City Adm. -

Anticipated Humanitarian Requirement for Water, Sanitation
1 TABLE OF CONTENTS ACRONYMS/GLOSSARY ......................................................................................... 1 EXECUTIVE SUMMARY ......................................................................................... 2 1. INTRODUCTION AND BACKGROUND ........................................................... 3 1.1. 2014 ANNUAL HUMANITARIAN REQUIREMENTS DOCUMENT ........................................................................... 3 1.2. HUMANITARIAN SITUATION OVERVIEW ........................................................................................................... 3 2. REVIEW OF THE SECOND HALF OF THE 2013 HUMANITARIAN RESPONSE ................................................................................................................... 6 2.1RELIEF FOOD AND TSF .............................................................................................................................................. 6 2.2 HEALTH AND NUTRITION ...................................................................................................................................... 8 2.3 WATER, SANITATION AND HYGIENE (WASH) .................................................................................................... 12 2.4 AGRICULTURE ..................................................................................................................................................... 14 2.5 EDUCATION ........................................................................................................................................................ -

HIGHLIGHTS in THIS ISSUE: Harvest Is Anticipated in the Highland and Midland Woredas • REGIONAL OVERVIEW of the Region
FOCUS ON ETHIOPIA PAGE 1 slaughtering of milking cows. Meanwhile, good meher HIGHLIGHTS IN THIS ISSUE: harvest is anticipated in the highland and midland woredas • REGIONAL OVERVIEW of the region. • NEWS: - POOR RAIN FORECASTS SUGGEST … - NEW NATIONAL NUTRITION STRATEGY Serious shortage of water and pasture is reported in Dillo, • UPCOMING & ONGOING MEETINGS Miyo, Dire, Dhas, Moyale, Teltele, Arero, and Yabello woredas in Borena zone; Liben woreda in Guji zone and 56 kebeles in various woredas of East Hararghe zone. The Focus on Ethiopia is produced by UN Office for the Coordination of Humanitarian Affairs (OCHA), in situation is severe in Dire woreda. Most of the ponds and collaboration with other UN agencies and partner NGOs. cisterns have dried and the yield of traditional wla/wells has Focus on Ethiopia provides a monthly overview of decreased. Most hand pumps, motorized units, and humanitarian trends and activities in Ethiopia, as well as boreholes require immediate rehabilitation. Pasture focusing on particular issues of interest. Send comments, reserves in Borena zone are over grazed, resulting in suggestions and contributions to [email protected] unusual livestock migration. Influx of herds from neighboring Somali Region aggravated the situation. Some schools are reportedly closed and dropout rates have increased, according to a joint assessment undertaken in REGIONAL OVERVIEW early January 2008. In addition, locust infestation in Bale, Borena and East Hararghe zones is damaging vegetation. OROMIYA The food security situation in the lowland woredas of As a result the physical condition of livestock deteriorated Borena, Guji, Bale, Arsi, East and West Hararghe zones is of and deaths of cattle is being reported. -
Dictionary of Cultivated Plants and Their Regions of Diversity Second Edition Revised Of: A.C
Dictionary of cultivated plants and their regions of diversity Second edition revised of: A.C. Zeven and P.M. Zhukovsky, 1975, Dictionary of cultivated plants and their centres of diversity 'N -'\:K 1~ Li Dictionary of cultivated plants and their regions of diversity Excluding most ornamentals, forest trees and lower plants A.C. Zeven andJ.M.J, de Wet K pudoc Centre for Agricultural Publishing and Documentation Wageningen - 1982 ~T—^/-/- /+<>?- •/ CIP-GEGEVENS Zeven, A.C. Dictionary ofcultivate d plants andthei rregion so f diversity: excluding mostornamentals ,fores t treesan d lowerplant s/ A.C .Zeve n andJ.M.J ,d eWet .- Wageninge n : Pudoc. -11 1 Herz,uitg . van:Dictionar y of cultivatedplant s andthei r centreso fdiversit y /A.C .Zeve n andP.M . Zhukovsky, 1975.- Me t index,lit .opg . ISBN 90-220-0785-5 SISO63 2UD C63 3 Trefw.:plantenteelt . ISBN 90-220-0785-5 ©Centre forAgricultura l Publishing and Documentation, Wageningen,1982 . Nopar t of thisboo k mayb e reproduced andpublishe d in any form,b y print, photoprint,microfil m or any othermean swithou t written permission from thepublisher . Contents Preface 7 History of thewor k 8 Origins of agriculture anddomesticatio n ofplant s Cradles of agriculture and regions of diversity 21 1 Chinese-Japanese Region 32 2 Indochinese-IndonesianRegio n 48 3 Australian Region 65 4 Hindustani Region 70 5 Central AsianRegio n 81 6 NearEaster n Region 87 7 Mediterranean Region 103 8 African Region 121 9 European-Siberian Region 148 10 South American Region 164 11 CentralAmerica n andMexica n Region 185 12 NorthAmerica n Region 199 Specieswithou t an identified region 207 References 209 Indexo fbotanica l names 228 Preface The aimo f thiswor k ist ogiv e thereade r quick reference toth e regionso f diversity ofcultivate d plants.Fo r important crops,region so fdiversit y of related wild species areals opresented .Wil d species areofte nusefu l sources of genes to improve thevalu eo fcrops . -

ETHIOPIA Food Security Outlook January to June 2011
ETHIOPIA Food Security Outlook January to June 2011 Following the meher harvest, which began in October Figure 1. Current estimated food security outcomes, 2010, food security has generally improved in the January 2011 meher producing parts of the country. However, due to crop damage caused by widespread floods and other weather related shocks the meher harvest is likely to be lower than initially anticipated. The Humanitarian Requirement Documents outlining assistance needs is expected to be released in February 2011. Although the National Meteorology Agency has not provided a forecast for the April to June gu/genna/belg rains, below normal performance of these rains is considered likely. This is expected to exacerbate prevailing food insecurity which resulted from near complete failure of October to December rains in southern pastoral and agro pastoral areas. Due to close to normal sapie (December/January) 2010 rains food security among the dominant root crop, For more information on FEWS NET’s Food Insecurity Severity Scale, please see: www.fews.net/FoodInsecurityScale mainly sweet potatoes growing areas in central and eastern SNNPR is estimated to remain stable Source: FEWS NET and WFP throughout the outlook period. The poor and very poor households normally rely on these harvests, during the March to May lean season. Staple food prices are likely to follow typical seasonal trends throughout the outlook period, though remain higher than the 2005 to 2009 averages given the current harvest and the continued price stabilization measures taken by the government. Seasonal calendar and critical events Source: FEWS NET FEWS NET Washington FEWS NET Ethiopia FEWS NET is a USAID-funded activity.